The critical care of infants during emergency situations requires specific knowledge and techniques that healthcare providers must master. This section provides essential guidelines for professionals to evaluate and manage various urgent scenarios involving newborns, ensuring optimal outcomes during these life-threatening situations.
By exploring key principles, such as airway management, heart rate assessment, and the administration of medications, medical staff can build the confidence needed to address immediate needs effectively. This approach helps ensure that even in high-pressure moments, the most appropriate actions are taken to stabilize and support the newborn’s health.
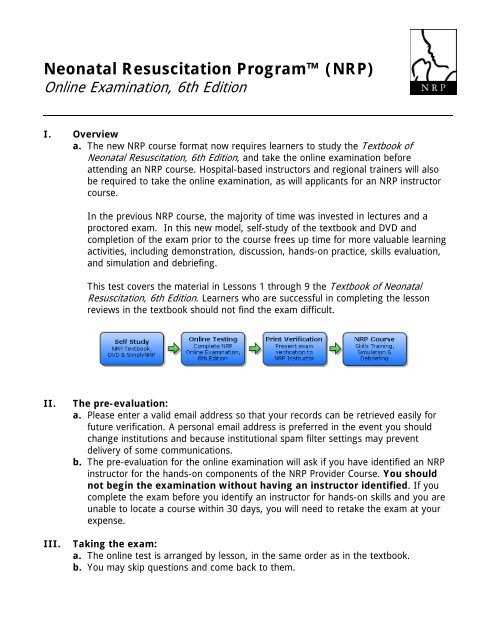
Newborn Emergency Care Evaluation
In critical situations involving infants, it is essential for healthcare providers to have a clear understanding of the appropriate actions to take. Effective evaluation of the newborn’s condition, along with rapid and accurate decision-making, plays a vital role in ensuring survival and long-term health. This section outlines key principles and methods used to assess and manage urgent infant care needs, enabling practitioners to confidently approach such emergencies.
Key Concepts for Effective Management
Comprehensive knowledge of life-saving techniques, airway interventions, and medication administration is necessary for successful management during infant emergencies. Familiarity with protocols ensures that healthcare professionals can perform necessary actions quickly and accurately.
Critical Steps for Immediate Action
Healthcare providers must know when to intervene, the appropriate techniques for stabilizing the infant, and how to monitor vital signs under pressure. These steps are crucial in preventing further complications and supporting the infant’s recovery.
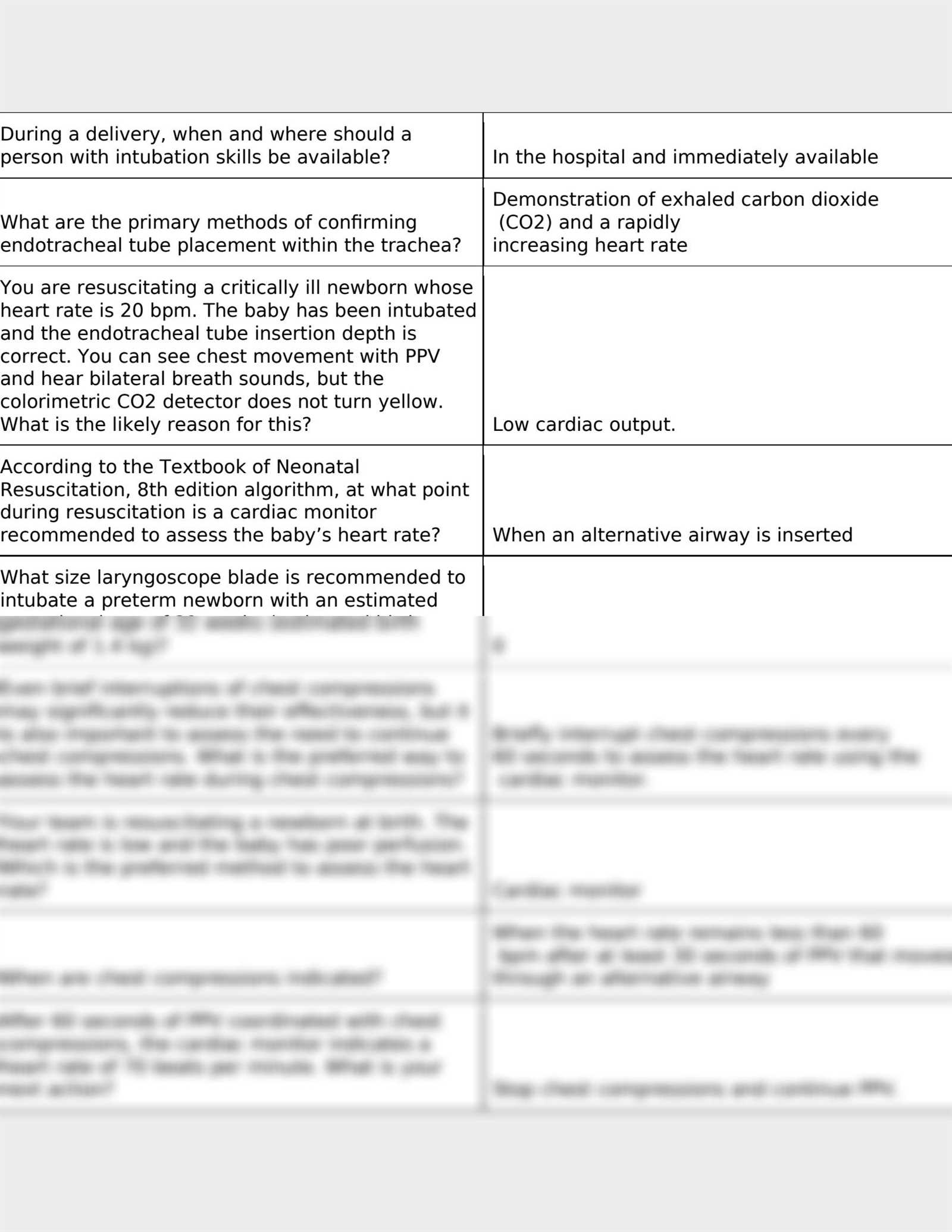
| Procedure | Indication | Action |
|---|---|---|
| Airway clearance | Obstructed airway | Use suction to clear airway |
| Chest compressions | Heart rate below 60 bpm | Perform compressions at appropriate depth and rate |
| Oxygen administration | Hypoxia | Provide supplemental oxygen |
| Epinephrine | Heart rate remains low | Administer epinephrine as per protocol |
Key Concepts in Newborn Critical Care
Understanding the essential principles of managing a newborn in distress is crucial for healthcare professionals. This involves recognizing life-threatening situations, assessing the infant’s condition promptly, and applying the most effective techniques to stabilize the baby. Mastery of these fundamental concepts ensures that medical staff can act swiftly and accurately in critical moments, improving the chances of a successful outcome.
Key aspects of newborn emergency care include airway management, proper assessment of the heart rate, and the use of appropriate interventions such as oxygen therapy or chest compressions. These actions are designed to address the immediate needs of the infant, enabling medical staff to maintain or restore vital functions quickly.
In addition, it is important to understand the specific protocols for handling various emergency scenarios, as well as the proper use of equipment and medications. A structured approach allows healthcare providers to prioritize actions, avoid common mistakes, and provide the best possible care in urgent situations.
Understanding the ABCDE Approach
The ABCDE approach is a structured method used in emergency medicine to assess and manage critically ill or injured patients. It ensures that healthcare providers prioritize interventions based on the severity of the patient’s condition. By following this systematic approach, practitioners can efficiently identify life-threatening issues and apply the appropriate actions to stabilize the patient in a logical sequence.
The ABCDE approach focuses on five key steps: airway, breathing, circulation, disability, and exposure. Each step is designed to address a specific aspect of the patient’s condition, ensuring that no critical issue is overlooked. The approach helps healthcare teams stay organized during high-stress situations, improving patient outcomes and reducing the likelihood of complications.
| Step | Focus | Action |
|---|---|---|
| A: Airway | Ensuring the airway is clear | Open the airway and remove any obstructions |
| B: Breathing | Assessing the patient’s breathing | Provide ventilation or oxygen if necessary |
| C: Circulation | Checking blood flow and pulse | Manage bleeding, provide fluids, and support circulation |
| D: Disability | Assessing neurological function | Check for responsiveness, pupil reaction, and limb movement |
| E: Exposure | Identifying hidden injuries or conditions | Expose the patient to fully assess for injuries while maintaining warmth |
Importance of Immediate Newborn Care
Providing prompt and effective care to an infant right after birth is critical for their survival and long-term health. Early interventions can prevent complications and address any immediate threats to the baby’s well-being. Proper management at this stage not only stabilizes the newborn but also sets the foundation for healthy development in the future.
Ensuring Vital Functions Are Stable
One of the key aspects of early newborn care is ensuring that the infant’s vital functions, such as breathing and heart rate, are functioning properly. Immediate action may be required to assist with breathing or stimulate the baby to initiate their own respiration. This can significantly reduce the risk of life-threatening conditions such as hypoxia or cardiac arrest.
Minimizing Long-Term Health Risks
Timely care during the initial moments after birth can help identify and address potential health risks that might affect the infant later in life. For instance, detecting and treating infections or metabolic imbalances early can prevent more serious complications from developing. Early interventions are essential for minimizing the long-term impact on the child’s health.
Recognizing Respiratory Distress in Newborns
Respiratory distress in newborns is a critical condition that requires immediate attention. It is essential for healthcare providers to quickly identify the signs and symptoms that indicate a newborn may be struggling to breathe. Early recognition allows for prompt intervention, which can significantly improve the chances of a positive outcome.
Signs of Respiratory Distress
The following signs may indicate that a newborn is experiencing difficulty breathing:
- Rapid or shallow breathing
- Flared nostrils
- Grunting or making noises during exhalation
- Abnormal chest movements, such as retractions
- Blue or pale skin, especially around the lips and fingertips
- Weak cry or lack of crying
Common Causes of Breathing Issues
Several factors can lead to respiratory problems in newborns. These may include:
- Premature birth: Premature infants often have underdeveloped lungs, which can make breathing difficult.
- Infections: Bacterial or viral infections can cause inflammation and impair normal respiratory function.
- Airway obstructions: Physical blockages, such as mucus or meconium, can prevent airflow.
- Birth trauma: Injuries during delivery can lead to breathing difficulties, especially in cases of hypoxia or chest trauma.
Role of Chest Compressions in Emergency Care
Chest compressions are a critical intervention used in emergency situations to maintain circulation and oxygen delivery to vital organs when the heart is not beating effectively. This technique helps ensure that blood continues to flow to the brain and other organs, providing the necessary support until the heart starts functioning normally or other interventions can be made. Effective chest compressions can significantly improve the chances of survival during a life-threatening event.
When to Perform Chest Compressions
Chest compressions are typically performed when the heart rate of the infant drops below a certain threshold, usually under 60 beats per minute, despite adequate ventilation. They are also indicated when the baby shows no signs of circulation or when other resuscitative efforts have not restored a normal heart rhythm. Early and timely initiation of compressions is essential to improving outcomes in these critical situations.
Technique and Effectiveness of Chest Compressions
Proper technique is vital for the success of chest compressions. The following guidelines are important:
- Positioning: The infant should be placed on a firm surface with their head slightly tilted back to open the airway.
- Compression Depth: The compressions should be approximately one-third of the chest depth to ensure effective blood flow.
- Compression Rate: Compressions should be delivered at a rate of about 100 to 120 per minute.
- Continuous Monitoring: It’s important to regularly assess the effectiveness of compressions and adjust as needed.
When done correctly, chest compressions can restore circulation and significantly improve the likelihood of a positive outcome in infants experiencing cardiac arrest or severe bradycardia.
Effective Use of Suction in Newborns
Clearing the airway is one of the first steps in managing a newborn in distress. Suctioning is a vital technique used to remove mucus, amniotic fluid, or other obstructions that can impede the infant’s ability to breathe properly. Proper suctioning helps ensure the airway is open and reduces the risk of complications such as aspiration or respiratory distress.
When to Use Suction
There are specific situations where suctioning is necessary. These include:
- Obstructed Airway: When there is visible mucus or fluid blocking the infant’s airway.
- Excessive Secretions: If the baby is struggling to clear excessive mucus or fluid on their own.
- Difficulty Breathing: If the infant shows signs of labored breathing or poor oxygenation due to airway blockage.
Proper Technique for Suctioning
Effective suctioning requires precision to avoid harm while ensuring that the airway is cleared. Here are key steps to follow:
- Choose the Right Equipment: Use a suction device appropriate for the infant’s size, such as a bulb syringe or a mechanical suction unit.
- Limit Suction Duration: Suctioning should be done for no more than 5 seconds at a time to prevent damage to the airway or excessive oxygen depletion.
- Positioning: Keep the baby’s head slightly tilted to one side to allow gravity to help with drainage while suctioning.
- Monitor Oxygen Levels: After suctioning, assess the baby’s oxygenation and breathing to ensure the airway remains clear.
While suctioning is a critical procedure, it should be done carefully to avoid trauma to the delicate tissues of the newborn’s airway. Proper technique ensures that the infant can breathe freely and receive adequate oxygen, supporting their immediate survival and well-being.
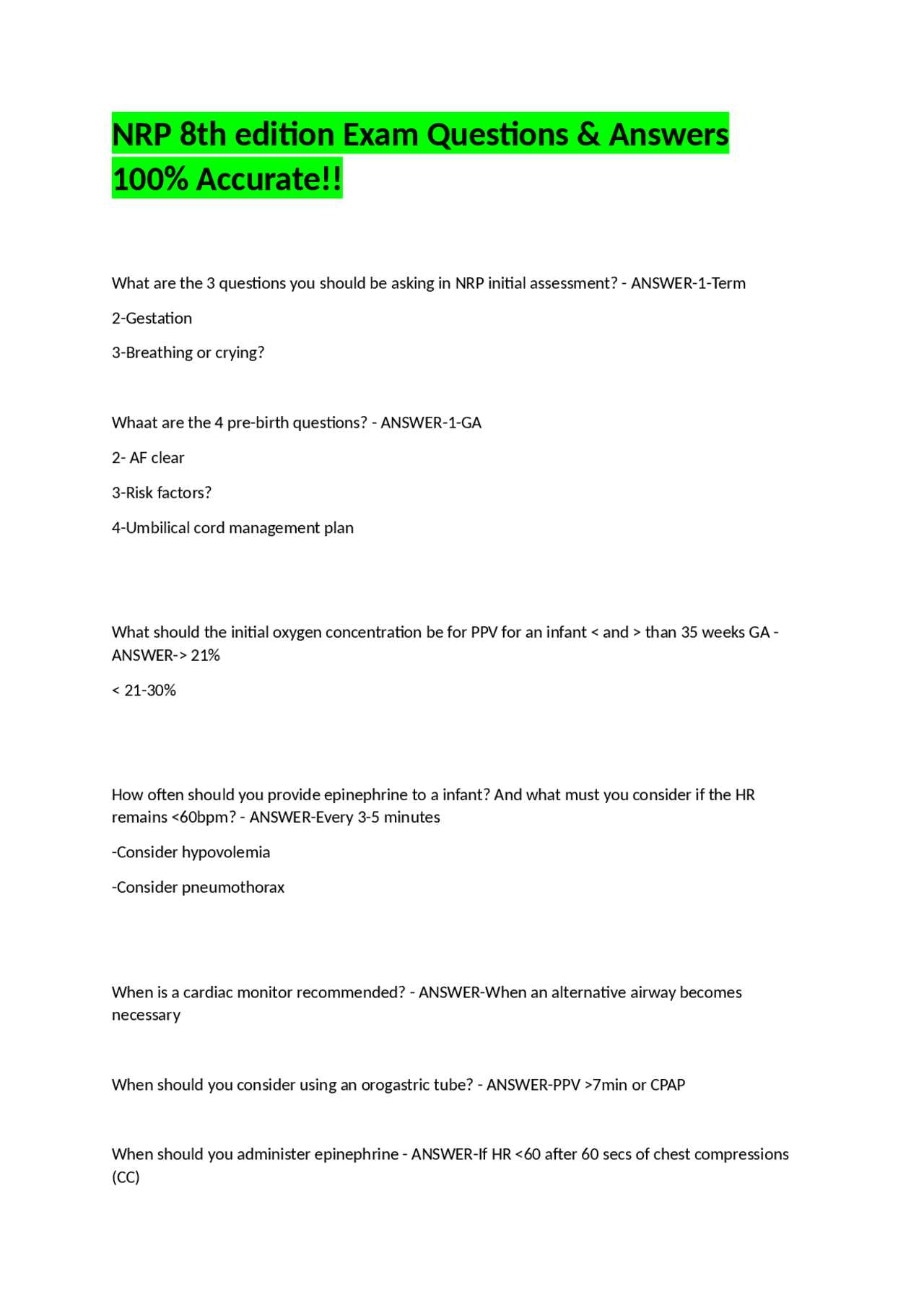
When to Administer Epinephrine
Epinephrine is a crucial medication used in emergency care to stimulate the heart and improve circulation. It is particularly important when a newborn’s heart rate is dangerously low or when other interventions have not been effective. Understanding when and how to administer this drug can significantly impact the chances of survival and recovery in critical situations.
Indications for Epinephrine Administration
Epinephrine should be considered when the infant exhibits signs of severe bradycardia (a heart rate less than 60 beats per minute) despite adequate ventilation and chest compressions. It is also indicated in cases of cardiac arrest or when there is poor perfusion, which could lead to irreversible organ damage if not corrected promptly. Key signs include:
- Heart rate below 60 beats per minute after sufficient ventilation
- Failure of the heart rate to improve with other resuscitative efforts
- Signs of inadequate blood circulation such as low blood pressure, poor peripheral perfusion, or cyanosis
Administration Guidelines
The correct timing and dosage are essential for the effectiveness of epinephrine. In general, it is administered through either an intravenous or intraosseous route. If these routes are not available, it may be given through the endotracheal tube. The dose is typically 0.01 to 0.03 mg/kg of the infant’s body weight, and it may be repeated every 3-5 minutes if necessary. Healthcare providers should continue to monitor the infant closely to assess the drug’s effectiveness and adjust the approach accordingly.
Approach to Airway Management
Effective airway management is essential in ensuring proper oxygenation and ventilation in critical situations. The first priority in any emergency care is to secure the airway and ensure that air can flow freely into the lungs. Whether due to obstruction, respiratory distress, or other complications, maintaining an open and clear airway is a fundamental step in improving the chances of survival and recovery.
Initial Assessment and Airway Opening
The first step in airway management is to assess the newborn’s breathing and determine if there is any obstruction. If the airway is blocked, the following actions should be taken:
- Positioning: The head should be placed in a neutral or slightly extended position to align the airway and facilitate easier breathing.
- Clear the Airway: Use suction devices, such as a bulb syringe or a suction catheter, to remove any secretions, mucus, or fluids that may be obstructing the airway.
- Stimulate Breathing: Gentle tactile stimulation can help initiate normal breathing patterns if the newborn is not actively breathing.
Advanced Airway Management
If basic measures do not resolve the airway issue, more advanced techniques may be required. These include:
- Endotracheal Intubation: In cases where ventilation is inadequate, inserting an endotracheal tube can ensure direct access to the airway and provide effective breathing support.
- Positive Pressure Ventilation: If the newborn’s respiratory effort is insufficient, positive pressure ventilation can be used to assist breathing and improve oxygenation.
- Monitoring: Continuous assessment of oxygen levels, heart rate, and overall clinical status is essential to adjust interventions as needed.
Effective airway management is a dynamic process that requires quick thinking, precision, and appropriate equipment. Timely intervention can greatly improve outcomes in critical situations and support the infant’s recovery.
Neonatal Oxygenation Guidelines
Oxygenation plays a vital role in supporting the respiratory function of newborns, particularly those in distress. Ensuring adequate oxygen levels helps prevent organ damage, supports brain function, and stabilizes the infant’s overall condition. Proper management of oxygen delivery requires a clear understanding of the guidelines to ensure both safety and effectiveness.
Initial Oxygen Administration
When a newborn is unable to breathe adequately on their own, oxygen must be provided promptly to prevent hypoxia. The initial approach to oxygen administration depends on the infant’s condition:
- Room Air: In most cases, a healthy newborn will begin breathing on their own and only need room air for oxygenation.
- Supplemental Oxygen: If the infant shows signs of inadequate oxygenation, such as low heart rate or cyanosis, supplemental oxygen may be required. This can be delivered via a face mask or oxygen hood.
- Positive Pressure Ventilation: If the newborn is unable to breathe effectively, positive pressure ventilation may be necessary to deliver oxygen directly into the lungs.
Monitoring and Adjusting Oxygen Levels
Continuous monitoring of oxygen saturation is critical to ensure the infant’s oxygen levels remain within the safe range. The following guidelines should be followed:
- Target Oxygen Saturation: Aim for an oxygen saturation of 85-95% during the first minutes of life. This range minimizes the risk of complications while ensuring adequate oxygen delivery.
- Adjust Oxygen Flow: If oxygen saturation is too low or too high, adjust the flow rate or method of delivery to stabilize the infant’s condition.
- Regular Assessment: Oxygen saturation should be checked frequently using a pulse oximeter, along with monitoring the infant’s heart rate and respiratory effort.
Proper oxygen management is crucial for supporting the vital functions of a newborn in distress. By following these guidelines, healthcare providers can ensure optimal oxygen delivery and reduce the risks associated with hypoxia and respiratory complications.
How to Assess Heart Rate During Resuscitation
Assessing the heart rate is a critical step in determining the effectiveness of emergency care for a newborn. The heart rate provides vital information regarding the infant’s circulatory status and response to intervention. Accurate measurement helps guide the decision-making process, ensuring that appropriate actions are taken to stabilize the infant’s condition.
Methods for Heart Rate Measurement
There are several techniques for assessing the heart rate, and selecting the right method depends on the newborn’s condition and the available equipment. The most common approaches are:
- Stethoscope: A simple and effective tool, the stethoscope is commonly used to listen for heart sounds in the chest. The heart rate can be counted by listening for the beats over a full minute.
- Umbilical Cord: In critical situations, the heart rate can be palpated through the umbilical cord if it remains intact. This method can provide a quick assessment of circulation in the early stages.
- ECG Monitoring: In more advanced settings, ECG (electrocardiogram) monitors can provide continuous, real-time data on the infant’s heart rate, offering a more precise and consistent reading.
Interpreting Heart Rate Findings
Once the heart rate is assessed, interpreting the results is essential to guide further action:
- Normal Heart Rate: A heart rate of 100 beats per minute or higher typically indicates that the infant is adequately oxygenated and does not require immediate interventions.
- Low Heart Rate: A heart rate below 60 beats per minute requires immediate intervention, such as chest compressions or administration of medications like epinephrine, to restore circulation and oxygen supply.
- Rapid Heart Rate: A heart rate significantly above normal levels may indicate distress, and further evaluation is needed to identify the underlying cause and determine appropriate management.
Effective monitoring and prompt action based on heart rate readings can significantly improve the chances of survival and recovery for a newborn in critical condition. It is important to continuously assess the heart rate throughout the care process to make informed decisions and adjust interventions as needed.
Techniques for Thermal Regulation
Maintaining an infant’s body temperature is crucial in the early stages of life. Without proper thermal regulation, a newborn is at risk of complications such as hypothermia, which can affect their metabolism, oxygen levels, and overall stability. Ensuring the infant is kept warm helps improve circulation, promote breathing, and support other essential bodily functions.
Methods to Maintain Body Temperature
Several effective techniques are used to maintain the infant’s temperature, ensuring they stay warm and comfortable. Some of the most common approaches include:
- Skin-to-Skin Contact: Placing the newborn directly on the caregiver’s chest helps regulate body temperature through shared warmth. This method is highly effective and encourages bonding while providing warmth.
- Warm Blankets: Wrapping the infant in pre-warmed blankets creates a barrier against heat loss and provides insulation, especially in colder environments.
- Incubators: In more controlled settings, incubators are used to maintain a constant temperature. These devices regulate the surrounding environment to keep the infant warm without the risk of overheating.
- Cap and Socks: Wearing a cap helps prevent heat loss from the infant’s head, while socks keep the extremities warm. These are essential accessories for managing thermal comfort.
Monitoring and Adjusting Temperature
It is important to continuously monitor the infant’s temperature to ensure they are not too cold or overheated. Techniques to measure and adjust include:
- Thermometers: Use of a thermometer to check the infant’s body temperature regularly is essential. The ideal temperature range is typically between 36.5°C and 37.5°C (97.7°F to 99.5°F).
- Environmental Control: In the case of incubators or heated environments, the temperature should be adjusted based on regular assessments to keep the infant comfortable.
- Adjusting Clothing: Clothing and bedding should be adjusted according to the infant’s temperature, adding or removing layers as needed to maintain a stable body temperature.
Proper thermal regulation is vital for supporting a newborn’s health and development. By implementing these techniques, healthcare providers can ensure that the infant remains in an optimal temperature range, promoting better overall health outcomes.
Monitoring Blood Sugar Levels in Newborns
Keeping track of blood sugar levels in infants is an essential aspect of early care, especially since their bodies are adjusting to life outside the womb. Proper glucose levels are crucial for a newborn’s energy, growth, and overall health. If left unchecked, imbalances can lead to serious complications such as hypoglycemia or hyperglycemia, which can affect brain function and organ development.
Blood sugar monitoring is typically done through regular tests to ensure that the infant’s glucose levels stay within a safe and optimal range. This process helps detect early signs of issues that might need intervention, such as feeding problems or metabolic conditions.
Methods of Monitoring Blood Sugar
There are various ways to measure blood glucose in newborns, depending on the situation and the available resources:
- Heel Stick Test: A small amount of blood is drawn from the heel using a lancet. This method is quick and commonly used in hospitals to test for low blood sugar levels.
- Capillary Blood Sampling: A blood sample is taken from a capillary, usually from the heel or the finger, and tested using a glucose meter.
- Blood Gas Analysis: In more critical cases, blood may be drawn from an artery or vein and analyzed to measure glucose levels in addition to other vital parameters.
When to Monitor Blood Sugar Levels
Some newborns are more at risk for blood sugar imbalances and require more frequent monitoring. Common reasons for close observation include:
- Preterm Infants: Premature babies often have underdeveloped systems, making them more susceptible to glucose instability.
- Infants with Low Birth Weight: Babies who are born underweight may struggle with regulating their blood sugar levels.
- Infants of Diabetic Mothers: Babies born to mothers with diabetes are at higher risk of experiencing low or high blood sugar after birth.
- Signs of Hypoglycemia: If the infant shows symptoms like jitteriness, poor feeding, or lethargy, blood sugar levels should be checked immediately.
Early detection of blood sugar imbalances is essential for ensuring the infant’s well-being. Timely intervention, such as providing the proper nutrition or glucose supplementation, can prevent further complications and promote healthy development.
Understanding Medication Dosages for Newborns
Administering the correct medication dosage to infants is a critical aspect of their healthcare. Due to their small size, immature organs, and developing metabolism, newborns process medications differently compared to older children or adults. As a result, accurate dosage calculations are essential to avoid both underdosing and overdosing, which could lead to serious health complications.
In many cases, medications need to be adjusted based on the infant’s weight, age, and overall health status. Healthcare providers must take into account several factors to ensure safe and effective treatment, including the specific condition being treated and the infant’s response to therapy.
Key Factors Affecting Dosage Calculation
Several factors influence how medications should be dosed for newborns:
- Weight: Newborns’ dosages are often calculated based on their weight. Since infants can vary greatly in size, this ensures that the correct amount of medication is given according to their body mass.
- Gestational Age: The age at birth, whether premature or full-term, also affects how medications are processed. Premature infants may require lower doses due to their underdeveloped organs.
- Metabolic Rate: Newborns have a higher metabolic rate compared to adults, which can affect how fast the body absorbs and eliminates medications.
- Condition Being Treated: The severity of the illness being treated also plays a role in determining the appropriate dosage. In some cases, medication needs may vary depending on the specific health challenges the infant faces.
Common Medications and Their Dosages
Newborns may require a variety of medications, from antibiotics to pain relievers. Here are a few examples of commonly administered drugs and their typical dosage adjustments:
- Antibiotics: Used to treat bacterial infections, these are often dosed based on weight, with a typical range of 10–20 mg per kilogram of body weight, depending on the specific antibiotic.
- Vitamin K: Administered shortly after birth to prevent bleeding, the standard dose is 1 mg for infants.
- Paracetamol: Used for pain relief, it is typically dosed at 10–15 mg per kilogram of body weight, given every 4–6 hours as needed.
- Surfactant: For infants with respiratory distress, surfactant therapy may be required, with dosage and timing based on the infant’s lung condition and weight.
Ensuring that the right medication and dosage are administered is essential for minimizing risks and improving health outcomes. Healthcare providers must carefully monitor infants after administering medications to ensure effectiveness and safety.
Common Errors in Newborn Emergency Care
When it comes to providing urgent care to newborns, even small mistakes can have serious consequences. In high-pressure situations, healthcare providers must stay vigilant and focused to avoid errors that could jeopardize the infant’s health. Understanding the common mistakes that occur during these critical moments is key to improving care outcomes and minimizing risks.
Errors in emergency care can stem from a variety of factors, including lack of training, poor communication, and failure to follow established protocols. It is crucial that all healthcare professionals involved in newborn care are familiar with best practices and remain aware of potential pitfalls during critical interventions.
Common Mistakes and Their Impact
Several frequent errors occur during the urgent care of newborns that can affect their chances of survival and recovery:
- Improper Airway Management: Failing to secure a clear airway is one of the most common and potentially fatal mistakes. This can lead to respiratory distress or failure to breathe, further complicating the infant’s condition.
- Incorrect Ventilation Pressure: Both excessive or insufficient pressure during ventilation can lead to lung injury or ineffective oxygenation. Proper training in techniques and equipment settings is essential to avoid this error.
- Delayed or Inadequate Circulatory Support: Failure to administer chest compressions or delayed initiation of this support can severely affect the baby’s blood circulation and oxygen delivery, potentially leading to organ failure.
- Improper Use of Medications: Administering incorrect dosages or inappropriate medications during a critical moment can worsen the infant’s condition. Dosing errors are often caused by incorrect weight calculations or misinterpretation of guidelines.
- Lack of Monitoring: Inadequate monitoring of vital signs during the intervention, such as heart rate, oxygen levels, and blood pressure, can result in unnoticed deterioration. Continuous assessment is vital to ensure effective care.
Mitigating Errors through Training and Protocols
Preventing these errors requires a combination of thorough training, clear communication, and adherence to established protocols. Healthcare professionals should regularly update their skills and knowledge to keep up with evolving guidelines and technologies. Moreover, team coordination is essential to ensure that each step of care is performed correctly and efficiently.
By learning from past mistakes and continuously refining care practices, healthcare providers can significantly improve outcomes in newborn emergencies and reduce the risk of complications.
How to Perform Proper Documentation
Effective documentation is a cornerstone of quality healthcare. It serves as a detailed record of all actions taken during a medical intervention, helping to ensure continuity of care, legal protection, and clear communication between healthcare teams. Proper documentation also facilitates the evaluation of care effectiveness and is crucial for clinical decision-making in the future.
In any medical setting, especially during critical situations, it is vital to document each step accurately. This includes all procedures performed, medications given, and the patient’s response to treatment. Timely and complete records ensure that essential information is available for future review, whether for legal purposes, audits, or ongoing patient care. Thorough documentation also aids in identifying areas for improvement in medical practices.
Key Aspects of Accurate Documentation
There are several key elements to consider when documenting a patient’s care, ensuring that the information is clear, accurate, and useful:
- Timestamping: Record the exact times of interventions and responses. This allows for a detailed sequence of events and is crucial for understanding the timeline of care.
- Specific Details: Note all relevant details about the actions performed, such as specific procedures, dosages of medications, and types of equipment used.
- Patient Response: Document how the patient responded to each intervention. This includes any changes in vital signs or overall condition.
- Team Involvement: List all individuals involved in the care process, specifying their roles to ensure accountability and clarity.
- Follow-up Instructions: Include plans for ongoing care, monitoring, and any further treatments needed after the initial intervention.
Best Practices for Comprehensive Documentation
To maintain high standards in documentation, healthcare providers should follow these best practices:
- Be Precise and Clear: Avoid vague language. Use clear, direct statements to describe each action and its result.
- Follow Standardized Terminology: Use universally accepted medical terms to avoid confusion and ensure that the records are easily understood by other professionals.
- Ensure Readability: Whether handwritten or digital, ensure that your documentation is legible and easy to follow.
- Review and Update: Regula
Reviewing Post-Care Steps
After immediate interventions have been carried out, the focus shifts to ensuring that the patient continues to stabilize and recover. This phase involves monitoring the patient’s condition, managing ongoing needs, and preventing complications. Effective post-care ensures that the efforts made during the initial phase have lasting positive effects and that the patient progresses toward full recovery.
During post-care, healthcare providers need to assess various systems of the body, support respiratory and circulatory functions, and provide any additional treatments as necessary. It is essential to closely observe the patient for signs of improvement or any issues that might arise after the first phase of treatment.
Key Post-Care Actions
After the initial care has been provided, several key steps must be followed to promote recovery and prevent setbacks:
- Monitoring Vital Signs: Regularly check heart rate, respiratory rate, blood pressure, oxygen levels, and body temperature to ensure that the patient remains stable.
- Providing Respiratory Support: If necessary, administer oxygen therapy or other forms of respiratory assistance to ensure adequate oxygen levels in the bloodstream.
- Maintaining Thermal Balance: Ensure that the patient is kept at the appropriate temperature by using heated blankets, incubators, or other devices to prevent hypothermia.
- Circulatory Support: If blood pressure or perfusion is low, administer intravenous fluids or medications to support circulatory function.
- Neurological Assessment: Continuously evaluate the patient’s neurological function to check for any signs of distress or abnormalities in behavior or reflexes.
Follow-Up and Ongoing Evaluation
In the post-care phase, regular follow-up and evaluation are critical to ensure that the patient is progressing as expected. These steps include:
- Regular Monitoring: Continue frequent monitoring of vital signs and physical condition to identify any changes or complications early.
- Multidisciplinary Consultation: Collaborate with specialists as needed to address any concerns or to further optimize care based on the patient’s condition.
- Documentation of Care: Carefully document all interventions, changes in the patient’s condition, and any important decisions made during this phase.
- Family Communication: Keep the family informed about the patient’s condition and progress, offering updates on treatments and expected outcomes.
Effective post-care is essential for ensuring that the patient continues to improve and avoids complications. By closely monitoring the patient, providing support as necessary, and remaining vigilant for any changes, healthcare professionals can help ensure the best possible outcome after initial treatment.