Accurate medical documentation is a vital component of patient care, especially in procedures involving sensitive health assessments. Proper record-keeping ensures clear communication between healthcare providers, supports clinical decision-making, and maintains patient safety throughout treatment. Effective documentation serves as a reference point for future consultations and enables better continuity of care.
In the context of women’s health, documenting key observations during a physical assessment is essential for tracking progress, identifying potential issues, and planning appropriate interventions. Healthcare professionals rely on structured methods to record both subjective experiences and objective findings. This approach not only aids in diagnosis but also supports the development of a comprehensive care plan tailored to individual needs.
Well-structured documentation helps create a clear picture of the patient’s condition, leading to more informed decisions and improved treatment outcomes. By adhering to established guidelines for accurate and concise record-keeping, providers can contribute to better healthcare delivery and maintain the highest standards of patient care.
Pelvic Exam SOAP Note Guide
Documenting clinical assessments accurately is crucial in providing high-quality care, especially during intimate health evaluations. A structured approach to recording key findings ensures that relevant information is captured in a clear and organized manner. This process is essential for guiding future care decisions and maintaining consistency in medical records.
When documenting a woman’s health evaluation, healthcare providers focus on both subjective information shared by the patient and objective data gathered through examination. The primary goal is to create a comprehensive account that reflects the patient’s current condition, enabling practitioners to assess the need for further action or treatment. This guide highlights the critical components that should be included in detailed medical records following such assessments.
By adhering to standardized documentation practices, providers not only enhance communication among healthcare teams but also improve patient outcomes. Clear, concise, and thorough recording ensures that all aspects of the assessment are addressed, reducing the risk of overlooking important details and improving the continuity of care.
Understanding SOAP Notes in Healthcare
In healthcare, documenting patient interactions and assessments is an essential practice for maintaining accurate records and ensuring effective treatment. A standardized format allows medical professionals to capture critical information in a structured way, making it easier to track progress, evaluate outcomes, and communicate with other providers. This method of documentation helps create a comprehensive picture of a patient’s health status and aids in decision-making throughout the care process.
One widely used method for organizing clinical data is the SOAP format. This system divides documentation into distinct sections: subjective observations, objective findings, assessment of the situation, and a plan for follow-up care. Each of these components plays a vital role in building an accurate, detailed record that can guide future treatment decisions and facilitate better communication among healthcare providers.
By using a consistent framework, SOAP documentation enhances clarity and ensures that important details are not overlooked. It allows for easy comparison over time and helps create a seamless flow of information, which is critical in managing patient care effectively. This method also improves efficiency by streamlining the documentation process, allowing healthcare professionals to spend more time focusing on patient well-being.
Importance of Accurate Documentation
In the healthcare field, precise and thorough record-keeping is a cornerstone of quality patient care. The ability to accurately document clinical encounters ensures that all relevant information is available for future reference, which is crucial for providing consistent and informed treatment. Detailed records allow healthcare providers to monitor patient progress, detect potential issues early, and make well-informed decisions regarding ongoing care.
Moreover, accurate documentation serves as a legal and ethical safeguard. It helps protect both the healthcare provider and the patient by ensuring that the care provided is transparent, well-documented, and in compliance with medical guidelines. It also plays a key role in facilitating communication among different members of the care team, ensuring everyone is aligned with the patient’s treatment plan.
Below is a table outlining the key benefits of maintaining accurate records:
| Benefit | Description |
|---|---|
| Improved Patient Care | Ensures all relevant information is available for informed decision-making. |
| Legal Protection | Provides a record of care given, helping to prevent legal issues. |
| Better Communication | Facilitates clear communication among healthcare professionals involved in patient care. |
| Accurate Tracking | Helps track patient progress over time and identify areas that need attention. |
Overview of Pelvic Exam Procedures

Clinical evaluations focused on women’s reproductive health involve a variety of assessments designed to gather essential information about a patient’s condition. These procedures are crucial for diagnosing and monitoring health issues, ensuring that the healthcare provider has the necessary data to make informed decisions about treatment and care. The process typically includes both a physical examination and the gathering of subjective information shared by the patient.
During such assessments, the healthcare provider carefully examines the relevant areas of the body, looking for signs of abnormalities or conditions that may require further investigation. This can include checking for infections, structural issues, or other health concerns related to the reproductive organs. In addition to the physical examination, the provider will often inquire about the patient’s medical history and current symptoms to ensure a comprehensive understanding of the patient’s health status.
These procedures are conducted in a manner that prioritizes patient comfort and privacy. The healthcare provider ensures that the patient is informed and at ease throughout the process, explaining each step and addressing any concerns. Accurate documentation of these procedures is essential, as it provides a clear record of findings that can guide future care decisions.
Key Elements of SOAP Notes
In medical documentation, a well-structured format is essential for capturing and organizing patient information. The system used to document clinical encounters is designed to ensure that all relevant aspects of the patient’s condition are clearly recorded. This method divides the documentation into distinct sections, each serving a specific purpose to create a comprehensive picture of the patient’s health status.
The primary components of this structure include subjective details, objective findings, an assessment of the patient’s condition, and a plan for future care. Each section plays a vital role in building an accurate, concise record. The subjective portion captures the patient’s reported symptoms and concerns, while the objective section focuses on the provider’s clinical observations and physical examination results. The assessment provides a synthesis of the information, helping to guide the diagnosis, and the plan outlines the next steps in treatment or follow-up care.
By following this framework, healthcare professionals ensure that critical information is not overlooked and that the record is both thorough and easy to understand. This organized approach supports clear communication, informed decision-making, and effective patient management across various healthcare settings.
Subjective Section: What to Include
The subjective section of a clinical record is focused on gathering information directly from the patient. This section is essential for understanding the patient’s experiences, concerns, and symptoms from their perspective. It provides a foundation for further evaluation and guides healthcare providers in forming a comprehensive picture of the patient’s condition.
Key Aspects to Document
In this section, healthcare professionals should capture a variety of important details, including but not limited to:
- Chief Complaint: The main issue or symptom the patient is seeking help for.
- History of Present Illness: A detailed account of the current health issue, including onset, duration, severity, and any relevant factors.
- Past Medical History: Relevant previous conditions or treatments that could influence the current health situation.
- Medications: A list of current medications, including dosage and frequency.
- Allergies: Any known allergies, especially to medications, foods, or environmental factors.
- Family History: A history of conditions in the family that may be relevant to the patient’s health.
Patient’s Descriptions and Concerns
It is important to document how the patient describes their symptoms, any emotional or psychological factors that may influence their condition, and their expectations or concerns about treatment. This can help tailor the approach to their needs and build a rapport, fostering better trust and communication.
By thoroughly documenting these aspects, the healthcare provider can create a clearer understanding of the patient’s experience, which is essential for planning effective care and treatment strategies.
Objective Findings in Clinical Documentation
The objective section of a healthcare record focuses on the healthcare provider’s observations and clinical measurements. Unlike the subjective portion, which is based on the patient’s report, this section contains tangible data gathered during the assessment. These findings provide an essential foundation for diagnosing the patient’s condition and planning the appropriate course of action.
Objective findings typically include the results of physical examinations, laboratory tests, and any imaging or diagnostic procedures. These are facts that can be measured, observed, or verified by the healthcare provider. It is essential to record these details precisely to ensure the accuracy and reliability of the medical record.
Key components to include in this section:
- Physical Examination: This includes findings such as palpation, auscultation, inspection, and other hands-on techniques used to assess the patient’s condition.
- Vital Signs: Blood pressure, heart rate, respiratory rate, and temperature.
- Laboratory Results: Data from blood tests, urine samples, or other diagnostic tests performed to identify specific conditions.
- Imaging Results: Information from X-rays, MRIs, ultrasounds, or other diagnostic images relevant to the patient’s condition.
- Functional Assessments: Observations of the patient’s movement, range of motion, or physical abilities.
Accurate and clear documentation of objective findings ensures that all healthcare team members are on the same page regarding the patient’s current status and can make informed decisions based on the facts. This section plays a crucial role in creating a complete and precise medical record that supports clinical judgment and improves patient care.
Assessing the Examination Results
After conducting a thorough clinical assessment, healthcare providers must carefully analyze the gathered findings to form an accurate understanding of the patient’s condition. This process involves evaluating the data from both the physical examination and any relevant tests or imaging results. A comprehensive analysis helps identify underlying conditions, assess the severity of symptoms, and guide the development of an appropriate treatment plan.
Key Considerations in Assessment
When assessing the results, it is essential to consider several key factors:
- Consistency: Are the physical findings consistent with the patient’s reported symptoms?
- Symptom Progression: Has there been any change in the patient’s condition since previous visits?
- Potential Complications: Are there any indications of complications or risk factors that could affect treatment outcomes?
- Contextual Factors: Are there lifestyle, family history, or environmental factors that could influence the assessment?
Documenting the Assessment
The assessment section serves to synthesize the information gathered and offer a clear diagnosis or clinical impression. This is where healthcare providers interpret the objective findings and use their professional judgment to evaluate the patient’s condition. Below is an example of how to structure this portion of the record:
| Finding | Interpretation | Possible Diagnosis |
|---|---|---|
| Abdominal tenderness | Indicates possible inflammation or infection | Gastrointestinal infection or pelvic inflammatory disease |
| Abnormal discharge | Suggests a potential infection or hormonal imbalance | Bacterial vaginosis or yeast infection |
| Fever | Points to an active infection or systemic inflammation | Infection or inflammatory condition |
By carefully analyzing and interpreting the results, the healthcare provider can determine the most appropriate next steps in managing the patient’s condition. This assessment ensures that all factors are considered before making a diagnosis or developing a treatment plan.
Planning Treatment Based on SOAP Notes
After completing a clinical assessment and recording all relevant findings, the next step is to develop a treatment plan tailored to the patient’s needs. This planning process is crucial for ensuring effective management of the patient’s condition and promoting recovery. The information documented in the assessment and diagnosis sections plays a key role in shaping the approach to care, allowing healthcare providers to make informed decisions about therapeutic options.
Key Steps in Developing a Treatment Plan
Creating a comprehensive treatment plan involves several important considerations, which can include:
- Addressing Immediate Concerns: Identifying urgent issues that need prompt attention, such as infections or acute pain.
- Setting Long-Term Goals: Establishing objectives for recovery, symptom management, or prevention of further complications.
- Selecting Appropriate Treatments: Choosing medications, therapies, or lifestyle changes based on the patient’s condition and preferences.
- Monitoring Progress: Determining the need for follow-up visits, tests, or adjustments to the plan as the patient’s condition evolves.
Types of Treatment Options
Based on the patient’s condition and the data recorded, treatment options may vary. Some common types of interventions include:
- Pharmacological Interventions: Prescribing medication to manage symptoms or treat underlying conditions, such as antibiotics for infections or pain relievers for discomfort.
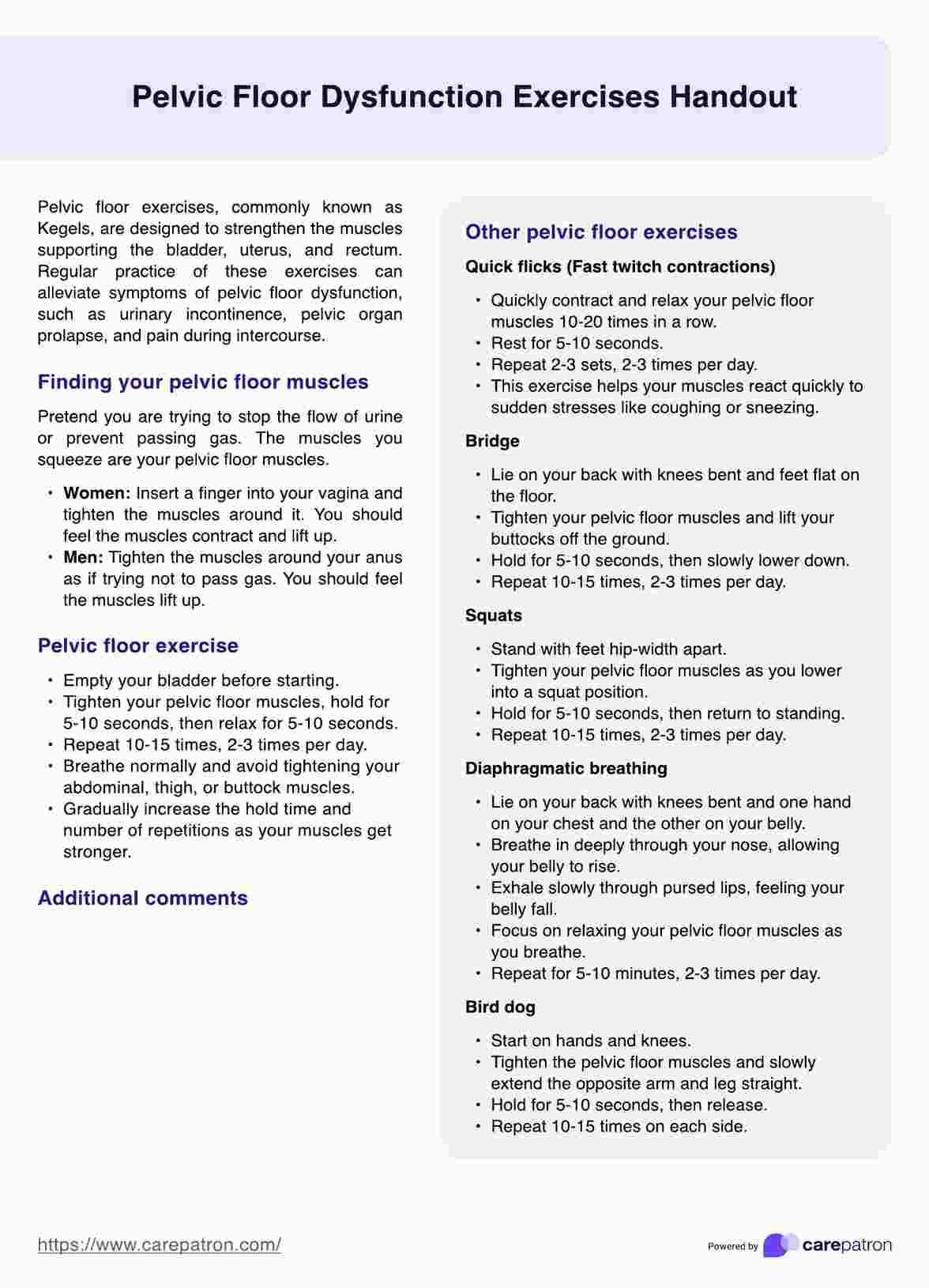
- Physical Therapy: Recommending exercises or other physical treatments to improve mobility, strength, or function.
- Surgical Interventions: In cases of more severe conditions, referring the patient for surgical evaluation or procedures might be necessary.
- Lifestyle Modifications: Suggesting changes to diet, exercise, or daily routines to support overall health and prevent recurrence of issues.
By systematically addressing each element of the patient’s care needs, healthcare providers can create a personalized plan that promotes healing and supports long-term well-being. A well-crafted treatment plan also ensures that both the patient and provider are aligned in their approach to managing health concerns effectively.
Common Mistakes in SOAP Note Writing
Accurate documentation is crucial in healthcare, as it serves as the foundation for clinical decisions, patient care, and communication among the healthcare team. However, errors in writing clinical records can lead to confusion, misdiagnoses, and suboptimal treatment plans. Understanding and avoiding common mistakes in documentation is key to maintaining high standards of patient care and ensuring the integrity of medical records.
Some of the most frequent mistakes in clinical record writing include:
- Vague or Incomplete Information: Omitting essential details or providing unclear descriptions of the patient’s symptoms, medical history, or physical findings can hinder accurate assessment and diagnosis.
- Failure to Document Objective Data: Relying solely on subjective reports without including measurable or observable data makes it difficult to track patient progress and can lead to inaccuracies in treatment decisions.
- Overgeneralization: Using broad or ambiguous terms without specifying the exact condition or symptoms can lead to confusion or misunderstanding by other healthcare providers.
- Inconsistent Terminology: Mixing up terms or using non-standard language can complicate communication and make it difficult to understand the patient’s condition or the plan of care.
- Not Updating the Record: Failing to update clinical notes after follow-up appointments, tests, or changes in the patient’s condition can result in outdated or incomplete information.
- Neglecting to Include Follow-up Plans: Omitting the next steps for monitoring or treatment plans can leave gaps in patient care and cause delays in necessary interventions.
To prevent these mistakes, healthcare providers should adhere to best practices in documentation, focusing on clarity, accuracy, and completeness. Ensuring that all relevant findings are recorded, using standardized language, and regularly updating patient records can significantly improve the quality of care and reduce the risk of errors.
Best Practices for Detailed Documentation
Accurate and thorough documentation is an essential aspect of effective patient care. It not only ensures clear communication between healthcare providers but also serves as a legal record of patient interactions and treatments. Following best practices for detailed documentation can help prevent errors, enhance patient outcomes, and ensure that clinical records are both complete and reliable.
To maintain high standards of documentation, healthcare professionals should consider the following best practices:
- Be Clear and Concise: Avoid ambiguity and unnecessary jargon. Use precise language to describe the patient’s condition, symptoms, and any procedures performed. This helps to ensure that the information is easily understood by other members of the care team.
- Include Relevant Details: Document all pertinent information, such as the patient’s medical history, current symptoms, test results, and any changes in condition. This provides a comprehensive view of the patient’s health status.
- Use Standardized Terminology: To ensure consistency and reduce the risk of misunderstandings, use universally accepted medical terms and classifications. Standardized language helps maintain clarity and accuracy across different healthcare settings.
- Document in Real-Time: Write down observations and findings as soon as possible after patient interactions. This prevents forgetting critical details and ensures that the documentation is as accurate as possible.
- Ensure Objectivity: Stick to facts and objective data when documenting patient conditions. Avoid inserting personal opinions or assumptions, as this could lead to misinterpretation and impact patient care.
- Be Thorough: Don’t leave out key information, such as follow-up plans, patient reactions, or any special considerations. Detailed documentation ensures that all relevant aspects of care are captured and can be referenced in the future.
- Review and Revise: Regularly review the documentation for accuracy and completeness. Correct any errors promptly and update any outdated information to maintain the integrity of the medical record.
By adhering to these best practices, healthcare providers can ensure that their documentation is not only accurate but also serves as a valuable tool for ongoing patient care. Clear, comprehensive, and timely records improve communication, reduce the risk of errors, and help deliver optimal care to patients.
Confidentiality and Legal Considerations
In the healthcare field, maintaining patient confidentiality and adhering to legal standards is of utmost importance. Healthcare providers are entrusted with sensitive information, and safeguarding this data is essential to ensure trust between patients and medical professionals. Failure to respect privacy and comply with legal requirements can lead to significant legal consequences, including penalties and loss of credibility.
When documenting patient information, several key principles must be followed to protect confidentiality and ensure compliance with legal requirements:
- Patient Privacy: All patient records should be treated as confidential. Information should only be shared with individuals who are directly involved in the patient’s care and with the patient’s explicit consent, where applicable.
- Secure Storage of Records: Both physical and electronic records must be stored securely to prevent unauthorized access. Healthcare organizations should implement measures such as password protection, encryption, and restricted access to ensure the integrity and confidentiality of patient data.
- Informed Consent: Patients should be fully informed about the purposes for which their information will be used. This includes explaining how their data will be documented and shared within the healthcare system. Consent should be obtained before any information is recorded or shared.
- Compliance with Laws: Healthcare providers must comply with relevant privacy laws, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States, which outlines strict guidelines for handling patient information. These laws ensure that patient data is collected, stored, and shared in a manner that protects patient rights and confidentiality.
- Minimization of Data: Only the necessary information should be documented and shared. Avoid unnecessary details that could compromise patient privacy or lead to potential misuse of personal data.
- Regular Training: Healthcare staff should receive regular training on confidentiality, privacy policies, and legal regulations to ensure compliance and promote a culture of respect for patient privacy.
By adhering to these principles, healthcare professionals can protect patient privacy, uphold trust, and minimize the risk of legal issues. Proper documentation practices not only ensure compliance with the law but also contribute to the overall quality of care and the reputation of healthcare institutions.
How to Structure SOAP Notes Effectively
Creating well-structured and organized patient documentation is essential for clear communication and effective care delivery. A logical and consistent format ensures that critical information is captured in a way that is easy to understand, review, and reference. Effective documentation helps healthcare providers make informed decisions, track patient progress, and communicate accurately with other members of the healthcare team.
To structure patient records effectively, it is important to follow a systematic approach. Here are the key steps to consider when creating thorough and organized entries:
- Start with the Subjective Information: Begin by recording the patient’s reported symptoms, concerns, and relevant history. This section should reflect the patient’s perspective and include key details such as the onset of symptoms, severity, duration, and any factors that affect the condition. It is essential to listen carefully and document precisely what the patient communicates.
- Include Objective Findings: The objective section should contain measurable, observable data gathered through physical examination, diagnostic tests, or other clinical observations. This could include vital signs, lab results, imaging findings, or any other relevant facts that can help assess the patient’s condition.
- Provide an Assessment: This section summarizes the healthcare provider’s interpretation of the patient’s condition based on the subjective and objective data. It should include a clear diagnosis or differential diagnosis and an explanation of the clinical reasoning behind the assessment.
- Outline the Plan: The plan section should detail the proposed next steps in the patient’s care. This includes any treatments, tests, referrals, follow-up appointments, and patient education. It should be clear, actionable, and aligned with the patient’s healthcare goals.
By following this structured approach, healthcare professionals can ensure that all relevant aspects of patient care are captured comprehensively. A well-organized record not only improves patient outcomes but also facilitates collaboration among care providers and ensures consistency in the treatment process.
Using SOAP Notes for Patient Follow-Up
Effective follow-up care is crucial in ensuring patients receive the best possible outcomes. Documentation plays a central role in the follow-up process, helping healthcare providers track patient progress, evaluate the effectiveness of treatments, and adjust care plans as needed. Structured records allow clinicians to quickly review prior visits, identify changes in condition, and make informed decisions about next steps in treatment.
SOAP-based documentation serves as an excellent tool for follow-up assessments. By clearly organizing patient information into specific categories, healthcare providers can ensure that important details are not overlooked during follow-up visits. The structured format helps maintain continuity of care while also improving communication across different healthcare teams.
Tracking Changes in Patient Condition
For follow-up visits, it is essential to compare the current state of the patient with previous assessments. The subjective section allows patients to report any changes in symptoms, while the objective section highlights any new findings. By referencing previous records, healthcare providers can determine whether the treatment plan is effective or needs modification. It also helps identify potential complications early, facilitating prompt intervention.
Setting New Goals and Adjusting Care Plans
Follow-up documentation not only tracks progress but also plays an essential role in adjusting care plans. The assessment section allows providers to evaluate the ongoing effectiveness of treatments and set new goals based on current patient needs. In the plan section, providers can outline adjustments to medications, therapies, or lifestyle recommendations, ensuring the patient is supported with the most up-to-date care plan.
By using structured records for follow-up, healthcare professionals can foster better patient engagement, track treatment progress efficiently, and improve long-term health outcomes. This process enhances both the quality of care and the patient experience, contributing to an overall more organized and effective healthcare system.
Integrating SOAP Notes into Electronic Systems
As healthcare continues to move towards digital solutions, the integration of structured documentation into electronic systems is becoming increasingly important. Electronic health records (EHRs) provide a seamless way to store and retrieve patient data, improving accessibility, communication, and decision-making. Structured documentation formats, such as those used for patient assessments, are essential for ensuring that key information is consistently recorded and easily accessible.
Incorporating structured patient records into electronic systems allows for greater efficiency and accuracy in documenting healthcare encounters. By using standardized templates, healthcare professionals can quickly enter relevant details about a patient’s condition, history, and treatment plan. This also allows for easy updates during follow-up visits and ensures that critical information is not missed or lost in the process.
One of the key advantages of integrating structured documentation into electronic systems is improved data sharing. With digital records, healthcare providers can easily share patient information across different departments, facilitating collaboration and enhancing patient care. This integration also supports automated decision-making tools that can provide real-time alerts and suggestions based on the documented data, helping clinicians make more informed decisions.
Furthermore, the use of electronic documentation systems enhances the security and confidentiality of patient data. These systems typically come with built-in encryption and access controls, ensuring that only authorized personnel can view or modify patient information. This level of security helps healthcare providers comply with legal and regulatory standards while maintaining patient trust.
Overall, integrating structured documentation formats into electronic health records systems enhances the quality, efficiency, and security of healthcare delivery. By streamlining the documentation process, healthcare professionals can focus more on patient care and less on administrative tasks, leading to better patient outcomes and a more effective healthcare system.
Training Healthcare Providers in SOAP Notes
Effective documentation is a critical skill for healthcare providers, ensuring accurate and comprehensive patient records that enhance care delivery. Training healthcare professionals to document patient encounters using structured formats is essential for maintaining high standards of care. Clear, concise, and consistent documentation ensures that important details about patient conditions, treatment plans, and progress are readily available to all team members involved in the patient’s care.
Healthcare providers must be trained to effectively use structured documentation formats that capture relevant information systematically. This includes understanding how to organize patient data into distinct sections, ensuring that subjective experiences, objective findings, assessments, and plans are clearly identified. Training should emphasize the importance of including all necessary details without omitting key information that could affect diagnosis or treatment.
Additionally, training should include familiarization with the tools and software used to input data into electronic health records (EHRs). Providers need to be comfortable navigating these systems, ensuring that their documentation is entered efficiently and accurately. Familiarity with EHRs helps reduce errors and improves the overall quality of patient records.
To ensure healthcare providers are consistently following best practices, regular workshops and refresher courses are valuable. These training sessions should focus on real-world scenarios, allowing providers to practice documenting patient encounters using structured formats. Feedback from peers and supervisors can further refine documentation skills, ensuring that all members of the healthcare team are on the same page when it comes to patient care.
Ultimately, thorough training in structured documentation leads to improved communication among healthcare teams, better patient outcomes, and enhanced legal compliance. As healthcare systems continue to evolve, training providers in best practices for documentation will remain an essential part of ensuring effective, safe, and high-quality care.
Improving Patient Care with SOAP Notes
Effective documentation plays a crucial role in enhancing patient care by ensuring clear communication between healthcare providers. A well-structured system of documenting patient interactions can help improve diagnosis, treatment planning, and follow-up care. By organizing patient information into distinct categories, healthcare providers can make more informed decisions, ultimately leading to better outcomes and a higher standard of care.
Enhancing Communication Among Care Teams
One of the most significant benefits of using structured documentation formats is the improvement in communication between different members of the healthcare team. By clearly outlining the patient’s symptoms, findings, assessments, and treatment plans, all healthcare providers involved in the patient’s care can stay informed and provide more coordinated treatment. This eliminates misunderstandings and ensures that each team member is aware of the patient’s current condition and treatment goals.
Ensuring Comprehensive Patient Records
Structured documentation also ensures that all aspects of the patient’s care are recorded, reducing the likelihood of important information being overlooked. By breaking down the encounter into separate sections, healthcare providers can ensure that no detail is missed, whether it is a symptom reported by the patient, an objective finding from a physical examination, or a planned course of action. This comprehensive record-keeping is essential for tracking patient progress over time and for making adjustments to treatment as needed.
Key Benefits of Structured Documentation
- Improved diagnosis: Clear documentation helps identify patterns and trends that might otherwise be missed.
- Faster decision-making: Organized records allow for quick access to relevant patient information, leading to faster clinical decisions.
- Increased patient safety: A thorough record reduces the risk of medication errors or miscommunication about treatment plans.
- Better follow-up care: Clear documentation ensures that important details are carried over during follow-up visits, promoting continuity of care.
Ultimately, the use of a structured documentation system fosters better collaboration, ensures that all relevant patient information is captured, and improves the overall quality of care. It supports healthcare providers in delivering timely, accurate, and effective treatment that benefits the patient at every stage of their care journey.