Accurate classification of diagnoses and procedures is essential in the healthcare industry, ensuring proper billing and statistical analysis. Understanding how to assign the correct codes can be challenging, especially when dealing with complex medical conditions. This section provides practical examples designed to enhance your knowledge and skills in this area.
By examining various case studies, you will gain insight into the decision-making process required to select the right codes. Each example presents a unique medical situation, helping you practice the critical thinking needed to navigate complex coding tasks.
Whether you’re just starting or are looking to refine your expertise, these real-world illustrations will guide you through the process. Mastering these techniques will not only improve your accuracy but also boost your confidence when dealing with different patient records and healthcare documentation.
ICD-10-CM Coding Scenarios Explained
Understanding the proper method for assigning the correct diagnosis and procedure codes is crucial in the medical field. This process plays a vital role in ensuring that healthcare providers are reimbursed accurately and that the correct data is recorded for statistical analysis. By examining realistic examples, it becomes easier to grasp the complexities involved in classifying medical conditions and procedures accurately.
Breaking Down Complex Medical Situations
Each medical situation requires careful attention to detail when selecting the appropriate codes. Even seemingly straightforward cases can involve nuances that impact the final selection. Thorough comprehension of the guidelines and structure behind the classification system is necessary to avoid common pitfalls and ensure accuracy in the final code assignment.
Practical Approaches to Selecting the Right Code
By working through real-life examples, one can develop the ability to make informed decisions in difficult situations. Using a systematic approach and understanding the key principles of code assignment makes it easier to navigate through the various options available for each condition. The process not only requires technical knowledge but also the ability to interpret medical documentation effectively.
Understanding ICD-10-CM Codes
Accurate classification of medical conditions is a critical aspect of the healthcare system. These classifications serve as the foundation for patient documentation, billing procedures, and statistical reporting. Understanding how to navigate the coding structure is essential for healthcare professionals who need to assign the right identifiers to diagnoses and treatments.
The system is designed to provide a universal way of representing diseases, injuries, and other health-related issues, ensuring consistency across the medical field. To facilitate this, each code corresponds to a specific condition or procedure, categorized into chapters and sections based on body systems or types of ailments.
| Category | Description | Example |
|---|---|---|
| Infectious Diseases | Conditions caused by pathogens like bacteria or viruses | Pneumonia, Tuberculosis |
| Neoplasms | Abnormal growths or tumors, benign or malignant | Lung cancer, Breast tumor |
| Endocrine Disorders | Conditions affecting the endocrine system | Diabetes, Hypothyroidism |
| Cardiovascular Diseases | Conditions related to the heart and blood vessels | Hypertension, Heart attack |
Each chapter within the classification system is subdivided into more specific categories, providing a detailed breakdown of related conditions. By understanding these classifications, medical professionals can ensure that their code assignments are precise, improving both the accuracy of patient records and the integrity of healthcare billing practices.
Common Coding Errors and Solutions
Inaccurate assignment of medical codes can lead to various problems, including incorrect billing, delayed reimbursements, and misinterpretation of patient records. These errors can stem from a lack of understanding, misreading of documentation, or confusion between similar conditions. Identifying common mistakes and understanding how to avoid them is key to improving accuracy in the classification process.
Frequent Mistakes in Code Selection
One of the most common errors is selecting the wrong code due to overlapping symptoms or diagnoses. For instance, confusion between conditions that share similar characteristics or using outdated codes can result in incorrect classifications. Careful review of the clinical documentation and staying updated with the latest guidelines is essential to avoid this issue.
Solutions for Ensuring Accuracy
To minimize mistakes, professionals should cross-reference codes with the detailed descriptions provided in the official coding manual. Utilizing code lookup tools and double-checking the provided information before finalizing the assignment can also help prevent errors. Thorough training and practice can further reduce the likelihood of selecting incorrect codes, ensuring better outcomes for both healthcare providers and patients.
How to Interpret ICD-10-CM Guidelines
Understanding and applying the official guidelines for medical classification can be challenging, as they provide a comprehensive framework for assigning the correct identifiers to various conditions. These rules are essential for ensuring accurate documentation, billing, and statistical reporting. Proper interpretation of the guidelines allows healthcare professionals to navigate through the complexities of diagnosis classification.
Key Principles of Guideline Interpretation
The guidelines are structured to offer clarity on how to approach the coding process for a wide range of medical conditions. They emphasize the importance of understanding the clinical context, including symptoms, diagnoses, and the patient’s medical history. By focusing on key elements such as the primary condition and its associated manifestations, professionals can make more informed decisions when selecting the appropriate codes.
Practical Tips for Applying Guidelines
One effective way to interpret these rules is to break them down into smaller sections, ensuring that each component is understood before moving on to the next. Cross-referencing guidelines with detailed case documentation can also help ensure that all conditions are accounted for and classified correctly. Consistent practice and familiarity with the guidelines lead to improved accuracy and confidence in making code assignments.
Real-World Examples of Coding Scenarios
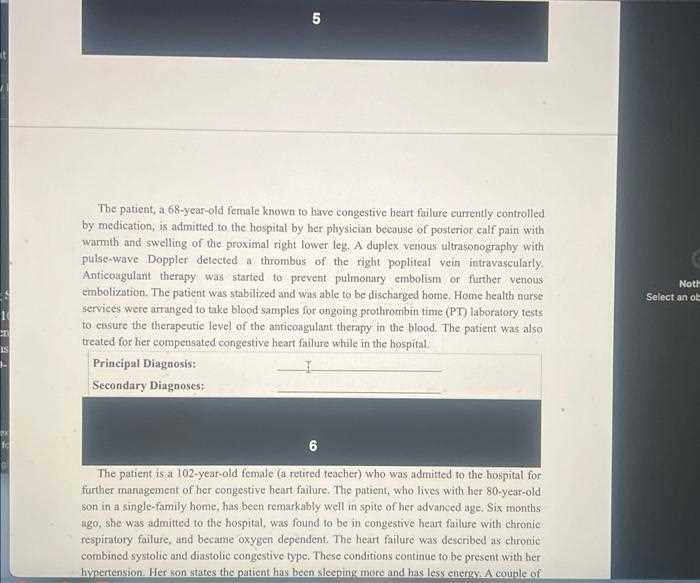
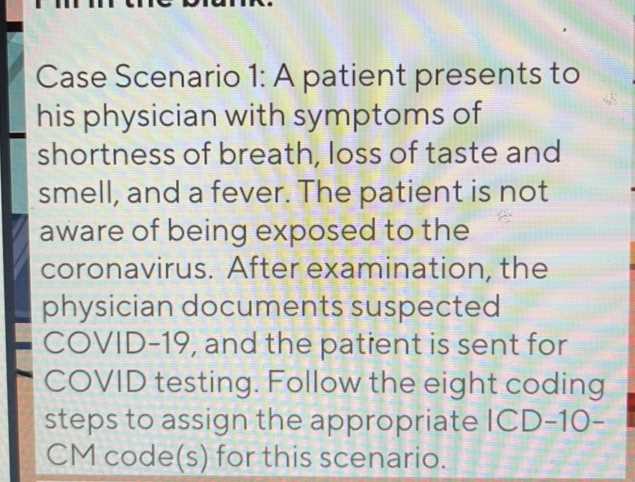
In the medical field, assigning the correct classification for a condition or procedure is not always straightforward. Real-life cases often involve complexities that require careful consideration of the patient’s medical history and symptoms. By studying practical examples, one can gain a deeper understanding of how to approach various clinical situations and make accurate code selections.
Below are a few common examples that demonstrate the process of selecting appropriate classifications based on detailed patient information. These cases highlight the importance of analyzing the clinical context and understanding the nuances of each condition.
| Condition | Description | Correct Code |
|---|---|---|
| Chronic Obstructive Pulmonary Disease (COPD) | A progressive lung disease that causes breathing difficulties | J44.9 – Chronic obstructive pulmonary disease, unspecified |
| Type 2 Diabetes | A metabolic disorder characterized by high blood sugar levels | E11.9 – Type 2 diabetes mellitus without complications |
| Acute Myocardial Infarction | A heart attack caused by a blockage of blood flow to the heart | I21.9 – Acute myocardial infarction, unspecified |
| Fractured Femur | A break in the thigh bone often resulting from trauma | S72.90XA – Unspecified fracture of femur, initial encounter |
Each example highlights the importance of considering all available information before selecting a code. The use of these classifications helps maintain consistency in patient records and supports accurate billing and statistical tracking within healthcare systems.
Step-by-Step Process for Accurate Coding
Assigning the correct medical classifications requires a systematic approach to ensure that all aspects of a patient’s condition are properly documented. This step-by-step process is designed to help healthcare professionals navigate the complexities of diagnosis and procedure classification, minimizing errors and improving accuracy in healthcare records.
Understanding the Documentation
The first step in the process is thoroughly reviewing the patient’s medical records. This includes examining the physician’s notes, lab results, and any other relevant clinical data. Understanding the full context of the condition and its associated symptoms is critical before proceeding to classification. Accurate documentation is the foundation for precise code assignment.
Choosing the Right Classification
After reviewing the documentation, the next step is selecting the most appropriate code based on the condition or procedure described. This requires familiarity with the classification system and a careful examination of each code’s specific criteria. By using the official manuals or online tools, coders can ensure they are selecting the most accurate code available.
| Step | Action | Key Considerations |
|---|---|---|
| Step 1 | Review medical documentation | Ensure all symptoms, diagnoses, and treatments are clearly recorded |
| Step 2 | Identify primary condition | Determine the most significant diagnosis or procedure for classification |
| Step 3 | Select appropriate code | Cross-reference documentation with code descriptions |
| Step 4 | Double-check for accuracy | Ensure the chosen code matches the clinical context |
Following these steps ensures that the final medical classification is as accurate as possible. Regular practice and ongoing education about the coding system help improve efficiency and reduce the chances of errors in patient records.
Key Differences Between ICD-9 and ICD-10
The transition from the previous classification system to the more advanced version brought significant changes to how medical conditions and procedures are recorded. Understanding these differences is crucial for healthcare professionals, as the new system offers enhanced specificity, a greater number of codes, and improved accuracy in categorizing diseases and treatments. Below are some of the key distinctions between the two systems.
Code Structure and Length
One of the most notable differences is the structure and length of the codes. In the older system, codes were primarily three to five characters long, while the newer system expands this to seven characters. This increase in characters allows for greater detail and precision in identifying diagnoses. The added characters provide specific information about the condition, its severity, and other relevant factors.
Number of Codes and Specificity
The newer classification system includes a significantly higher number of codes, offering greater granularity in terms of disease classification. While the previous version covered around 14,000 conditions, the updated system includes over 70,000 codes. This expansion allows for more precise tracking of conditions, helping improve patient care and support better decision-making in clinical practice.
| Feature | ICD-9 | ICD-10 |
|---|---|---|
| Code Length | 3-5 characters | 3-7 characters |
| Number of Codes | 14,000 codes | 70,000+ codes |
| Level of Specificity | Limited specificity | High level of detail |
| Use of Placeholder Characters | Not used | Uses placeholder characters (e.g., “X”) |
The enhanced specificity and expanded coding structure in the newer system are designed to capture a wider range of conditions and improve the overall efficiency of healthcare documentation and billing processes. These changes ultimately lead to more accurate reporting and better tracking of public health data.
Challenges in ICD-10-CM Code Selection
Selecting the appropriate medical codes for diagnoses and procedures can be a complex task. The expanded classification systems and the variety of medical conditions require healthcare professionals to have a deep understanding of both the guidelines and the specific details of each case. The challenges arise not only from the volume of codes but also from the need for precision and the ability to accurately interpret clinical documentation.
Complexity of Code Categories
One of the primary difficulties is the sheer complexity of the coding categories. Modern classification systems feature thousands of codes that can be grouped into broad categories, each containing numerous subcategories. Healthcare professionals must carefully differentiate between similar conditions to ensure the correct code is chosen. The overlapping nature of some codes can lead to confusion and potential errors in classification.
Incomplete or Inaccurate Documentation
Another challenge is dealing with incomplete or inaccurate patient documentation. Without detailed and precise information from physicians and healthcare providers, it becomes more difficult to select the correct code. If critical details such as the severity, stage, or complications of a condition are missing, coders may have to make assumptions, which can result in misclassification.
To overcome these challenges, coders often rely on tools like coding software, reference materials, and consultation with healthcare providers to ensure they make the most accurate selections possible. Regular training and updates are also essential in keeping up with new codes and changes in classification guidelines.
Tips for Avoiding Coding Mistakes
Accurate selection of medical classification codes is crucial for proper billing, patient care, and health data management. Mistakes in this process can lead to claims rejections, incorrect billing, and potential legal issues. To minimize errors, it’s essential to adopt a careful, methodical approach and follow best practices that promote accuracy and consistency.
Thorough Review of Documentation
One of the most important steps in avoiding mistakes is ensuring that all medical documentation is complete and accurate. Coders should always double-check the physician’s notes, test results, and other relevant information before making a selection. Any missing or ambiguous details can lead to misclassification.
- Ensure all symptoms, diagnoses, and treatments are clearly noted.
- Clarify any unclear terms or abbreviations with the healthcare provider.
- Look for additional reports or diagnostic tests that may provide more context.
Use of Code Lookup Tools
Utilizing online code lookup tools and official manuals can significantly reduce the risk of errors. These resources help coders locate the most accurate and up-to-date codes based on the information in the patient’s medical records.
- Regularly refer to official coding guidelines to ensure compliance.
- Take advantage of software that helps validate code selections.
- Cross-check similar codes to verify the correct choice.
Continuous Training and Education
Keeping up with changes in medical classification systems is essential to prevent mistakes. Regular training helps coders stay informed about new codes, revisions to existing codes, and best practices in code selection.
- Attend workshops and webinars on updated guidelines.
- Participate in coding certification programs to enhance knowledge and skills.
- Follow updates from authoritative healthcare organizations regarding changes in classification systems.
By maintaining a meticulous approach, using available tools, and investing in ongoing education, healthcare professionals can avoid common mistakes and ensure the highest level of accuracy in classification processes.
Impact of ICD-10-CM on Healthcare Billing
The shift to a more detailed and expansive classification system has had a significant impact on healthcare billing practices. With more specific codes available, billing processes have become more precise, yet they also demand greater attention to detail. Healthcare providers, insurers, and coders must ensure accuracy in the documentation and classification of medical services to facilitate proper reimbursement and avoid claim denials.
Improved Accuracy and Reimbursement
One of the primary advantages of the updated system is the ability to capture a higher level of detail in diagnoses and procedures. This allows for better representation of the patient’s condition and the treatment provided, leading to more accurate billing. Insurers can process claims more efficiently and reimburse healthcare providers based on the precise nature of the services rendered.
- Greater specificity helps eliminate ambiguities in claims.
- Proper documentation supports appropriate reimbursement levels.
- Accurate codes reduce the likelihood of underpayment or overpayment.
Challenges in Transition and Compliance
However, transitioning to the updated system has introduced certain challenges. The increased complexity of the classification means that medical professionals must be more diligent in their coding practices. Errors can result in claim rejections or delays in reimbursement, leading to financial strain for healthcare providers. Additionally, compliance with regulations and guidelines is crucial to avoid audits and penalties.
- Training and adaptation are essential for coding staff to maintain compliance.
- Frequent audits may be necessary to ensure correct code usage.
- Complex codes require additional time and resources to ensure accuracy.
Overall, while the transition has brought about improvements in the accuracy of healthcare billing, it has also highlighted the need for ongoing education, training, and technological support to minimize errors and ensure smooth reimbursement processes.
Advanced Coding Techniques for Professionals
For seasoned professionals, mastering advanced techniques in classification is crucial for maintaining accuracy and efficiency in complex cases. These methods go beyond basic code selection and require a deep understanding of medical terminology, guidelines, and nuances within the healthcare system. By honing these skills, professionals can ensure that they provide the most precise and comprehensive codes, reducing errors and improving overall workflow.
Utilizing Combination Codes
One of the key strategies in advanced classification is the use of combination codes. These are codes that represent multiple conditions or factors in a single entry. Professionals need to understand when and how to apply these codes to avoid unnecessary fragmentation of diagnoses. Proper use of combination codes can significantly streamline the process and ensure that all relevant aspects of a patient’s condition are captured.
- Review medical records for coexisting conditions that can be captured in a single code.
- Apply the most specific code to avoid unnecessary combinations.
- Ensure that all components of a condition are included in the selected code.
Advanced Review of Medical Documentation
In-depth analysis of medical documentation is essential for identifying the most appropriate classifications. This involves scrutinizing physician notes, test results, and patient history to identify subtle details that may influence code selection. Professionals must look beyond surface-level symptoms and consider the patient’s full clinical picture.
- Cross-reference medical records to ensure all relevant diagnoses and treatments are documented.
- Interpret lab results, radiology reports, and physician comments accurately.
- Look for secondary conditions or complications that might affect treatment codes.
Staying Updated with Regulatory Changes
Healthcare coding standards and guidelines are regularly updated. Professionals must stay informed of any regulatory changes that could affect code selection or billing practices. This requires ongoing education and awareness of the latest trends, including the introduction of new codes or the retirement of outdated ones.
- Subscribe to updates from regulatory bodies to stay informed.
- Participate in webinars, workshops, and coding conferences.
- Leverage professional resources such as coding manuals and online databases for real-time guidance.
By applying these advanced techniques, professionals can navigate complex coding challenges with greater accuracy and efficiency, ensuring proper reimbursement and reducing the likelihood of errors in their classification processes.
Using ICD-10-CM for Specific Diagnoses
Accurate classification of medical conditions is essential for effective treatment, proper billing, and insurance reimbursement. The process involves selecting the most appropriate codes to represent specific diagnoses, ensuring that all relevant details are captured. Understanding how to apply the correct codes for various conditions can significantly improve the clarity and precision of healthcare documentation.
Identifying Common Conditions
For common illnesses and conditions, it’s crucial to select the right code that reflects the severity, type, and cause of the condition. Professionals should review patient records carefully to distinguish between different variations of the same disease, as some conditions may have multiple codes based on factors such as chronicity or underlying causes.
- Consider the presence of co-existing conditions, such as diabetes or hypertension, which may affect the primary diagnosis.
- Pay close attention to modifiers that specify the stage, type, or location of the condition.
- Utilize combination codes to capture more than one related condition in a single entry.
Complex or Rare Diagnoses
In the case of complex or less common diseases, careful interpretation of medical records is essential. These conditions may require the use of detailed codes that account for unusual factors, such as rare symptoms or genetic variations. Properly classifying these diagnoses ensures that healthcare providers receive appropriate compensation and that patients’ medical histories are accurately reflected.
- Ensure that rare conditions are properly identified and classified by cross-referencing with specialized coding resources.
- Look for notes from specialists that may provide additional details for accurate code selection.
- Consult up-to-date coding manuals to ensure that all relevant aspects of complex diagnoses are represented.
By following these steps, healthcare professionals can ensure that diagnoses are categorized correctly, facilitating accurate treatment and reimbursement processes while reducing errors in patient care documentation.
Code Validation and Verification Methods
Ensuring the accuracy of medical codes is a critical aspect of healthcare administration. Proper validation and verification methods are necessary to confirm that the selected codes reflect the correct diagnoses and treatments. These procedures help minimize errors, ensuring compliance and maximizing reimbursement while maintaining the integrity of patient records.
Validation Steps
Validation involves reviewing the selected codes to ensure they are correctly aligned with the patient’s condition and the provided medical documentation. This process helps confirm that the codes are both comprehensive and specific enough to represent the condition or procedure accurately.
- Cross-reference codes with patient medical records to verify that all relevant information is included.
- Ensure that the codes match the most current guidelines and coding standards.
- Check for consistency between the diagnosis and the treatment provided to avoid mismatches.
Verification Techniques
Verification goes a step further by actively confirming that the selected codes comply with the rules set forth by insurers and regulatory bodies. It often involves utilizing specialized software tools or coding assistants to cross-check the codes against established criteria.
- Use coding software or automated tools to run validation checks and suggest potential errors.
- Verify that modifiers are properly applied to capture nuances in the diagnosis or treatment.
- Consult clinical coders or coding specialists for complex cases that require deeper review.
By utilizing these validation and verification methods, healthcare providers can ensure accurate, efficient, and compliant coding practices, which ultimately improve the overall quality of patient care and streamline administrative processes.
Understanding Medical Terminology for Coders
For healthcare professionals involved in the process of assigning diagnostic and procedural codes, a strong understanding of medical terminology is essential. The language of medicine is rich and specific, and it serves as the foundation for accurately translating clinical information into standardized codes. Without a clear grasp of medical terminology, errors can occur, potentially leading to incorrect coding, improper billing, and even compromised patient care.
Medical terminology encompasses a wide range of terms related to human anatomy, diseases, treatments, and procedures. Coders must be familiar with these terms to interpret clinical documentation effectively and select the appropriate codes. The following are key areas to focus on:
Key Areas of Medical Terminology for Coders
- Anatomical Terms: Understanding body parts and systems, such as the cardiovascular, respiratory, or musculoskeletal systems, is essential for accurate code assignment.
- Disease Terminology: Coders should be well-versed in the names of conditions, disorders, and diseases, from common illnesses like diabetes to rare genetic disorders.
- Procedure and Treatment Terms: It is vital to recognize the various medical procedures and treatments, such as surgeries, diagnostic tests, and therapies, to assign the correct procedural codes.
Common Medical Prefixes, Suffixes, and Root Words
- Prefixes: These are added to the beginning of words to modify their meaning. For example, “hypo-” means low or under, as in “hypotension” (low blood pressure).
- Suffixes: These are added to the end of words and often indicate the type of condition. For instance, “-itis” refers to inflammation, as seen in “arthritis” (inflammation of the joints).
- Root Words: The core part of a medical term, such as “cardi-” (heart) or “neuro-” (nerve), which forms the foundation of many related terms.
By mastering medical terminology, coders can confidently navigate clinical documentation, identify the correct diagnoses and procedures, and ensure that coding is precise, compliant, and consistent. This knowledge is fundamental to the overall efficiency and accuracy of the healthcare coding process.
Resources for Improving Coding Accuracy
Accurate medical record classification is a crucial part of healthcare administration. To achieve precision and consistency, professionals must continually refine their skills and stay updated with the latest standards. Numerous tools and resources are available to assist in enhancing coding accuracy, from educational materials to technological advancements.
By leveraging the right resources, coders can improve their proficiency, reduce errors, and ensure compliance with regulations. Below are some of the most effective tools and practices that can help professionals improve their coding accuracy:
Educational and Training Resources
- Workshops and Webinars: Regular participation in live or recorded sessions focused on best practices and updates in medical classification systems.
- Certification Programs: Enrolling in specialized courses, such as those offered by professional organizations, to achieve certification and gain deeper expertise.
- Online Courses: Numerous platforms provide structured learning paths that cover the nuances of medical terminology, documentation, and classification systems.
Tools for Coding Support
- Code Lookup Software: Advanced search tools and databases that allow professionals to quickly find the correct classification based on clinical notes.
- Code Books and Manuals: Official guides and reference books offer a thorough understanding of classification structures and code assignment rules.
- Audit Software: Tools designed to review and verify codes, ensuring that they are accurate and compliant with current guidelines.
Incorporating these resources into everyday practice can significantly improve the precision and reliability of the classification process, leading to better outcomes in both billing and patient care. Ongoing education and utilization of advanced tools ensure that coding professionals are equipped to handle the complexities of modern healthcare systems.
Frequently Asked Questions About ICD-10-CM
As healthcare systems continue to evolve, so too does the process of classifying medical conditions and procedures. Understanding the intricacies of classification systems can be challenging for many professionals, especially those new to the field. This section addresses some of the most common questions regarding the structure, usage, and impact of medical classification systems, aiming to clarify common misconceptions and provide helpful insights.
What is the Purpose of Medical Classification Systems?
Medical classification systems serve to organize and standardize the documentation of patient diagnoses and treatment procedures. These systems ensure that healthcare providers, insurance companies, and researchers have a common framework for interpreting medical information, which enhances communication and facilitates billing, reporting, and analysis.
How Do Classification Systems Impact Billing and Reimbursement?
Accurate and consistent coding is essential for proper billing and reimbursement. Incorrectly assigned codes can result in claim denials, delayed payments, or financial penalties. Therefore, understanding the structure of classification systems and applying them correctly ensures that healthcare providers are reimbursed promptly and fairly for their services. Effective coding also reduces the risk of audits and compliance issues.
By understanding the rules and structure of medical classification systems, healthcare professionals can better navigate the complex environment of medical documentation and billing. Continual education and practical experience are key to mastering this essential aspect of healthcare administration.