Understanding the complexities of the human nervous system is crucial for anyone preparing for a clinical evaluation in this field. Mastering the fundamental concepts, along with the ability to apply them in real-world scenarios, is key to success. The topics covered in this section will provide a comprehensive overview to guide your preparation and enhance your knowledge base.
In-depth knowledge of the brain, spinal cord, and peripheral nerves is often tested, with a focus on recognizing symptoms, diagnosing conditions, and understanding treatment options. This section will equip you with practical tools and insights to approach challenges with confidence.
Through focused practice and understanding, you can refine your ability to respond to complex case studies, interpret diagnostic data, and showcase a clear grasp of neurological functions. Whether you are a student or professional, preparing effectively will help solidify your expertise in this vital area of healthcare.
Key Concepts and Practice Scenarios
Mastering the field of neurology requires a solid foundation in its core principles. This section focuses on common challenges you may face during evaluations, offering a blend of theoretical knowledge and practical applications. Understanding the relationship between symptoms, diagnoses, and treatment options is essential to navigating this area with confidence.
Core Areas to Focus On
Reviewing vital topics such as nervous system functions, disease mechanisms, and clinical observations will help you gain a clearer understanding. Below is a list of critical areas to examine, designed to test your grasp of key concepts.
| Topic | Focus Area | Importance |
|---|---|---|
| Brain and Spinal Cord | Understanding structure and function | Fundamental to diagnosing neurological disorders |
| Motor and Sensory Pathways | Key in identifying movement disorders | Critical for clinical evaluations |
| Reflexes and Responses | Evaluating nervous system activity | Essential for assessing neurological integrity |
| Diagnostic Tools | Interpreting tests like MRIs and CT scans | Helps confirm suspicions and guide treatment |
Practical Scenarios
Familiarity with common clinical situations is necessary for any professional in the field. Being able to respond effectively to hypothetical cases or patient histories will allow you to demonstrate both theoretical knowledge and clinical reasoning. Practice and critical thinking are essential in refining your approach to such challenges.
Key Concepts in Neurology
Understanding the fundamental principles of the nervous system is essential for anyone studying or working in the field of clinical care. The intricacies of the brain, spinal cord, and peripheral nerves form the backbone of diagnosing various conditions. A strong grasp of how these components interact, as well as the mechanisms behind their functions, is necessary to make informed decisions and provide effective treatments.
Essential topics include the structure of the central and peripheral systems, how signals are transmitted, and the various disorders that can disrupt these processes. By mastering these key concepts, you will be better equipped to identify symptoms, understand their causes, and respond with appropriate interventions.
Core areas like sensory perception, motor control, reflexes, and cognition are central to this field. Each area provides unique insights into the overall functioning of the body, making it crucial to understand both the individual components and their interconnectedness. This foundational knowledge allows for more accurate assessments and better clinical judgment.
Common Disorders Tested in Assessments
During clinical evaluations, it is crucial to have a deep understanding of various conditions that affect the nervous system. These disorders often present with distinct symptoms that require careful analysis to diagnose accurately. Knowledge of the most common diseases and conditions, including their causes, symptoms, and treatment options, is essential for any healthcare professional working in this field.
Frequently Encountered Conditions
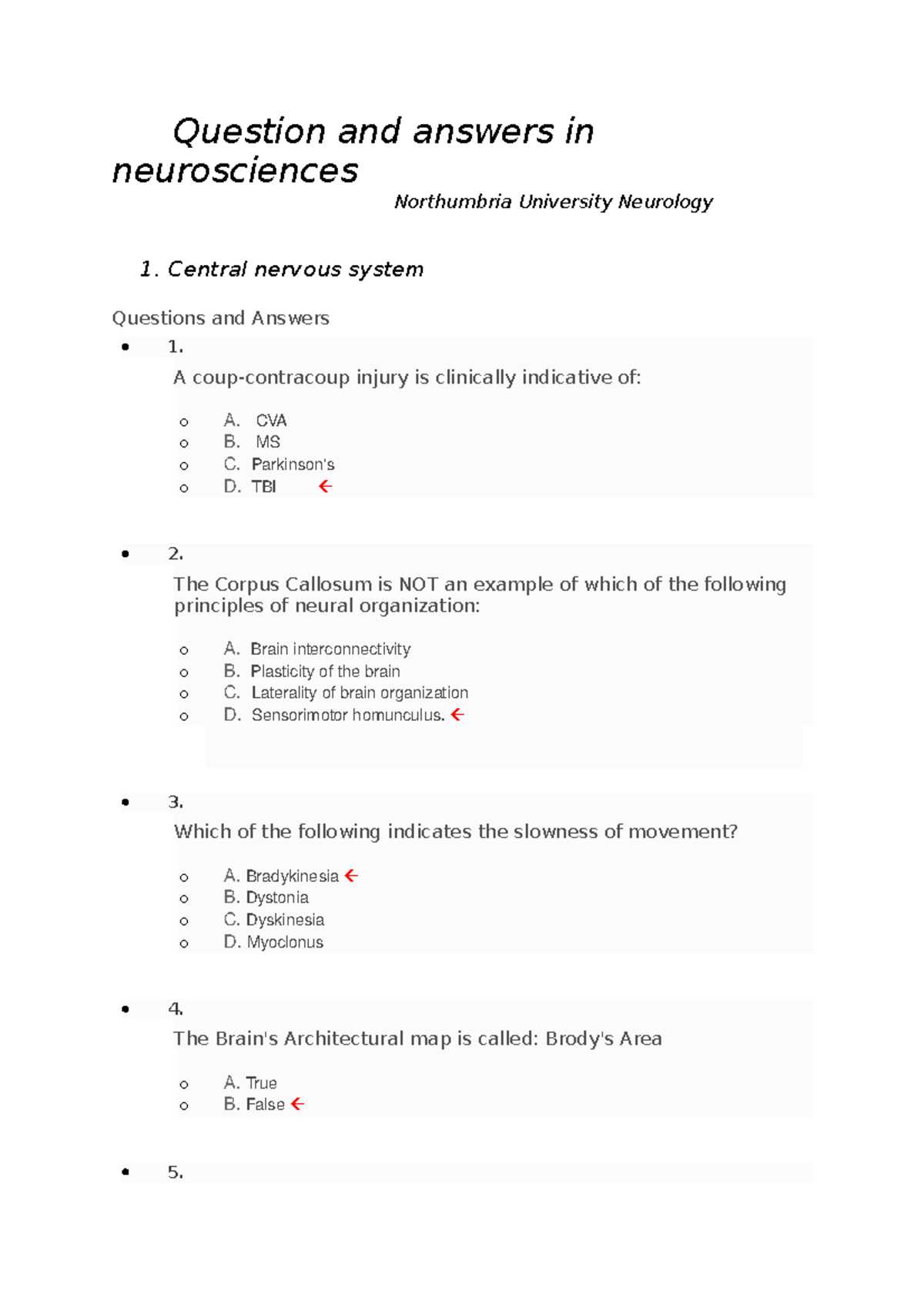
Several disorders are regularly tested due to their prevalence and impact on daily functioning. Below is a list of conditions that are important to study, each highlighting different aspects of the nervous system.
| Disorder | Key Features | Symptoms |
|---|---|---|
| Parkinson’s Disease | Degeneration of motor neurons | Tremors, rigidity, bradykinesia |
| Multiple Sclerosis | Immune system attacks myelin | Muscle weakness, visual disturbances, fatigue |
| Alzheimer’s Disease | Progressive cognitive decline | Memory loss, confusion, personality changes |
| Epilepsy | Recurrent seizures | Convulsions, loss of consciousness |
| Stroke | Interruption of blood flow to the brain | Weakness, speech difficulties, paralysis |
Understanding the Symptoms
Recognizing the symptoms of these disorders is vital for providing effective care. Early detection and accurate diagnosis often lead to better outcomes, making it essential for healthcare providers to stay informed about the latest diagnostic tools and treatments available for these common conditions.
Understanding Neuroanatomy for Success
To succeed in clinical assessments, a comprehensive understanding of the structure and function of the nervous system is essential. Familiarity with the brain, spinal cord, and peripheral nerves forms the foundation of neurological evaluations. By knowing how these components interact, you can effectively interpret symptoms and devise appropriate treatment plans.
Key concepts include the roles of different brain regions, the pathways through which information is transmitted, and the way sensory and motor functions are coordinated. This knowledge helps clinicians make informed decisions and understand the underlying causes of various disorders.
Moreover, understanding the anatomical layout enables you to recognize when things go wrong, which is critical in diagnosing conditions that may present with subtle or complex signs. Mastery of these basic principles will not only enhance your clinical acumen but also improve your ability to apply theoretical knowledge to practical situations.
Key Concepts in Physiology You Should Know
Having a deep understanding of how the nervous system functions at a physiological level is critical for assessing various conditions. The principles governing signal transmission, nerve function, and the communication between different parts of the body provide essential insights for diagnosis and treatment. Mastering these concepts will not only enhance your theoretical knowledge but also sharpen your ability to evaluate clinical cases.
Below are several key areas that are crucial to grasp in order to excel in clinical practice:
- Resting Membrane Potential: Understanding the difference between intra- and extracellular ion concentrations and how they contribute to the resting state of neurons.
- Action Potential: The process by which electrical impulses travel along neurons, including depolarization, repolarization, and the role of ion channels.
- Synaptic Transmission: The release of neurotransmitters and how signals are passed between neurons at synapses.
- Neurotransmitters: The chemical messengers that facilitate communication within the nervous system and their impact on various functions.
- Reflex Arcs: The pathway through which sensory information is processed, leading to a motor response, critical for understanding rapid reactions in the body.
Being familiar with these physiological processes will give you a solid foundation for recognizing how disruptions can lead to various disorders. Understanding these mechanisms is fundamental for diagnosing conditions that arise from abnormal nerve functions or impaired signal transmission.
Clinical Scenarios for Neurology Assessments
In clinical practice, it is essential to be prepared for real-world scenarios that test both theoretical knowledge and the ability to apply it to patient care. These situations often involve identifying symptoms, making diagnoses, and selecting appropriate treatments based on the information presented. Analyzing case studies and practical examples can help develop the critical thinking skills necessary for accurate decision-making.
Common Case Scenarios
Several scenarios frequently appear in clinical settings, highlighting different aspects of nervous system disorders. These situations require a blend of observation, diagnosis, and management skills. Here are some common case types that often arise:
- Motor Dysfunction: A patient presents with muscle weakness or paralysis. Understanding the underlying cause, whether it’s a stroke, spinal injury, or degenerative disorder, is crucial.
- Sensory Abnormalities: Cases where patients report numbness, tingling, or loss of sensation. Recognizing patterns related to nerve damage, neuropathy, or systemic conditions is vital for proper treatment.
- Seizure Disorders: A case involving episodes of convulsions or loss of consciousness. Determining the type of seizure, whether focal or generalized, and understanding potential triggers helps guide management.
- Headaches and Migraines: A patient describes recurrent or severe headaches. The ability to differentiate between primary and secondary causes, such as tension headaches, migraines, or more serious conditions like tumors, is essential.
Approach to Diagnosis
In each clinical scenario, it is important to approach the case systematically. This involves taking a thorough patient history, performing physical and neurological exams, and utilizing diagnostic tools such as imaging or lab tests. An accurate diagnosis hinges on integrating all available information, including patient symptoms, medical history, and test results.
Diagnostic Techniques in Neurology
Accurate diagnosis of neurological conditions requires a combination of clinical assessment and advanced diagnostic tools. Understanding how to apply these techniques effectively allows clinicians to detect disorders that may otherwise remain hidden. Each tool plays a unique role in revealing underlying issues within the nervous system, whether through imaging, electrical testing, or fluid analysis.
The right diagnostic approach ensures timely intervention, which is critical for improving patient outcomes. Below is a summary of the most commonly used diagnostic methods in the field:
| Technique | Purpose | Common Uses |
|---|---|---|
| Magnetic Resonance Imaging (MRI) | Detailed imaging of the brain and spinal cord | Identifying tumors, strokes, multiple sclerosis |
| Computed Tomography (CT) | Rapid imaging for acute conditions | Evaluating hemorrhages, trauma, and tumors |
| Electroencephalography (EEG) | Recording brain electrical activity | Diagnosing epilepsy, sleep disorders, encephalopathies |
| Electromyography (EMG) | Assessing electrical activity in muscles | Diagnosing muscle disorders, nerve injuries |
| Lumbar Puncture | Collection of cerebrospinal fluid (CSF) | Testing for infections, bleeding, and inflammatory diseases |
Each of these diagnostic tools provides valuable insights into different aspects of neurological health. By mastering the use of these techniques, healthcare professionals can confidently identify, assess, and manage a wide range of conditions affecting the nervous system.
Neuroimaging and Its Relevance
In modern clinical practice, imaging techniques play a pivotal role in diagnosing conditions affecting the nervous system. These technologies provide invaluable insights by creating detailed visual representations of the brain, spinal cord, and peripheral structures. The ability to visualize these areas non-invasively has revolutionized how healthcare providers understand, diagnose, and monitor a wide range of neurological disorders.
Types of Imaging Techniques
There are several types of imaging methods commonly used to assess the nervous system, each serving distinct purposes and offering different levels of detail. Below are the most frequently used imaging techniques:
- Magnetic Resonance Imaging (MRI): This method uses magnetic fields and radio waves to generate detailed images of the brain and spinal cord, making it essential for detecting conditions such as tumors, strokes, and multiple sclerosis.
- Computed Tomography (CT): A CT scan combines multiple X-ray images to create cross-sectional views of the body. It is especially useful for quickly identifying acute issues such as hemorrhages, traumatic injuries, and certain types of strokes.
- Positron Emission Tomography (PET): This imaging technique allows for the observation of metabolic processes within the brain. It is often used to assess conditions like Alzheimer’s disease, tumors, and areas of abnormal brain activity.
Significance in Clinical Practice
The relevance of neuroimaging cannot be overstated. By providing precise and detailed images, these techniques allow clinicians to identify structural changes, monitor disease progression, and plan appropriate interventions. In many cases, they are indispensable for confirming diagnoses, evaluating treatment responses, and predicting outcomes. Additionally, these tools help in differentiating between similar symptoms caused by various underlying disorders, which is critical for tailoring individualized treatment plans.
Tips for Answering Multiple-Choice Questions
When facing assessments that include multiple-choice formats, it is crucial to develop strategies that maximize efficiency and accuracy. These tests often contain several options, with only one correct choice, so it’s important to analyze each one carefully before selecting your response. The key to success lies not just in knowledge, but in applying a structured approach to reading the options and identifying the best answer.
Here are several effective strategies that can help you navigate multiple-choice formats more confidently:
| Tip | Description |
|---|---|
| Read the Question Carefully | Before reviewing the options, ensure you understand the question. Pay attention to keywords, such as “always”, “never”, or “most likely”, which can significantly change the meaning. |
| Eliminate Obvious Wrong Answers | By removing clearly incorrect options, you increase your chances of selecting the correct answer from the remaining choices. |
| Look for Patterns | In some cases, multiple-choice options follow certain patterns, such as using similar terms or concepts. This can help you narrow down choices more efficiently. |
| Trust Your First Instinct | If you’re unsure, your first instinct is often correct. Avoid second-guessing too much, as overthinking can lead to confusion. |
| Check for “All of the Above” or “None of the Above” | If these options are present, review all other choices carefully. “All of the above” is only correct when all individual answers are true, while “None of the above” is correct if none of the options are correct. |
By implementing these strategies, you can improve both the accuracy and efficiency of your responses, giving you a better chance of achieving a strong performance in these types of assessments.
Common Neurological Symptoms to Study
Understanding key symptoms related to nervous system disorders is essential for recognizing and diagnosing various conditions. These signs often manifest in different ways, from physical changes in movement to cognitive impairments, and they can indicate a wide range of underlying issues. Studying these symptoms helps build the foundation for more accurate assessments and better management of patient care.
Key Symptoms to Recognize
Here are some of the most common manifestations that are important to familiarize yourself with:
- Headaches: Frequent or severe headaches can be a sign of several conditions, including migraines, tension headaches, or more serious issues like tumors or aneurysms.
- Dizziness and Vertigo: These can result from a variety of causes, including inner ear issues, strokes, or vestibular disorders.
- Seizures: Sudden, uncontrolled electrical activity in the brain can lead to convulsions or altered awareness, often linked to epilepsy or brain injuries.
- Tremors: Involuntary shaking, commonly associated with Parkinson’s disease, can also occur in other neurological conditions.
- Weakness or Paralysis: These symptoms can point to motor nerve damage, strokes, or spinal cord injuries.
- Memory Loss: Cognitive decline, often seen in conditions like dementia or Alzheimer’s disease, can be an early warning sign of more serious neurological conditions.
- Vision Problems: Blurred vision, double vision, or sudden loss of vision could indicate issues with the brain, optic nerve, or eye-related disorders.
How to Approach These Symptoms
Recognizing these symptoms early on can lead to faster diagnosis and more effective treatment. It’s essential to differentiate between symptoms caused by common, mild issues and those linked to more serious, complex conditions. Familiarity with the presentation of each symptom, as well as their potential causes, can guide further testing and help clinicians make informed decisions regarding treatment plans.
Important Reflexes and Their Significance
Reflexes are automatic, rapid responses to stimuli that play a critical role in protecting the body and maintaining balance. These involuntary actions are controlled by the spinal cord and brainstem, and they provide essential clues about the integrity of the nervous system. Understanding these reflexes is key to diagnosing various neurological conditions, as abnormalities can indicate underlying issues with the central or peripheral nervous systems.
Below are some of the most important reflexes that are commonly tested in clinical practice, along with their significance in evaluating nervous system function:
- Patellar Reflex (Knee-Jerk Reflex): This is one of the most well-known reflexes, tested by tapping the patellar tendon below the knee. A normal response is a quick contraction of the quadriceps muscle, causing the lower leg to kick. This reflex is used to assess the integrity of the L2-L4 spinal nerves.
- Babinski Reflex: In this test, the sole of the foot is stroked, and the response is observed. A normal response in adults is a downward curling of the toes. An abnormal response, such as the upward extension of the big toe, can indicate damage to the corticospinal tract, often seen in conditions like multiple sclerosis or a stroke.
- Achilles Reflex (Ankle-Jerk Reflex): By tapping the Achilles tendon, this reflex is used to assess the S1-S2 spinal nerve roots. A normal response is the contraction of the calf muscle, causing the foot to flex downward. This reflex helps in evaluating the lower motor neurons.
- Corneal Reflex: This reflex is tested by gently touching the cornea with a wisp of cotton, causing a blink in response. It helps assess the function of the trigeminal nerve (cranial nerve V) and the facial nerve (cranial nerve VII).
- Gag Reflex: This reflex is stimulated by touching the back of the throat. A strong gag response indicates normal function of both the glossopharyngeal nerve (cranial nerve IX) and the vagus nerve (cranial nerve X). Its absence can signal a problem in the brainstem.
By observing these reflexes, clinicians can assess both the function and the integrity of the nervous system. Abnormal responses may suggest nerve damage, spinal cord issues, or brain lesions, allowing for targeted diagnostic testing and more accurate treatment planning.
Motor and Sensory Pathways Explained
The body’s ability to move and sense its environment relies on complex networks of nerves that transmit signals between the brain, spinal cord, and peripheral areas. These networks, or pathways, are critical in enabling voluntary movement and the perception of stimuli. Understanding these pathways is essential for diagnosing disorders related to movement and sensation, as disruptions in these systems can result in various neurological symptoms.
Motor and sensory pathways are distinct but interrelated systems. Motor pathways are responsible for sending signals from the brain to muscles, while sensory pathways transmit information from sensory receptors to the brain. Both pathways involve multiple structures, and any damage along the route can impact normal function.
Motor Pathways
Motor pathways control voluntary muscle movements. The primary motor pathway consists of the corticospinal tract, which begins in the motor cortex of the brain. These signals travel down the spinal cord and synapse with lower motor neurons that ultimately stimulate muscles. Damage to this pathway can lead to weakness, paralysis, or other motor deficits.
- Corticospinal Tract: This is the primary pathway responsible for voluntary movement. It controls fine motor skills and movement coordination.
- Extrapyramidal Pathways: These pathways help regulate muscle tone and involuntary movements, playing a crucial role in maintaining posture and balance.
- Cerebellar Pathways: These pathways are involved in the coordination of voluntary movements and the maintenance of balance. Damage to the cerebellum can lead to ataxia, or uncoordinated movement.
Sensory Pathways
Sensory pathways are responsible for transmitting sensory information, such as touch, pain, temperature, and proprioception, from the body to the brain. The primary sensory pathways include the spinothalamic tract and the dorsal column-medial lemniscal pathway. These pathways enable the brain to process and interpret sensory input, allowing for a coordinated response to environmental stimuli.
- Spinothalamic Tract: This pathway transmits sensations of pain, temperature, and crude touch from the body to the brain.
- Dorsal Column-Medial Lemniscal Pathway: This pathway is responsible for transmitting fine touch, vibration, and proprioception (awareness of body position).
- Trigeminothalamic Tract: This pathway transmits sensory information from the face, allowing for the perception of touch, pain, and temperature.
Both motor and sensory pathways are essential for everyday functioning. Damage to these pathways can lead to a wide variety of symptoms, ranging from difficulty moving or perceiving sensations to more severe impairments in coordination and balance. Understanding how these pathways work and where they may be affected is key to diagnosing and treating many neurological conditions.
Neuropharmacology and Treatment Questions
Understanding the interaction between medications and the nervous system is crucial for the effective treatment of neurological disorders. The study of how drugs affect brain function and the pathways involved in various conditions helps guide treatment strategies. Knowledge in this field is essential for selecting appropriate therapies that can improve patient outcomes and manage symptoms effectively.
Pharmacological treatments for neurological conditions involve various classes of drugs that target specific aspects of the nervous system. These treatments aim to modify neurotransmitter activity, alter synaptic transmission, or protect neurons from further damage. It’s vital to understand the mechanisms of these drugs, their potential side effects, and their role in treating different conditions.
Key Drug Classes in Neurological Treatments
- Antidepressants: These drugs are commonly used to treat mood disorders, including depression and anxiety. They work by altering levels of neurotransmitters such as serotonin and norepinephrine, which help regulate mood and emotional responses.
- Anticonvulsants: Medications that help control seizures by stabilizing electrical activity in the brain. They are essential for managing epilepsy and other seizure-related disorders.
- Antipsychotics: These drugs are used to treat conditions like schizophrenia and bipolar disorder by modulating the activity of neurotransmitters like dopamine, which is often involved in psychotic symptoms.
- Parkinson’s Disease Medications: These include drugs like levodopa, which increase dopamine levels in the brain, helping to manage symptoms of Parkinson’s disease such as tremors and rigidity.
- Multiple Sclerosis Medications: These drugs aim to manage inflammation and slow the progression of the disease. Immunomodulatory drugs are often prescribed to reduce the frequency and severity of relapses.
Considerations in Treatment Selection
When selecting treatments for neurological disorders, several factors must be considered, including the specific diagnosis, the patient’s overall health, and the potential side effects of the medication. For example, while certain medications may be effective for managing symptoms, they may also have adverse effects that must be closely monitored.
- Side Effect Profiles: Some treatments come with significant side effects, such as drowsiness, weight gain, or gastrointestinal issues. Choosing the right medication requires weighing the benefits against these potential downsides.
- Drug Interactions: Many neurological drugs interact with other medications, which could affect their efficacy or cause harmful reactions. It’s essential to evaluate the patient’s full medication list to avoid dangerous combinations.
- Patient Compliance: The effectiveness of a treatment depends not only on its pharmacological properties but also on how well the patient adheres to the prescribed regimen. Factors such as pill burden and frequency of dosing can impact adherence.
In addition to medications, non-pharmacological treatments like physical therapy, cognitive therapy, and lifestyle changes can play a critical role in managing neurological conditions. A comprehensive treatment plan should take all these factors into account to provide the most effective care.
How to Interpret Neurological Tests
Interpreting the results of diagnostic tests related to the nervous system requires a thorough understanding of both normal and abnormal findings. These tests provide valuable insights into the functioning of the brain, spinal cord, and peripheral nervous system. By analyzing the data obtained from various procedures, healthcare professionals can form a clearer picture of the patient’s condition and guide treatment decisions accordingly.
In order to accurately assess test results, it is essential to consider several factors. These include the type of test conducted, the patient’s medical history, and any presenting symptoms. A comprehensive approach to interpretation can help identify the underlying cause of neurological issues, whether they are acute, chronic, or related to systemic conditions.
Common Types of Neurological Tests
- Magnetic Resonance Imaging (MRI): This imaging technique provides detailed images of the brain and spinal cord, allowing physicians to identify structural abnormalities such as tumors, lesions, or plaques. The interpretation of MRI scans involves analyzing tissue density, as well as the presence of any abnormal growths or damage to neural structures.
- Electroencephalogram (EEG): This test measures electrical activity in the brain. The results are used to identify conditions like epilepsy, sleep disorders, and certain types of brain damage. Interpreting an EEG involves recognizing patterns of brain waves that deviate from the normal range, which can suggest specific types of neurological disorders.
- Computed Tomography (CT) Scan: CT scans provide cross-sectional images of the brain, helping detect bleeding, strokes, or fractures. In interpreting CT scans, radiologists focus on identifying areas of abnormal density that may indicate acute changes in the brain.
- Electromyography (EMG): This test assesses the electrical activity of muscles and the nerve cells that control them. Abnormal results can indicate issues with nerve function or muscle disorders. Interpretation focuses on the presence of electrical abnormalities during muscle contractions.
- Lumbar Puncture (Spinal Tap): This procedure involves collecting cerebrospinal fluid (CSF) from around the spinal cord. It is commonly used to diagnose infections, inflammation, and conditions like multiple sclerosis. Interpreting CSF involves assessing protein levels, cell counts, and the presence of pathogens.
Key Considerations When Interpreting Results
When reviewing neurological test results, it is crucial to take a holistic approach. While individual test results can provide valuable insights, they must always be interpreted in conjunction with clinical signs and patient history. This ensures that the diagnosis is both accurate and comprehensive.
- Patient History: Understanding the patient’s medical background, including any previous neurological conditions or family history, is critical in interpreting test results. This context helps to identify whether a condition is hereditary, progressive, or triggered by an external factor.
- Symptom Correlation: The results of a test are more meaningful when correlated with the patient’s symptoms. For instance, if a patient experiences numbness in a particular part of the body, an MRI showing a lesion in the corresponding area of the brain or spinal cord is more likely to be significant.
- Variability in Test Results: Some neurological tests may yield results that are within the normal range, but still suggest underlying issues when combined with other findings. A low-level abnormality in one test may not be significant on its own, but if it coincides with other signs, it may warrant further investigation.
Ultimately, accurate interpretation requires expertise and careful consideration of all available information. While tests can provide essential data, the clinical context in which they are used remains crucial for a successful diagnosis and treatment plan.
Neurological Assessment in Clinical Practice
Assessing the function of the nervous system is a fundamental component of patient care, crucial for diagnosing a wide range of conditions. This evaluation involves systematically checking the functioning of the brain, spinal cord, and peripheral systems. A thorough examination allows clinicians to identify abnormalities, track changes over time, and tailor treatment plans accordingly.
In clinical practice, this assessment is essential not only for detecting disorders but also for monitoring progress and adjusting therapeutic approaches. The process usually includes a combination of observational skills, physical examination, and specialized tests. Each step is aimed at revealing any signs of dysfunction, such as impaired movement, sensation, or cognition.
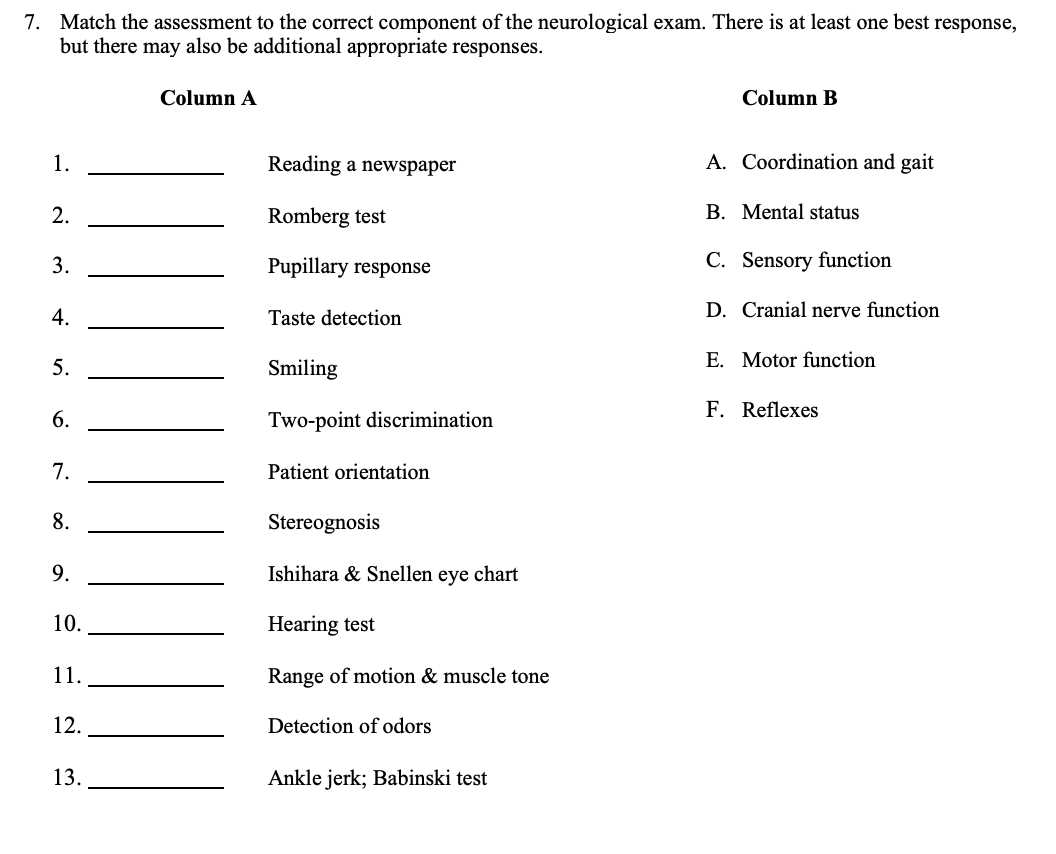
Key Components of a Neurological Assessment
- Patient History: A detailed review of the patient’s symptoms, medical history, and any risk factors is the foundation of the assessment. Understanding the onset, duration, and progression of symptoms can provide vital clues about the underlying condition.
- Mental Status: Evaluating cognitive function is critical in identifying conditions such as dementia, stroke, or encephalopathy. This includes testing memory, attention, language, and executive functions.
- Motor Function: Assessment of muscle strength, coordination, and movement patterns helps identify motor deficits or signs of neurological disorders such as Parkinson’s disease or multiple sclerosis.
- Sensory Function: Evaluating sensory pathways, including touch, temperature, pain, and proprioception, is essential for detecting nerve damage or central nervous system dysfunction.
- Reflexes: Testing deep tendon reflexes and other involuntary movements helps to assess the integrity of the spinal cord and nerve pathways.
Interpreting Results and Developing a Plan
Once the examination is complete, interpreting the findings is essential for determining the course of action. Clinicians look for patterns of abnormal results that correlate with specific conditions. In many cases, the assessment is only the first step, with further tests or imaging required to confirm the diagnosis.
- Clinical Correlation: It’s essential to consider the context in which the symptoms occur. Age, pre-existing conditions, and the patient’s overall health can affect the significance of certain findings.
- Referral for Further Testing: If the assessment points to a specific disorder, further diagnostic testing, such as imaging or lab work, may be necessary to confirm the condition.
- Monitoring Over Time: Neurological assessments are not always conclusive after a single visit. Regular monitoring is often required, especially in progressive disorders like multiple sclerosis or Alzheimer’s disease.
In summary, a thorough evaluation of the nervous system in clinical practice is crucial for diagnosing, managing, and tracking neurological conditions. By systematically assessing a patient’s history, physical function, and cognitive status, healthcare professionals can make informed decisions that directly impact patient outcomes.
Advanced Topics in Neurological Disorders
The field of neurological conditions is vast, encompassing a wide array of diseases that affect the brain, spinal cord, and peripheral nervous system. Some disorders are well understood, while others present complex challenges in diagnosis and treatment. In this section, we will explore more advanced topics in the realm of nervous system dysfunctions, shedding light on the mechanisms, cutting-edge research, and treatment options available for the most intricate cases.
While many neurological disorders are recognized and treated early, others are far more elusive and require specialized knowledge and expertise. These conditions often involve rare pathophysiological processes or complex interplays between genetic and environmental factors. Understanding these advanced topics is essential for clinicians aiming to provide effective care for patients with severe or progressive conditions.
Rare and Complex Neurological Diseases
- Prion Diseases: These include rare, degenerative conditions such as Creutzfeldt-Jakob disease. Prions, misfolded proteins, cause other proteins to also misfold, leading to irreversible neurological damage and ultimately death. The pathology and progression are not fully understood, making diagnosis and treatment extremely challenging.
- Neurodegenerative Disorders: Disorders such as Huntington’s disease, amyotrophic lateral sclerosis (ALS), and multiple system atrophy involve progressive degeneration of neurons. These diseases are characterized by gradual motor and cognitive decline, often without effective treatments to halt progression. Advanced research is focused on gene therapies, stem cell treatments, and new medications to slow the progression.
- Leukodystrophies: A group of rare genetic disorders that affect the white matter of the brain. These disorders lead to the loss of myelin, the protective covering of nerve fibers, and can cause severe cognitive and motor impairments. New advances in gene therapy offer hope for managing these debilitating conditions.
Emerging Diagnostic Techniques and Treatments
- Advanced Imaging Technologies: Techniques such as functional MRI (fMRI), positron emission tomography (PET), and diffusion tensor imaging (DTI) are revolutionizing the way clinicians visualize brain activity and detect abnormalities. These methods allow for earlier diagnosis, monitoring disease progression, and tailoring more personalized treatment plans.
- Gene Therapy and Precision Medicine: In some cases, genetic mutations are the root cause of neurological diseases. Gene therapy aims to directly correct or replace faulty genes. Precision medicine, which uses genetic, environmental, and lifestyle data to customize treatments, is becoming increasingly important in treating complex conditions like Alzheimer’s and Parkinson’s diseases.
- Stem Cell Research: Stem cell therapies hold the promise of regenerating damaged tissue, particularly in cases of spinal cord injury, stroke, or neurodegenerative diseases. While still in the experimental stages, stem cells offer potential for reversing some types of brain and spinal cord damage.
As advancements continue in understanding and treating neurological disorders, these complex conditions present both challenges and opportunities. The ability to diagnose rare diseases earlier, combined with emerging therapies and technological innovations, will likely transform how neurological care is provided in the future. Ongoing research and collaboration between scientists, clinicians, and patients are essential in improving the outcomes for individuals affected by these disorders.
Preparing for Neuro Exam with Practice
Preparation for assessments related to the nervous system requires not only understanding theoretical concepts but also honing practical skills. Mastery of both allows for better recall and efficient problem-solving when faced with complex scenarios. This section focuses on how consistent practice can improve performance and ensure a comprehensive understanding of key concepts, diagnostic techniques, and patient management strategies. Engaging with real-world cases, refining skills, and practicing different approaches will increase confidence and proficiency.
Key Areas to Focus On
- Understanding Pathophysiology: Comprehending how diseases affect the nervous system helps in identifying symptoms, signs, and underlying causes. Reviewing case studies and clinical scenarios can enhance your ability to make accurate diagnoses.
- Practicing Physical Examinations: Regular practice of neurological assessments, such as reflex testing, sensory examinations, and cranial nerve checks, is essential. Consistently performing these tasks ensures accuracy and improves patient interactions.
- Mastering Imaging Techniques: Gaining proficiency in reading diagnostic images like MRIs and CT scans can provide a deeper understanding of how anatomical and functional abnormalities present. This skill is crucial in interpreting findings in real clinical environments.
Strategies for Effective Practice
- Simulated Clinical Scenarios: Repeated exposure to clinical case simulations helps reinforce theoretical knowledge and prepares you for handling real-life situations. Practicing with peers, mentors, or virtual platforms allows for valuable feedback and learning.
- Mock Patient Encounters: Interacting with mock patients or standardized patients can help develop a patient-centered approach to care. These interactions focus on building communication skills while applying theoretical knowledge to practical situations.
- Active Recall and Spaced Repetition: Using study techniques like active recall, where you test yourself on key concepts, and spaced repetition, where information is reviewed at increasing intervals, can solidify your memory and improve long-term retention.
Regular practice not only strengthens knowledge but also fosters the confidence necessary to excel. By combining theory with hands-on experience, individuals can ensure they are prepared for any challenge that may arise in the clinical setting.