
Accurate evaluation of the upper limb is crucial in diagnosing a wide range of musculoskeletal conditions. This process involves a combination of hands-on techniques and tests that help healthcare professionals determine the root cause of pain, weakness, or limited mobility. By understanding the various steps involved, practitioners can improve their diagnostic accuracy and provide better care to their patients.
Effective examination begins with a thorough understanding of anatomy and common injuries that affect the region. Evaluating joint stability, muscle strength, and the presence of inflammation or structural damage is essential for identifying the correct condition. Specialized tests, along with physical maneuvers, can highlight underlying issues that may not be immediately obvious through basic observation alone.
Mastering these evaluation techniques is vital for clinicians in ensuring appropriate treatment plans and timely interventions. Whether it’s managing acute injuries or chronic conditions, a detailed and systematic approach plays a key role in achieving favorable patient outcomes. It’s important for practitioners to continually refine their skills to stay ahead of emerging trends and techniques in musculoskeletal care.
Upper Limb Assessment Overview
Performing a comprehensive evaluation of the upper extremity is essential for diagnosing a wide range of conditions. This process combines physical techniques and diagnostic tests to assess joint function, muscular strength, and any signs of injury or pathology. A thorough examination helps identify the root cause of discomfort, dysfunction, or pain, allowing for effective treatment planning.
In this section, we will explore the various steps involved in the upper limb evaluation process, focusing on key diagnostic maneuvers and tests that can uncover potential issues. Whether it’s assessing for joint instability, impingement, or muscle imbalances, a systematic approach is critical for accurate assessment. These tests not only help in identifying conditions but also aid in determining the severity of the injury or dysfunction.
Mastering the evaluation of the upper extremity is vital for healthcare professionals who manage musculoskeletal disorders. Understanding the techniques involved and when to apply them is crucial for providing optimal care. This overview provides the foundation for a more detailed examination of specific diagnostic methods used to evaluate the upper limb’s function and integrity.
Understanding Upper Limb Examination Techniques
Effective assessment of the upper extremity involves a combination of manual maneuvers and clinical tests designed to identify abnormalities. A detailed understanding of these techniques allows healthcare providers to systematically evaluate the region, detect potential issues, and diagnose conditions that affect joint function, stability, and mobility. These methods are essential for identifying everything from simple sprains to complex structural injuries.
Key Techniques for Comprehensive Evaluation
There are several fundamental approaches used in the examination process, each targeting specific areas of concern. These techniques generally include the following:
- Palpation: Used to detect tenderness, swelling, and abnormalities in bone or soft tissue.
- Range of Motion Testing: Assesses flexibility and joint movement through active and passive motions.
- Strength Testing: Evaluates muscle function and the ability to resist force during specific movements.
- Special Tests: Specific maneuvers designed to pinpoint conditions like impingement or instability.
When to Apply These Techniques
These examination techniques are applied at different stages of the clinical evaluation, depending on the patient’s symptoms and medical history. For instance:
- Initial Assessment: Focuses on palpation and range of motion to get an overview of the condition.
- Targeted Evaluation: Special tests are employed once a general understanding of the injury is obtained.
- Functional Testing: Strength and stability tests are critical for identifying more subtle issues or assessing recovery progress.
By mastering these techniques, clinicians can ensure a more accurate diagnosis and tailor their treatment approach to each individual patient’s needs.
Key Components of the Upper Limb Assessment
A thorough evaluation of the upper extremity requires a systematic approach that covers multiple aspects of joint and soft tissue function. The goal is to identify any areas of dysfunction, instability, or injury that may be impacting movement and strength. This assessment involves both visual inspection and hands-on techniques, each targeting specific concerns related to mobility, muscle performance, and joint health.
Essential Elements of the Assessment
Several key components contribute to a comprehensive examination, helping practitioners gather important data about the patient’s condition:
- Inspection: Observing the affected area for signs of swelling, bruising, deformity, or asymmetry.
- Palpation: Gently feeling the region for tenderness, warmth, or any abnormal masses in the muscles, tendons, or joints.
- Range of Motion Testing: Evaluating the flexibility and mobility of the joint through active and passive movements.
- Strength Testing: Assessing the muscle’s ability to resist external forces, often done in specific positions to isolate muscle groups.
Advanced Diagnostic Maneuvers
In addition to basic techniques, more specialized tests are used to evaluate specific conditions that may not be immediately obvious. These can include:
- Specialized Joint Tests: Such as maneuvers to detect instability, impingement, or labral tears.
- Functional Movement Screening: Observing how the patient moves in functional tasks to identify limitations in motion or strength.
Each of these components is essential for gathering a complete picture of the patient’s condition, ensuring that treatment decisions are based on accurate and thorough information.
Common Upper Limb Injuries and Symptoms
The upper extremity is susceptible to a variety of injuries, ranging from acute trauma to chronic overuse conditions. These injuries can affect the joints, muscles, tendons, and ligaments, leading to pain, weakness, and limited mobility. Recognizing the symptoms and understanding the most common injuries is essential for providing appropriate treatment and rehabilitation.
Frequent Injuries in the Upper Limb
Several types of injuries are commonly seen in the upper extremity, including:
- Rotator Cuff Tears: Damage to the group of muscles and tendons that stabilize the joint, often leading to pain and weakness.
- Impingement Syndrome: Occurs when tendons in the area are irritated or compressed, causing pain during overhead movements.
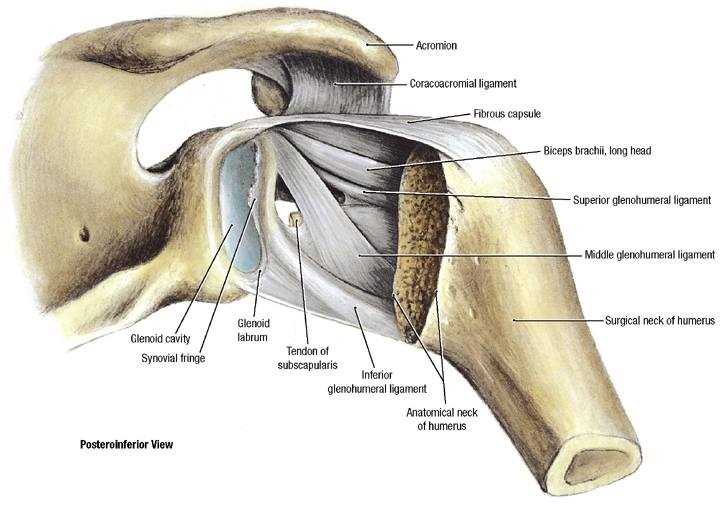
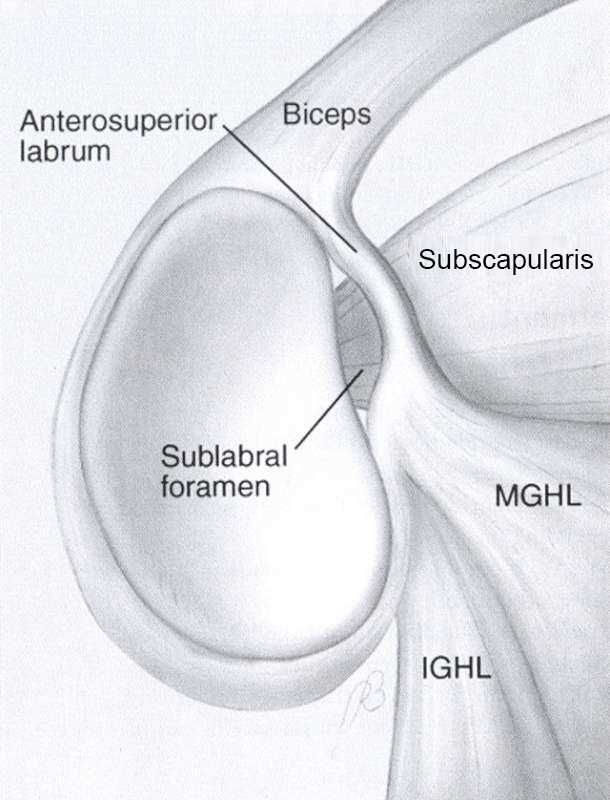
- Labral Tears: Injury to the cartilage that stabilizes the joint, which can lead to instability and pain.
- Fractures: Broken bones, such as the collarbone or upper arm, that typically result from falls or direct impact.
- Tendinitis: Inflammation of the tendons, often caused by repetitive motions or overuse.
Common Symptoms to Watch For
Injuries to the upper extremity often present with a range of symptoms, which can help guide diagnosis:
- Pain: Typically worsens with movement or specific activities, especially those involving lifting or overhead motions.
- Swelling and Bruising: Indicating trauma or inflammation in the affected area.
- Weakness: Difficulty in performing everyday tasks or movements due to compromised muscle function.
- Limited Range of Motion: Stiffness or discomfort when attempting to move the arm in certain directions.
Identifying these injuries early and understanding their symptoms can significantly impact the effectiveness of treatment and recovery. Proper diagnosis is crucial for determining the best course of action and preventing long-term complications.
Performing the Physical Examination Steps
Conducting a physical assessment of the upper limb is a crucial process in diagnosing musculoskeletal conditions. It involves several systematic steps aimed at evaluating the function, strength, and overall health of the affected area. By following these steps, healthcare providers can effectively identify the source of pain, weakness, or instability and develop an appropriate treatment plan.
Steps in the Physical Assessment
The process typically unfolds in a sequence of actions that allow for a thorough evaluation of the limb’s condition:
- Initial Observation: Begin by visually examining the limb for any deformities, swelling, bruising, or asymmetry, which can provide clues about the underlying issue.
- Palpation: Gently palpate the area to assess for tenderness, warmth, or abnormal bumps, which can suggest inflammation or injury to specific structures.
- Range of Motion Testing: Check the joint’s ability to move freely through its natural range, both actively (patient-driven) and passively (examiner-assisted).
- Strength Assessment: Evaluate muscle strength by testing the patient’s ability to resist applied force during specific movements.
- Specialized Tests: Perform targeted diagnostic maneuvers to assess for conditions like instability, tendon damage, or impingement, which may not be apparent during the initial steps.
Techniques for Accurate Diagnosis
Within each step, various techniques are used to gather precise information about the injury or condition:
- Active Movement Observation: Observe the patient as they move their arm through specific ranges to identify limitations or discomfort.
- Resisted Movement Testing: Ask the patient to resist force applied by the examiner to assess the strength of individual muscle groups.
- Stability Tests: Use specialized maneuvers to evaluate the integrity of the joint and the surrounding ligaments.
- Joint Compression/Distraction: Techniques to assess the condition
Palpation Techniques for Upper Limb Diagnosis
Palpation is a critical step in the physical examination process, allowing healthcare providers to assess the condition of muscles, joints, tendons, and ligaments. This hands-on approach helps identify areas of tenderness, swelling, or abnormal texture, providing valuable clues about the underlying issue. By systematically palpating different structures, clinicians can narrow down the possible causes of pain and discomfort.
During the examination, specific palpation techniques are employed to ensure a thorough evaluation of the affected area. These techniques can help detect inflammation, muscle strains, tendonitis, and other conditions that may not be immediately visible. Below is a summary of key palpation methods used in upper limb assessments.
Palpation Technique Target Area Purpose Superficial Palpation Skin and soft tissues To identify areas of swelling, warmth, or bruising caused by injury or inflammation. Deep Palpation Muscles and tendons To assess for tenderness, muscle spasms, or abnormal masses in deeper tissues. Joint Line Palpation Joint spaces To detect joint effusion, tenderness, or abnormalities like cartilage damage or instability. Crepitus Detection Joint or tendons To feel for abnormal sounds or sensations indicating damage to cartilage or tendons. Each of these techniques is designed to provide specific information about the tissues being assessed, helping clinicians to determine the next steps in the diagnostic process. By combining palpation with other evaluation methods, a clearer picture of the patient’s condition can be obtained, leading to more accurate treatment decisions.
Testing Range of Motion in the Upper Limb
Evaluating the range of motion (ROM) of the arm is an essential component of the diagnostic process, as it helps determine the extent to which the limb can move in various directions. This assessment is crucial in identifying any restrictions, stiffness, or pain that may be present during movement. By observing both active and passive movements, healthcare providers can gather important information about the mobility and health of the joint and surrounding tissues.
ROM tests are typically divided into active and passive categories. Active ROM involves the patient moving the arm independently, while passive ROM involves the examiner moving the arm for the patient. These evaluations help detect issues such as joint instability, muscle weakness, or potential injury to ligaments and tendons. A comprehensive assessment of movement can highlight any abnormal patterns or limitations, aiding in the diagnosis of musculoskeletal conditions.
Test Type Movement Assessed Purpose Active ROM Patient moves the arm through various motions. Evaluates the patient’s ability to move the limb independently and identifies pain or movement restrictions. Passive ROM Examiner moves the arm for the patient. Helps assess joint flexibility and detects restrictions or pain that the patient cannot actively demonstrate. Resisted ROM Patient resists examiner’s movement of the arm. Assesses muscle strength and identifies any weakness or discomfort under resistance. End Feel Testing Determines the sensation at the endpoint of movement. Detects abnormal end-feels such as spasm or hard stops, which may indicate underlying joint or soft tissue issues. By performing these tests, healthcare providers can better understand the functional capacity of the upper limb and identify potential sources of pain or dysfunction. This information is vital in formulating an effective treatment and rehabilitation plan for the patient.
Special Tests for Rotator Cuff Pathology

When assessing damage to the muscles and tendons around the upper limb’s primary joint, specific clinical tests are crucial for identifying potential issues with the rotator cuff. These specialized tests are designed to provoke symptoms and reveal underlying injuries or dysfunctions, such as tears, tendinopathy, or impingement. A comprehensive approach using these tests helps clinicians pinpoint the source of pain and determine the best course of action for treatment.
Each test targets different aspects of rotator cuff function, such as strength, movement patterns, and pain response. Performing these tests allows for a more detailed understanding of the patient’s condition, aiding in the differentiation of various musculoskeletal pathologies that may present with similar symptoms.
Commonly Used Tests
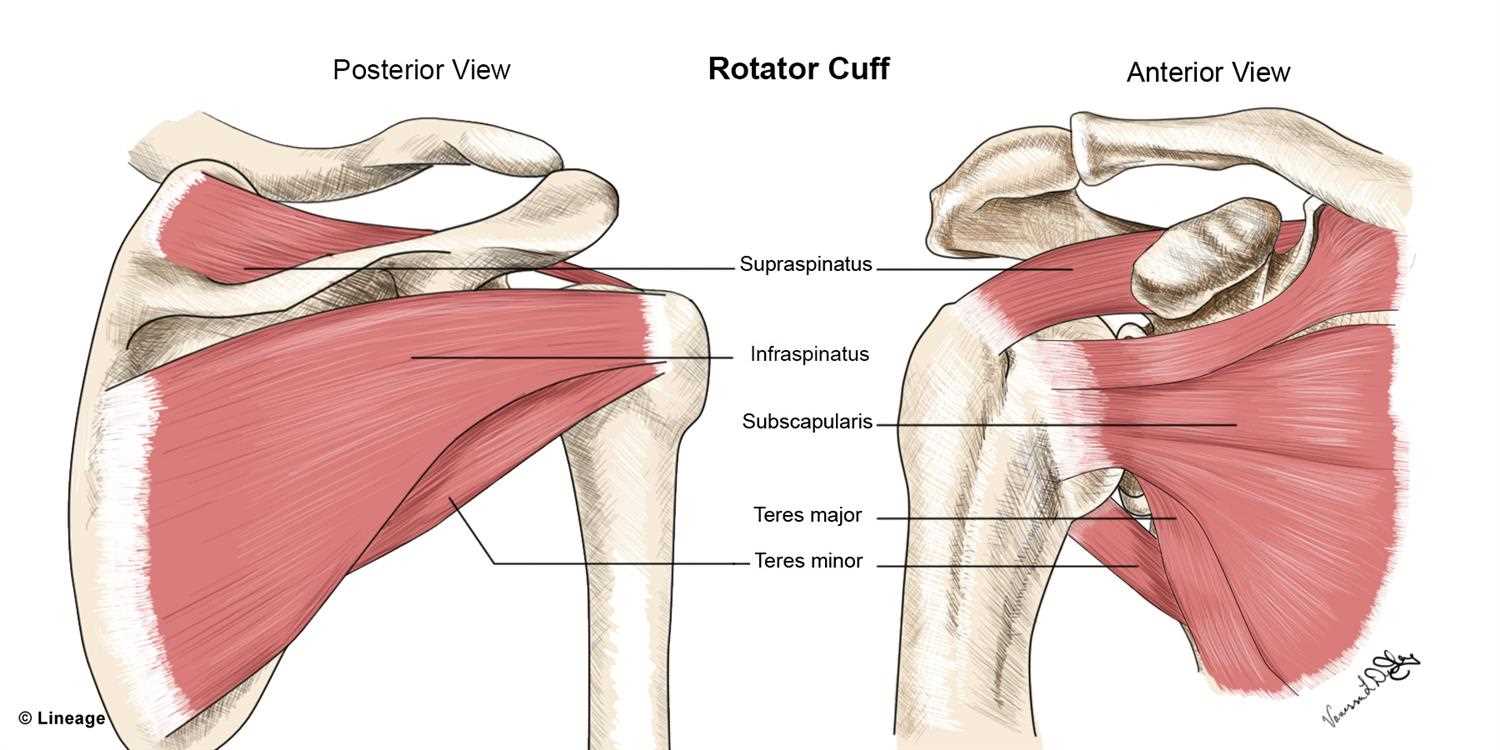
- Neer’s Test: This test involves raising the arm while the examiner stabilizes the scapula, assessing for pain or discomfort indicative of impingement or rotator cuff tears.
- Hawkins-Kennedy Test: A commonly used test to identify impingement of the rotator cuff tendons, particularly the supraspinatus tendon, by forcibly rotating the arm.
- Empty Can Test: The patient elevates the arm to 90 degrees in the scapular plane while the examiner applies downward pressure. This test evaluates the integrity of the supraspinatus tendon.
- Drop Arm Test: This test assesses the integrity of the rotator cuff muscles, particularly the supraspinatus, by having the patient lower their arm from a fully abducted position. Pain or difficulty in lowering the arm may indicate a tear.
- External Rotation Lag Sign: Used to test the infraspinatus and teres minor tendons, this test involves holding the arm in external rotation and assessing for lag or inability to maintain the position.
How These Tests Aid in Diagnosis
By performing these specialized tests, clinicians can evaluate the condition of the rotator cuff and determine the severity of the injury. Positive results from multiple tests help confirm a diagnosis and guide further imaging or treatment interventions. While these tests are not conclusive on their own, they provide valuable insights that help in the overall clinical assessment and decision-making process.
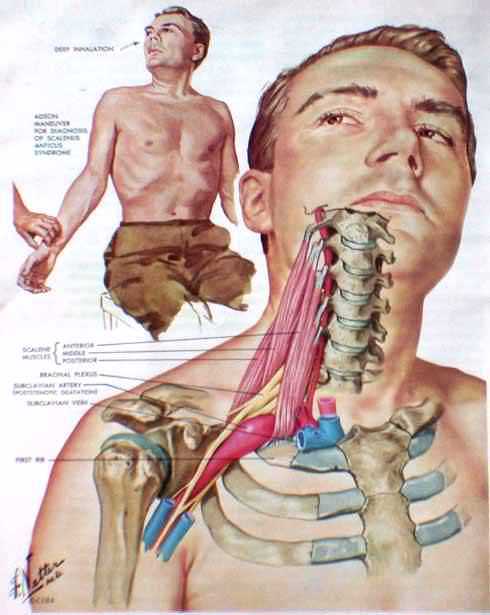
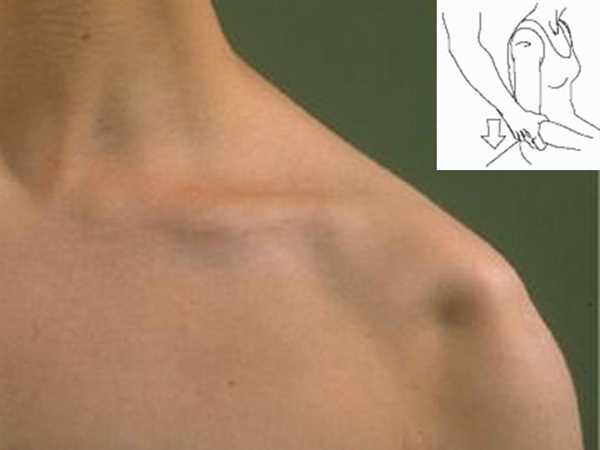
Assessing Joint Instability and Dislocations

Evaluating joint instability and the risk of dislocations is a key aspect of musculoskeletal assessments. Instability in the upper limb’s primary joint can lead to a range of symptoms, from pain and weakness to a feeling of the joint “slipping” or “giving way.” Dislocations, which involve the displacement of the joint surfaces, often occur due to trauma or repeated stress, and can severely impair function. Early recognition of these issues is essential to prevent further damage and to guide appropriate treatment.
Clinicians rely on a combination of physical tests, patient history, and imaging to assess the degree of instability. By performing these tests, they can determine whether the joint is prone to dislocations or subluxations, which occur when the joint partially slips out of place. A thorough evaluation helps identify any underlying structural abnormalities or weaknesses that may contribute to joint instability.
Common Tests for Joint Instability:
- Apprehension Test: This test assesses the stability of the anterior joint capsule by applying pressure and rotation to the joint. A positive result is marked by discomfort or the patient’s apprehensive response, indicating potential instability or a history of dislocations.
- Relocation Test: Often performed after the apprehension test, this test involves applying a posterior force to the joint to see if it alleviates discomfort. It helps confirm anterior instability or a previous dislocation event.
- Sulcus Sign: This test assesses inferior instability by pulling the arm downward while observing for a visible indentation beneath the acromion. A positive sign suggests instability in the joint’s lower region.
- Load and Shift Test: Used to evaluate the degree of both anterior and posterior instability, this test involves applying force to the humeral head to assess how much it moves within the joint socket.
By using these diagnostic techniques, healthcare providers can effectively assess the degree of instability and help prevent recurrent dislocations or further damage. Addressing instability early on is crucial for reducing the risk of long-term complications, such as joint degeneration or chronic pain.
Impingement Tests in Joint Evaluation
Impingement is a common cause of pain in the upper limb’s primary joint, often resulting from the compression or irritation of soft tissues such as tendons or bursa. This condition typically arises when these structures become trapped between the bone surfaces during movement. Proper diagnosis is essential for managing impingement and preventing further tissue damage. Specific clinical tests are used to identify impingement, aiding healthcare professionals in determining the most appropriate treatment approach.
These diagnostic tests are designed to provoke the symptoms associated with impingement, such as pain or restricted motion. By replicating movements that stress the affected areas, these tests help identify the presence of inflammation or structural abnormalities in the joint’s soft tissues.
Key Impingement Tests
- Neer’s Test: This test involves passively raising the arm while stabilizing the scapula, aiming to compress the tendons beneath the acromion. Pain during this movement is indicative of impingement, particularly affecting the rotator cuff tendons.
- Hawkins-Kennedy Test: This test assesses for impingement by bringing the arm into 90 degrees of flexion and internally rotating it. Discomfort or pain during this motion suggests the presence of tendon irritation or narrowing of the subacromial space.
- Jobe’s Test (Empty Can Test): In this test, the arm is positioned in the scapular plane and the examiner applies downward pressure while the patient resists. Pain or weakness during this test suggests a problem with the supraspinatus tendon, a common site of impingement.
Importance of Impingement Tests
These tests help differentiate impingement from other causes of joint pain and dysfunction. By confirming the presence of impingement, clinicians can recommend treatments that target the root cause, such as physical therapy, corticosteroid injections, or, in severe cases, surgery. Identifying the specific site of impingement is crucial for effective management and recovery.
Identifying Labral Tears During Examination
Labral tears are a common cause of joint instability and discomfort, often resulting from trauma or repetitive strain. These tears involve the cartilage that helps to stabilize the joint by securing the head of the bone within the socket. Detecting labral tears requires careful assessment using specific physical tests that aim to reproduce symptoms and identify potential damage to the cartilage. These tests are crucial for guiding treatment decisions and determining the need for further imaging or surgical intervention.
Clinicians often rely on a combination of patient history, physical examination, and diagnostic tests to pinpoint the presence of a labral tear. The most effective way to identify this injury is through special maneuvers designed to stress the joint in ways that reveal instability or pain associated with cartilage damage.
Common Tests to Detect Labral Tears

- O’Brien’s Test: The patient’s arm is positioned in front of them with the elbow straight and the palm facing up. The examiner then applies downward pressure while the patient resists. Pain or clicking felt during this maneuver suggests a possible labral tear.
- Crank Test: This test involves rotating the arm in a particular way while maintaining a specific level of pressure. Reproduction of pain or mechanical symptoms, such as catching or popping, is indicative of a labral tear.
- Anterior Apprehension Test: This test focuses on the anterior aspect of the joint. The arm is placed in a position that typically causes dislocation. If the patient shows signs of discomfort or apprehension, it may suggest damage to the labrum.
- Joint Line Tenderness: Palpation of the joint line may reveal localized tenderness, which can point to a tear in the labral cartilage, especially when combined with other symptoms or test results.
Early identification of a labral tear is essential for minimizing long-term damage. While physical tests are valuable in the diagnostic process, they are often supplemented with imaging studies, such as MRI or CT arthrograms, for a definitive diagnosis. Proper management can involve conservative treatments like physical therapy or more invasive interventions like arthroscopy, depending on the severity of the injury.
Shoulder Examination in Traumatic Injuries
Traumatic injuries to the upper limb often result in significant pain, instability, and limited mobility. Proper assessment of the affected area is essential to identify the underlying pathology and develop an appropriate treatment plan. The process involves a systematic evaluation that aims to rule out fractures, dislocations, and soft tissue damage, while also considering the mechanism of injury and the patient’s clinical presentation.
In traumatic cases, rapid and thorough assessment is crucial for timely intervention. A detailed history of the injury, including the forces involved, direction of impact, and patient symptoms, is integral to understanding the nature of the injury. The physical examination is focused on identifying the extent of tissue damage, joint stability, and the presence of any deformities or functional limitations.
Key Steps in the Examination
- Initial Inspection: Observe the injured area for any obvious deformities, swelling, bruising, or asymmetry. Signs of dislocation or fractures may be visible or palpable during this phase.
- Palpation: Gently palpate the affected region to assess tenderness, crepitus, or abnormal movement. Pay special attention to the joint line and surrounding soft tissues, as tenderness in specific areas may indicate ligament or tendon damage.
- Range of Motion (ROM) Testing: Carefully assess the range of motion in the joint. Restricted or painful movement can help determine the extent of the injury and whether there is a structural issue like ligament tears or muscle strains.
Diagnostic Maneuvers
- Apprehension and Relocation Test: This maneuver helps assess joint stability, particularly after dislocation or subluxation. It involves placing the joint in a position of vulnerability and applying pressure to determine if the patient experiences apprehension or discomfort.
- Compression and Distraction Tests: These tests help identify fractures or joint instability by applying compressive and distractive forces to the injured area. Pain or a change in symptoms during these tests may suggest a specific type of injury.
In cases of traumatic injuries, it is important to follow the physical examination with appropriate imaging studies, such as X-rays or MRI, to confirm the diagnosis and rule out fractures or more complex soft tissue injuries. Early detection of these conditions is critical for preventing further damage and ensuring optimal recovery.
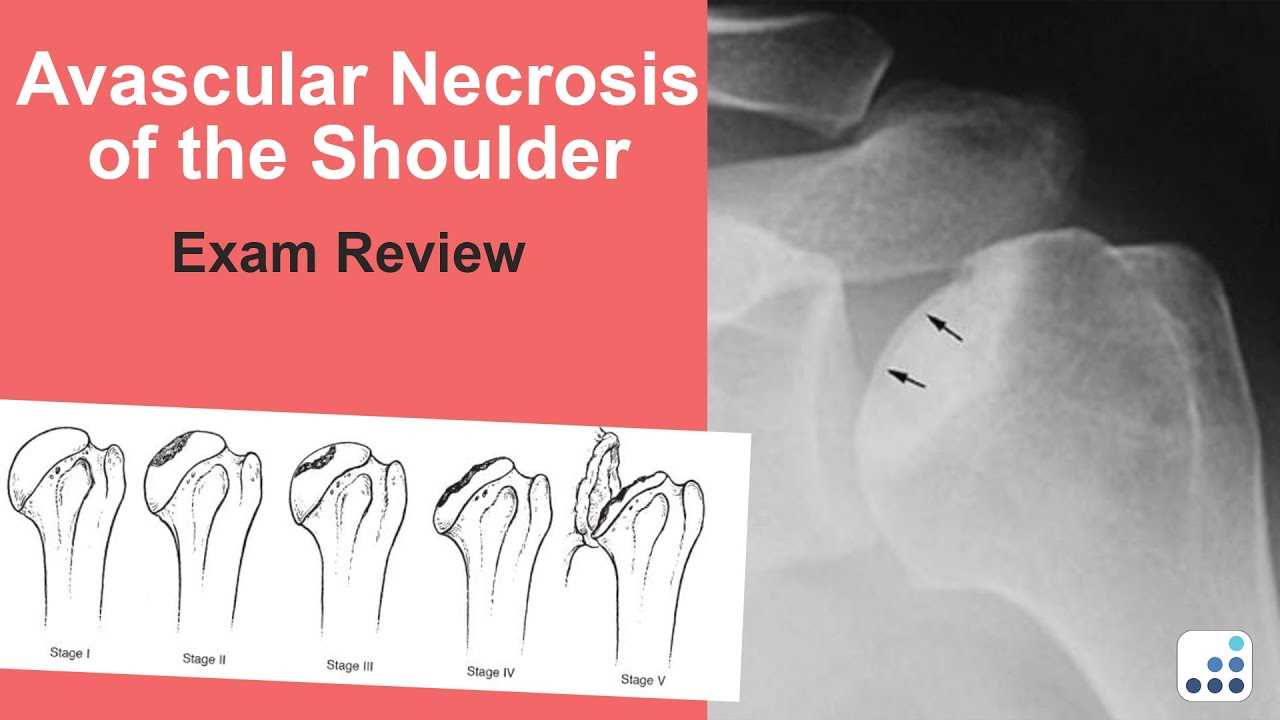
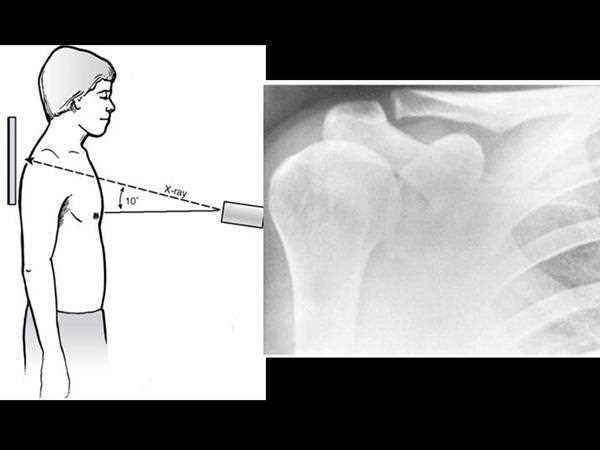
Using Imaging to Support Shoulder Diagnosis
Imaging plays a vital role in confirming the diagnosis of musculoskeletal injuries, particularly when physical examination alone does not provide sufficient information. It enables clinicians to visualize internal structures, detect fractures, assess soft tissue damage, and evaluate joint integrity. With advancements in diagnostic imaging, tools such as X-rays, MRI, and ultrasound have become invaluable in diagnosing injuries and guiding treatment decisions.
Imaging techniques help identify both acute and chronic conditions, providing detailed insights into bone and soft tissue abnormalities. These tools are essential for confirming suspicions raised during the clinical examination and for ruling out more complex pathologies that may not be apparent through physical tests alone.
Common Imaging Modalities
- X-ray: A primary imaging tool for detecting fractures, dislocations, and joint alignment issues. It is often the first choice when assessing acute injuries or trauma to the upper limb.
- Magnetic Resonance Imaging (MRI): This technique offers a detailed view of soft tissues, including muscles, tendons, ligaments, and cartilage. It is crucial for diagnosing tears, strains, or inflammation in soft tissues.
- Ultrasound: A dynamic imaging tool that is useful for evaluating soft tissue conditions, such as tendonitis or muscle tears. It can also be used to guide injections or aspirations.
When to Use Imaging
- Acute Trauma: Imaging is typically ordered following significant trauma to the joint or surrounding tissues to check for fractures, dislocations, or other structural damage.
- Chronic Pain or Dysfunction: In cases of ongoing discomfort, weakness, or limited range of motion, imaging can provide critical information on underlying conditions, such as degenerative diseases or long-standing ligament injuries.
- Pre-surgical Planning: For complex cases requiring surgery, imaging helps surgeons understand the exact nature of the injury, allowing for more precise treatment planning.
Incorporating imaging into the diagnostic process ensures a comprehensive evaluation and improves the accuracy of treatment decisions. It also allows for better monitoring of healing progress and can provide valuable information on any complications that may arise during recovery.
Approach to Shoulder Evaluation
The evaluation of upper limb injuries, particularly those affecting the complex joint structures, requires a systematic and thorough approach. A detailed assessment begins with a comprehensive history, followed by physical examination techniques designed to assess joint mobility, integrity of soft tissues, and strength. This process is critical in identifying pathologies such as rotator cuff tears, labral injuries, or joint instability. The evaluation process must be structured to gather relevant information while ruling out other potential diagnoses.
Key to this approach is a combination of both clinical tests and imaging modalities. The clinical evaluation provides insight into the patient’s condition, while imaging is used to confirm suspicions and identify underlying conditions that may not be detectable during the physical assessment.
Systematic Assessment Strategy
- History Taking: Understanding the patient’s symptoms, including the onset, type, and location of pain, along with any prior injuries, is crucial to guide the assessment.
- Physical Examination: A thorough examination that includes inspection, palpation, range of motion testing, and strength assessments. Special tests are then used to pinpoint specific conditions such as impingement or instability.
- Imaging Studies: In some cases, imaging is used to provide additional information regarding fractures, soft tissue injuries, or joint pathologies that may not be evident on physical exam.
Key Components of the Approach
Step Description History Gathering information on symptoms, injury mechanism, and any previous treatments or conditions. Inspection Assessing visible deformities, muscle wasting, or asymmetry that could indicate underlying pathology. Palpation Identifying areas of tenderness, swelling, or abnormal masses within the joint or surrounding tissues. Range of Motion Testing Evaluating the movement of the joint in all directions to assess flexibility and identify limitations or pain during motion. Diagnostic Challenges in Shoulder Assessments
Accurately diagnosing injuries or conditions related to the upper limb can be particularly challenging due to the complex anatomy of the joint and the overlapping symptoms of various pathologies. Several factors contribute to these challenges, including the patient’s ability to clearly describe symptoms, the subtle nature of certain injuries, and the limitations of physical testing alone. In some cases, conditions may mimic one another, making it difficult to pinpoint the exact source of discomfort without a thorough and methodical evaluation.
Additionally, many musculoskeletal conditions, such as rotator cuff tears, labral tears, or joint instability, can present with similar pain patterns and functional limitations. Without careful assessment and, when necessary, imaging studies, a precise diagnosis may remain elusive. Furthermore, some injuries may present with few outward signs, which can lead to underdiagnosis or misdiagnosis if the examination is not comprehensive.
Key challenges include:
- Symptom Overlap: Many conditions, such as impingement syndrome, tendonitis, and labral tears, can present with similar signs such as pain, weakness, or limited mobility, making it difficult to distinguish between them based solely on physical examination.
- Subtle Injuries: Some injuries, particularly those involving soft tissues like the rotator cuff or labrum, may not be immediately apparent through routine physical tests and may require advanced imaging techniques to confirm.
- Patient Reporting: Patients often struggle to accurately describe their symptoms, which can affect the diagnostic process. Pain location, severity, and the mechanism of injury may be misrepresented, further complicating the diagnosis.
- Limitations of Physical Tests: Certain pathologies, such as labral tears or partial tendon ruptures, may not be easily identifiable through traditional physical examination alone and often require the use of specialized diagnostic tools.
Overcoming these challenges requires a systematic approach that includes a detailed history, thorough physical examination, and, when appropriate, diagnostic imaging. In some cases, it may also be necessary to rely on a combination of clinical findings and patient response to specific tests to accurately identify the underlying condition.
Rehabilitation Considerations Post-Exam
Following a comprehensive evaluation, rehabilitation plays a crucial role in the recovery and long-term function of the affected joint. The approach to rehabilitation depends on the specific diagnosis, the severity of the condition, and the individual’s overall health and activity level. Early intervention is often key to restoring mobility, strength, and stability, but the rehabilitation process should be tailored to the unique needs of each patient.
Initial rehabilitation typically focuses on reducing pain and inflammation while protecting the injured area from further damage. This phase may include modalities such as rest, ice, or anti-inflammatory medications. As pain subsides, the focus shifts to restoring range of motion and strength through controlled, therapeutic exercises designed to improve function without overstressing the tissues.
Key rehabilitation considerations include:
- Gradual Progression: Rehabilitation should progress in stages, starting with gentle movements and exercises, followed by strengthening routines and, eventually, functional drills that mimic daily or sports activities.
- Individualized Plan: A tailored rehabilitation plan is essential, considering the type of injury, age, fitness level, and goals of the patient. Not all individuals recover at the same pace, and a personalized plan ensures that progress is made safely and effectively.
- Strengthening and Stability: Building muscle strength and improving the stability of the joint is critical for preventing future injuries. Exercises that target the surrounding muscles are incorporated to enhance overall support.
- Return-to-Activity Guidelines: Gradual reintroduction to activity should be guided by the patient’s ability to tolerate increased loads and movements without exacerbating pain or discomfort. Specific tests or criteria may be used to determine readiness for full activity.
In some cases, ongoing rehabilitation may be necessary even after the initial recovery phase. Regular follow-up visits can help monitor progress, adjust the rehabilitation plan as needed, and ensure that the individual regains optimal function for daily life or athletic performance.
Improving Skills in Shoulder Examination
Mastering the art of assessing joint and soft tissue function requires a blend of knowledge, practice, and clinical experience. Whether in a clinical or athletic setting, a thorough examination can reveal key insights into the underlying issues affecting mobility, stability, and pain. Building expertise in this area involves honing both technical skills and a deep understanding of anatomical structures and pathology.
Key strategies to improve these assessment skills include:
- Practice and Repetition: Regular practice enhances the accuracy and speed of performing tests. The more frequently a clinician performs the assessment, the more proficient they become in detecting subtle signs of dysfunction.
- Continuous Learning: Staying updated on the latest research and techniques in anatomy, pathology, and diagnostic methods helps to refine assessment approaches. Understanding new theories can improve clinical decision-making and diagnostic accuracy.
- Focused Observation: Developing a keen eye for visual cues during the physical examination–such as asymmetry, swelling, or abnormal movement patterns–is crucial for identifying potential issues early on.
- Feedback and Mentorship: Working with experienced clinicians provides valuable feedback that helps refine technique. Observing more experienced practitioners in action can expose new methods and approaches that might not be immediately apparent.
Improving these skills also requires patience and attention to detail. Consistently applying these strategies will contribute to more accurate diagnoses, improved patient outcomes, and a higher level of clinical competence.