
Successfully navigating the pediatric life support certification process requires a deep understanding of key principles and practices. This section will provide you with essential information to enhance your preparation, focusing on critical concepts and practical scenarios you’ll encounter. By reviewing common themes and protocols, you can approach your assessment with confidence and a well-rounded knowledge base.
Effective preparation involves not only memorizing guidelines but also applying them to real-life situations. This guide will help you identify the most important topics and areas to focus on, ensuring that you are equipped with the knowledge needed for successful certification.
Understanding core concepts and being familiar with the structure of the assessment is key. By exploring various study strategies and sample questions, you’ll be able to assess your readiness and identify areas that need further attention. Prepare thoroughly to ensure a smooth and successful certification journey.
Pediatric Life Support Assessment Guide
Preparing for the pediatric life support certification requires careful study of essential procedures and protocols. This section outlines a comprehensive guide to help you tackle the key topics and provide clear strategies for succeeding in the assessment. Whether you are a beginner or have previous experience, understanding these areas is vital for achieving the best results.
Key Focus Areas
To ensure that you are well-prepared, focus on the following areas, which are commonly tested:
- Assessment and recognition of pediatric emergencies
- Effective resuscitation techniques for children
- Proper medication dosages and delivery methods
- Understanding of advanced life-saving algorithms
- Clear communication in high-pressure scenarios
Test Preparation Strategies
Utilize these strategies to maximize your study efforts and enhance your chances of success:
- Review key protocols and their application in real-life situations
- Practice with sample questions and case studies to familiarize yourself with question formats
- Prioritize high-yield topics, such as airway management and CPR techniques
- Take time to understand the reasoning behind each treatment approach
- Ensure you are familiar with both basic and advanced life support guidelines
By focusing on these key areas and adopting effective study habits, you will feel confident and prepared for the certification process.
Overview of Pediatric Life Support Assessment
The pediatric life support certification process is designed to assess your understanding and ability to apply life-saving techniques in emergency situations involving children. This section provides an overview of what to expect, highlighting the most critical aspects of the assessment that will test your knowledge and readiness for real-life scenarios.
What the Certification Covers
During the assessment, you will be tested on your ability to manage various pediatric emergencies and provide appropriate interventions. Some of the areas you will need to focus on include:
- Initial patient assessment and recognition of distress signs
- Airway management and resuscitation techniques
- Appropriate use of medications in emergencies
- Advanced techniques for life support in pediatric patients
- Understanding of critical protocols and guidelines
Structure and Format
The test is structured to evaluate both theoretical knowledge and practical application. You can expect a combination of multiple-choice questions, scenario-based questions, and possibly a hands-on component that simulates real-world situations. Preparation is key to navigating these diverse question types and demonstrating your proficiency in pediatric care.
Being familiar with the structure of the certification process will help you manage your time effectively and approach each section with confidence.
How to Prepare for Pediatric Advanced Life Support Certification
To successfully prepare for pediatric advanced life support certification, it is crucial to combine knowledge with practical experience. Understanding medical protocols, recognizing signs of distress in children, and knowing the appropriate steps to take in urgent situations are essential. A focused approach to both theory and hands-on practice will ensure you are well-equipped to handle critical pediatric emergencies with confidence and competence.
Effective Study Techniques
Preparation for certification requires consistent and efficient study methods. Consider these effective techniques to guide your learning:
- Review and memorize key treatment protocols for pediatric emergencies.
- Practice skills regularly through simulation scenarios to build muscle memory and improve decision-making under pressure.
- Set a study schedule that includes daily learning goals, with breaks for practical practice.
- Engage in group study sessions to discuss and clarify complex topics.
- Use study guides, flashcards, or digital tools for quick reviews and reinforcing important concepts.
Focus Areas for Mastery
There are several critical areas to prioritize when preparing for this certification. These areas are commonly tested and require in-depth understanding:
| Key Topic | Level of Importance |
|---|---|
| Cardiac Arrest Management | High |
| Airway and Breathing Support | High |
| Shock and Fluid Management | Medium |
| Medications and Dosage Calculation | Medium |
| Team Roles and Communication | Low |
By mastering these core areas and committing to consistent practice, you will be well-prepared for the challenges presented during the certification process. Prioritize hands-on skills and understanding theoretical concepts to ensure a balanced and comprehensive preparation.
Understanding Key Pediatric Concepts
When preparing for any advanced life support certification, it is essential to have a deep understanding of pediatric care fundamentals. Key concepts in pediatric medicine include recognizing physiological differences in children compared to adults, mastering the identification of common emergency scenarios, and knowing the appropriate responses to those situations. A solid grasp of these concepts ensures that healthcare providers can manage urgent care situations effectively, with the child’s best interests at the forefront.
Key Differences in Pediatric Physiology
Children are not just small adults; their bodies function differently, and recognizing these differences is crucial for proper care. Some of the important physiological factors to keep in mind include:
- Heart Rate Variations: Children typically have higher heart rates than adults. Understanding these variations can help in accurate assessment.
- Respiratory Patterns: Pediatric respiratory systems are more prone to obstruction and collapse. Early intervention is vital.
- Fluid Balance: Children are more susceptible to dehydration and fluid imbalances due to their higher metabolic rate and greater body surface area.
- Temperature Regulation: Pediatric patients may have a harder time regulating body temperature, which can complicate critical care situations.
Emergency Protocols for Children
Effective pediatric emergency care requires a different approach than adult care. A few common protocols and approaches to focus on include:
- Assessment of Airway and Breathing: Quick identification of respiratory distress and securing an airway is essential for survival.
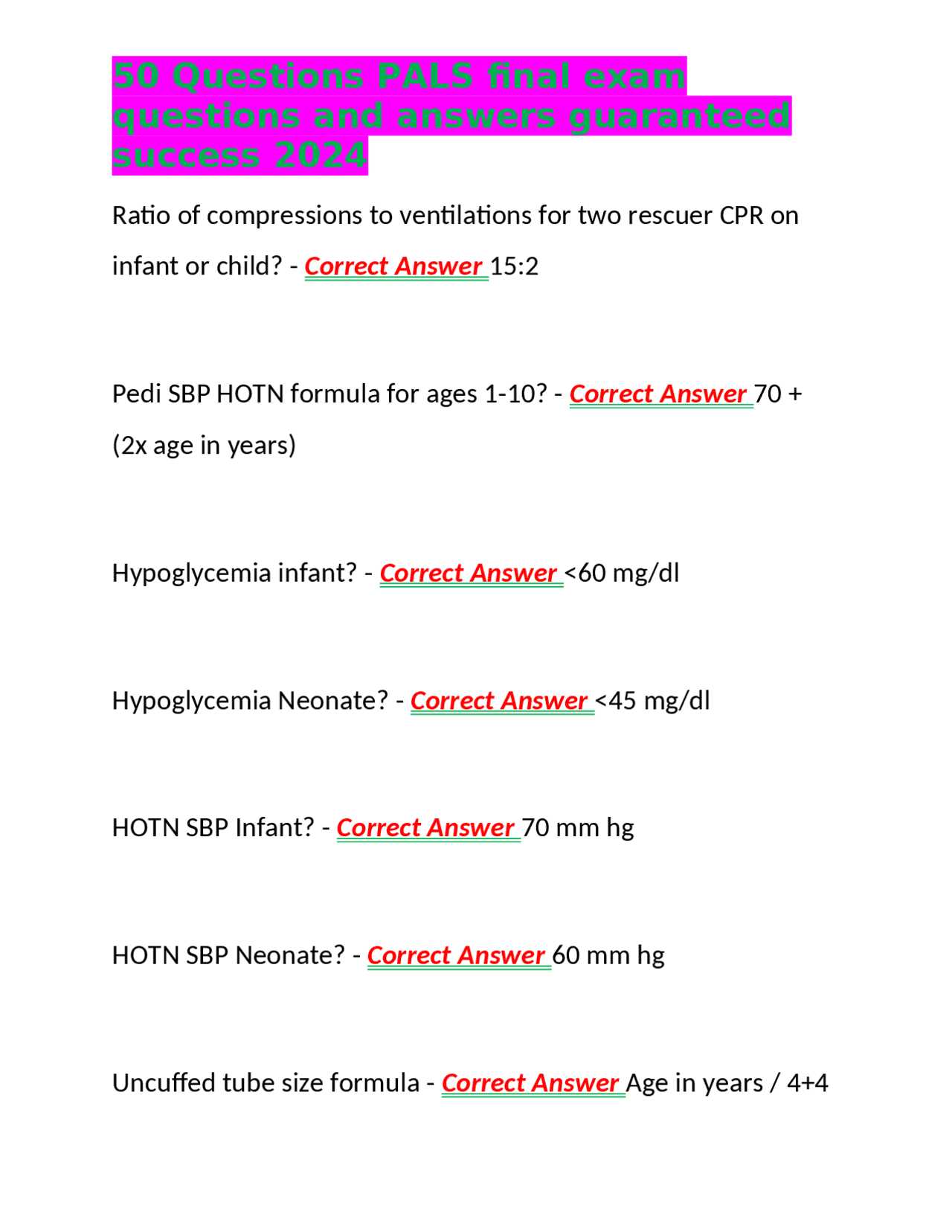
- Cardiac Arrest Management: The protocols for pediatric cardiac arrest differ significantly from those for adults, with variations in CPR techniques and medication dosages.
- Shock Recognition: Children can compensate for shock for a time, so it’s crucial to identify early signs of shock, such as rapid heart rate and poor capillary refill.
- Medication Dosage: Pediatric patients require specific dosing based on their weight, age, and size. Understanding how to calculate doses properly is essential.
By mastering these concepts, healthcare providers will be better equipped to assess and manage pediatric patients in emergency situations, ensuring the best possible outcomes for the child.
Common Topics Covered in Pediatric Life Support Training
In pediatric emergency care, several key topics are consistently emphasized to ensure healthcare professionals are well-prepared to handle critical situations. These topics encompass a range of life-saving techniques, clinical knowledge, and scenario-based protocols that are crucial for effective intervention in pediatric emergencies. By focusing on these areas, providers can ensure they are ready to deliver the best care possible under pressure.
Key Clinical Concepts and Procedures
The following clinical areas are essential in pediatric life support training:
- Cardiac Arrest Management: Knowing the differences in performing CPR and advanced life support techniques for children compared to adults is vital. This includes techniques for airway management, chest compressions, and defibrillation.
- Respiratory Distress and Failure: Identifying signs of respiratory distress, and being familiar with treatment protocols for pediatric patients facing respiratory emergencies, such as airway obstruction and asthma attacks.
- Shock Management: Recognizing the early signs of shock in children and understanding the appropriate steps to stabilize circulation, including fluid resuscitation and medication protocols.
- Trauma and Injury Management: Trauma is a leading cause of pediatric emergencies. Proper techniques for assessing injuries, managing bleeding, and stabilizing fractures are critical in saving lives.
Special Considerations for Pediatric Care
In addition to basic life support protocols, there are specific considerations unique to children’s physiology and care needs:
- Fluid and Electrolyte Imbalances: Pediatric patients are more susceptible to dehydration and imbalances, especially in critical care. Understanding how to manage fluids in young patients is crucial.
- Weight-Based Medication Dosing: Medication dosing for children is typically based on their weight, and accurately calculating these doses is essential to prevent over- or under-administration.
- Neonatal and Infant Care: Special procedures are required for newborns and infants due to their fragile physiology. This includes neonatal resuscitation, neonatal airway management, and monitoring for signs of sepsis.
These topics are essential components of any training aimed at preparing healthcare professionals to effectively respond to pediatric emergencies. Mastery of these concepts ensures that providers are equipped with the skills needed to make quick, accurate decisions in high-stress situations.
What to Expect in Pediatric Life Support Assessment
When preparing for a pediatric life support assessment, candidates should be ready to encounter a range of clinical scenarios that test their ability to respond effectively in emergency situations. The assessment is designed to evaluate the participant’s knowledge, skills, and decision-making abilities in various pediatric care emergencies. It will involve both theoretical questions and practical exercises, which simulate real-life situations that healthcare providers might face.
Types of Scenarios and Questions
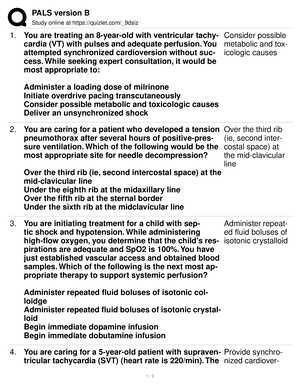
The assessment typically includes a mix of multiple-choice questions and scenario-based exercises, where candidates must demonstrate their competence in managing critical pediatric situations. Below are some areas that are commonly covered:
- Cardiopulmonary Resuscitation (CPR) Techniques: Candidates will be assessed on their ability to perform pediatric CPR correctly, including the appropriate technique for infants, children, and adolescents.
- Airway Management: Proper techniques for securing a pediatric airway, including the use of adjuncts such as suction devices, bag-valve masks, and endotracheal tubes, will be tested.
- Drug Dosing and Administration: Participants will be required to demonstrate accurate knowledge of pediatric medication dosages, particularly for critical care drugs.
- Trauma and Injury Response: Participants may be asked to make rapid decisions regarding the stabilization of a child following an injury, including fracture management and control of bleeding.
Key Skills Tested
In addition to knowledge of medical procedures, the assessment also evaluates several key practical skills:
- Effective Communication: Clear communication is crucial in emergency settings. Candidates will need to demonstrate how they interact with team members, deliver concise instructions, and ensure patient safety.
- Clinical Decision-Making: The assessment will test the participant’s ability to make critical decisions under pressure, prioritizing actions and interventions based on the severity of the situation.
- Teamwork: The ability to work as part of an emergency response team is crucial. Participants will be observed on their ability to coordinate and collaborate effectively with others.
Successfully completing this assessment ensures that healthcare professionals are ready to handle a wide variety of pediatric emergencies, using the most current and effective protocols for life-saving interventions.
Study Tips for Pediatric Life Support Assessment
Preparing for a pediatric life support assessment requires a focused approach to mastering both the theoretical knowledge and practical skills needed to handle critical pediatric emergencies. To succeed, it is essential to follow a structured study plan, integrate hands-on practice, and actively test your understanding through various methods.
Key Study Strategies
1. Review Guidelines and Protocols: Make sure you are familiar with the latest guidelines and protocols for pediatric emergencies. Understanding the recommended steps for resuscitation, airway management, and medication dosing is crucial for the assessment. Regularly review updated materials from reliable sources to ensure your knowledge is current.
2. Practice Hands-On Skills: Practical skills such as performing CPR, managing airways, and using emergency equipment should be practiced regularly. Find a training center or group where you can rehearse these skills in a controlled environment. Hands-on practice helps reinforce the procedures and ensures you’re comfortable performing them under pressure.
3. Utilize Scenario-Based Learning: Simulation exercises are key to preparing for real-life situations. By engaging in scenario-based learning, you can simulate high-pressure emergency scenarios and practice decision-making. This approach helps you improve your response time and effectiveness in critical moments.
Additional Tips
- Break Down Complex Topics: Divide complex topics into manageable sections. Focus on one area at a time, such as drug dosages, specific resuscitation techniques, or trauma management, to avoid feeling overwhelmed.
- Collaborate with Peers: Studying with a group can provide different perspectives and help reinforce learning. Discuss challenging scenarios with colleagues to improve your understanding and retention.
- Test Yourself: Regularly test your knowledge with quizzes and mock assessments. This will help you identify any areas where you may need further study and improve your confidence in answering questions quickly and accurately.
4. Stay Calm and Confident: Remember that remaining calm and composed is essential in emergency situations. Confidence in your skills and knowledge will improve your performance during both the practical and theoretical portions of the assessment.
By following these tips and staying dedicated to your preparation, you will be well-equipped to succeed in the pediatric life support assessment, ensuring you’re ready to provide effective care when it’s most needed.
Practice Questions for Pediatric Life Support Assessment
To effectively prepare for a pediatric life support evaluation, it’s crucial to practice with a variety of questions that test both your theoretical understanding and practical decision-making skills. By tackling practice questions, you can identify knowledge gaps, reinforce key concepts, and improve your response time under pressure. These questions typically cover emergency protocols, drug dosages, and resuscitation techniques, ensuring that you are well-prepared for any scenario.
Sample Practice Questions
- Question 1: A 4-year-old child is brought into the emergency room after a near-drowning incident. What is the first step in managing this case?
- Assess the child’s airway and breathing
- Administer oxygen
- Start intravenous access
- Perform chest compressions
- Question 2: You are managing a 6-year-old patient with suspected anaphylaxis. What is the recommended first-line treatment?
- Administer epinephrine intramuscularly
- Administer antihistamines
- Begin intravenous fluids
- Provide oxygen therapy
- Question 3: What is the appropriate dose of epinephrine for a child experiencing severe allergic reaction with respiratory distress?
- 0.01 mg/kg of body weight
- 0.1 mg/kg of body weight
- 1 mg/kg of body weight
- 0.5 mg/kg of body weight
- Question 4: In a scenario where a child presents with bradycardia, what is the first intervention that should be performed?
- Assess the heart rate and reassess after 5 minutes
- Administer atropine
- Start chest compressions immediately
- Provide bag-mask ventilation
How to Use Practice Questions Effectively
- Review the Answer Key: After attempting each question, review the correct answers and understand why they are the best choices. This helps reinforce the correct decision-making process.
- Time Yourself: Practice under timed conditions to simulate the pressure of real-life scenarios. This will help you become more efficient and calm during critical situations.
- Focus on Weak Areas: If you consistently struggle with certain topics, dedicate more study time to those areas. Repetition will improve your understanding and retention.
- Discuss with Peers: Collaborate with colleagues to go over difficult questions and scenarios. Group discussions can provide different perspectives and deepen your understanding of complex topics.
Using practice questions regularly will improve your confidence and competence, ensuring you are ready for any pediatric emergency that may arise.
Time Management During the Assessment
Effective time management during an assessment is crucial to ensure that all tasks are completed accurately within the allotted time frame. By organizing your approach, prioritizing questions, and managing your pace, you can reduce stress and maximize performance. The goal is to balance thoroughness with efficiency, allowing enough time to review your responses before submission.
Strategies for Efficient Time Use
- Prioritize Easy Questions: Begin with questions you are confident about. This will help build momentum and secure quick points. Avoid spending too much time on difficult questions at the start.
- Allocate Time Per Section: Divide your total time based on the number of sections or questions. Stick to the designated time for each part to ensure you can address everything.
- Watch the Clock: Regularly check the time to avoid rushing towards the end. Set a reminder halfway through the assessment to assess your progress and adjust if needed.
- Skip and Return: If a question is taking too long, move on and come back to it later. It’s better to answer all the easier questions first than to get stuck on a single problem.
- Review Your Responses: If time permits, leave the last 5-10 minutes for a final review of your answers. Look for any obvious mistakes or questions that may require adjustments.
How to Deal with Time Pressure
- Stay Calm: Anxiety can hinder your ability to think clearly. Take deep breaths if you feel overwhelmed and focus on one question at a time.
- Don’t Overthink: Trust your initial instincts for most questions. Spending too much time reconsidering your answers can lead to unnecessary stress.
- Break Down Complex Questions: For questions that seem complicated, break them down into manageable parts. Identify key concepts and tackle them step by step.
By applying these time management strategies, you can optimize your performance and complete the assessment with confidence and clarity.
Reviewing Critical Pediatric Emergencies
Understanding how to recognize and respond to life-threatening conditions in children is a vital aspect of healthcare training. Pediatric emergencies require swift, accurate assessments and interventions, as children often exhibit different signs and symptoms compared to adults. Familiarity with the most common critical situations ensures that healthcare providers can act decisively under pressure, improving the chances of positive outcomes.
Common Pediatric Emergencies
- Respiratory Distress: Conditions like asthma, pneumonia, or foreign body obstruction can quickly escalate to respiratory failure. Recognizing early signs, such as wheezing or difficulty breathing, is essential for prompt treatment.
- Cardiac Arrest: Although rare in children, cardiac arrest can result from severe trauma, congenital heart defects, or electrical disturbances. Immediate resuscitation and defibrillation are key in improving survival chances.
- Sepsis: A systemic infection can lead to shock and organ failure if not rapidly addressed. Identifying signs such as fever, rapid heart rate, and altered mental state can help in early intervention.
- Trauma and Head Injuries: Trauma, including head injuries and fractures, is common in pediatric emergencies. It is critical to assess the severity of the injury and prevent further damage.
- Anaphylaxis: Severe allergic reactions can cause rapid airway constriction and shock. Early recognition and administration of epinephrine can save lives.
Approach to Pediatric Emergencies
- Initial Assessment: The ABCDE approach (Airway, Breathing, Circulation, Disability, Exposure) is used to quickly evaluate and stabilize the child. Prioritizing life-threatening issues ensures that the child receives the most urgent care first.
- Clear Communication: In critical situations, clear communication with the child’s family and medical team is crucial. Accurate information helps guide treatment decisions.
- Pre-hospital Care: Timely intervention, whether by paramedics or first responders, can stabilize a child until they reach the hospital. Initial management, such as airway control and fluid resuscitation, is often life-saving.
- Teamwork: Pediatric emergencies require coordination among healthcare professionals, including doctors, nurses, and specialists. Collaborative decision-making is essential for effective management.
By staying well-versed in common pediatric emergencies and maintaining a structured approach, healthcare providers can significantly improve the prognosis for children in critical conditions.
Important Protocols and Guidelines
In pediatric care, following established protocols and guidelines is crucial for providing timely and effective treatment. These protocols ensure that healthcare professionals are prepared to respond to emergencies, manage critical situations, and improve patient outcomes. They serve as evidence-based frameworks, allowing for consistent care across various healthcare settings.
Key Protocols to Follow
- Airway Management: Ensuring that the child’s airway is open and secure is the first priority in any emergency. Guidelines include assessing airway patency, using appropriate airway devices, and providing respiratory support when necessary.
- Cardiopulmonary Resuscitation (CPR): CPR protocols are essential for cases of cardiac arrest. Providers should follow the correct compression-to-ventilation ratios, and adjust the techniques based on the child’s age and size.
- Fluid Resuscitation: When managing shock or dehydration, timely fluid administration is vital. Protocols outline the use of intravenous fluids, including saline or lactated Ringer’s, and help guide the rate and volume of fluid replacement.
- Defibrillation and Medication: Guidelines for defibrillation emphasize the use of the correct energy levels for pediatric patients. Medications such as epinephrine or atropine should be administered as per age-specific dosages and clinical indications.
Clinical Guidelines for Specific Conditions
- Sepsis Management: Early recognition and treatment of sepsis are essential. Protocols for sepsis include early antibiotic administration, fluid resuscitation, and monitoring for organ failure.
- Respiratory Emergencies: Treatment guidelines for respiratory distress focus on non-invasive techniques such as oxygen therapy and nebulized medications. In cases of severe obstruction or respiratory failure, intubation may be necessary.
- Anaphylaxis Protocol: In cases of severe allergic reactions, administering epinephrine immediately is the key step. Guidelines recommend assessing airway and circulatory stability, and providing antihistamines and corticosteroids as needed.
- Trauma Management: Protocols for managing trauma emphasize stabilizing the patient’s spine, controlling bleeding, and addressing fractures. Special care is taken when dealing with head injuries, ensuring that neuroprotective measures are in place.
Key Considerations for Effective Care
- Early Recognition: One of the most critical components of pediatric emergency care is the early identification of life-threatening conditions. Guidelines emphasize recognizing warning signs such as abnormal vital signs, changes in consciousness, or difficulty breathing.
- Team Collaboration: Effective communication and teamwork are integral in managing critical situations. Clear roles should be established among healthcare providers to ensure efficient care and minimize errors.
- Patient Monitoring: Continuous monitoring of vital signs, including heart rate, respiratory rate, blood pressure, and oxygen saturation, is crucial during emergency interventions. Guidelines stress the importance of reassessing the patient regularly and adjusting treatment as needed.
By adhering to these protocols and guidelines, healthcare providers can ensure that children receive the most effective and evidence-based care during critical situations, ultimately improving their chances of recovery.
Test-Taking Strategies for PALS Exam
Effective preparation is key to performing well in any assessment, especially in critical care settings. Developing strong test-taking strategies can help you approach each question with confidence, manage your time effectively, and reduce anxiety. By applying a structured approach, you can maximize your chances of success and improve your overall performance on the test.
Time Management Tips
One of the most important aspects of any test is managing your time effectively. Below are some strategies to ensure you make the most of the time allotted:
- Read the Instructions Carefully: Start by thoroughly reading the directions to ensure you understand what is being asked. Skipping this step can lead to misunderstandings and mistakes.
- Don’t Spend Too Much Time on One Question: If a question seems too difficult, move on and come back to it later if time permits. This ensures that you complete all the questions within the time limit.
- Set Time Limits for Each Section: Break down the total time available and assign a specific amount of time for each section of the test. This helps you pace yourself and ensures you don’t rush through easier questions.
How to Approach Multiple-Choice Questions
Multiple-choice questions can sometimes feel overwhelming, but there are strategies to improve your chances of choosing the right answer:
- Eliminate Incorrect Answers: Begin by eliminating answers that you know are clearly wrong. This improves your odds if you need to make an educated guess.
- Look for Keywords: Focus on keywords in both the question and the answer options. Pay attention to qualifiers like “always,” “never,” and “most likely,” which can help you identify the best choice.
- Choose the Best Option: When uncertain, choose the answer that is most consistent with your clinical knowledge. Avoid second-guessing yourself too much.
Staying Calm and Focused
Maintaining composure during the test is crucial. Below are some techniques to help you stay calm and focused:
- Practice Relaxation Techniques: Before the test, practice deep breathing or other relaxation exercises to reduce stress. This can help calm your nerves during the test.
- Stay Positive: Keep a positive mindset throughout the test. Confidence in your preparation can reduce anxiety and help you perform better.
- Don’t Rush: Take your time and avoid rushing through questions. Focus on understanding the question and the available choices before making a decision.
Reviewing Your Answers
If time permits, always review your answers before submitting the test. Check for simple mistakes such as misread questions or overlooked details. Reviewing allows you to catch errors that might have been missed in your initial attempt.
| Strategy | Action |
|---|---|
| Time Management | Allocate time per section and avoid dwelling on difficult questions. |
| Multiple-Choice Questions | Eliminate clearly wrong answers and focus on the most relevant keywords. |
| Staying Calm | Practice relaxation and stay positive throughout the test. |
| Answer Review | Use remaining time to review answers for mistakes. |
By incorporating these strategies into your preparation and test-taking process, you can approach the assessment with confidence and improve your overall performance. Preparation and a well-planned approach are essential for success in any high-stakes test, particularly when the health and safety of pediatric patients are at stake.
Resources for PALS Exam Preparation
When preparing for high-stakes assessments, having access to the right materials can make a significant difference. Utilizing reliable resources will help solidify your understanding of critical concepts, improve recall, and enhance your confidence. From textbooks to online platforms, a variety of tools are available to support your study process and ensure that you are fully prepared for the challenge ahead.
Key Resources for Study
Below is a list of useful study materials and platforms that can aid in your preparation:
- Textbooks: Comprehensive textbooks often provide detailed explanations, case studies, and practice questions to reinforce your knowledge.
- Online Courses: Many educational platforms offer online courses with video lectures, quizzes, and simulated scenarios to help you familiarize yourself with key concepts.
- Mobile Apps: Several mobile applications are designed specifically to help with reviewing essential protocols and guidelines through flashcards, quizzes, and interactive content.
- Practice Tests: Taking practice tests under timed conditions allows you to assess your progress and become familiar with the format of the assessment.
- Workshops and Study Groups: Engaging in workshops or forming study groups can provide collaborative learning opportunities and help you discuss complex topics with peers.
Websites and Online Platforms
In addition to physical books and classes, online resources can supplement your study materials. Consider using the following platforms for your preparation:
- Interactive Learning Platforms: Websites such as Khan Academy, MedCram, or online medical schools offer courses focused on pediatric care, emergency medicine, and related subjects.
- Official Guideline Websites: Websites like the American Heart Association or similar organizations often publish updated protocols and recommended practices that can be invaluable for studying.
- Educational Forums and Communities: Participating in online forums or communities like Reddit or Quora can help you get insights and advice from other professionals who have already completed the preparation process.
Additional Preparation Materials

| Resource Type | Purpose |
|---|---|
| Textbooks | Provide comprehensive material for in-depth understanding. |
| Online Courses | Offer video lectures and interactive content for visual learners. |
| Mobile Apps | Allow for on-the-go study with quick access to important material. |
| Practice Tests | Help simulate the test environment and track progress. |
| Study Groups | Provide collaborative learning and peer support. |
Incorporating these resources into your study routine can significantly enhance your preparation. By combining various types of learning tools, you ensure that you’re well-equipped to handle any questions or scenarios that arise during the assessment.
Understanding Pediatric Resuscitation Techniques
Effective resuscitation in children requires a deep understanding of both the physiological differences in pediatric patients and the appropriate techniques for restoring circulation and respiration. These techniques are designed to address emergencies where a child’s life is at risk, and they involve a series of steps aimed at ensuring the airway is clear, circulation is restored, and adequate oxygenation is achieved. Mastering these procedures is critical for healthcare providers working with young patients, as quick and accurate responses can make all the difference in the outcome of a pediatric emergency.
The main principles of pediatric resuscitation revolve around assessment, airway management, breathing support, and circulation restoration. These key components form the basis of life-saving interventions, but each step must be adapted to the unique needs of a child, considering factors such as age, size, and the underlying cause of the emergency. Knowledge of these techniques ensures healthcare professionals are equipped to provide the best care in high-pressure situations.
Key Medication Doses in Pediatric Emergencies
In pediatric emergencies, administering the correct medication dosage is crucial for effective treatment and patient safety. Proper dosing can vary greatly depending on the child’s weight, age, and medical condition. It is essential for healthcare providers to be familiar with the most commonly used medications and their recommended dosages to respond quickly and accurately in critical situations. This knowledge is vital to avoid complications or incorrect treatment during urgent care procedures.
Common Medications and Their Doses
| Medication | Recommended Dose | Route of Administration |
|---|---|---|
| Adrenaline (Epinephrine) | 0.01 mg/kg (1:10,000 solution) | Intravenous or intraosseous |
| Amiodarone | 5 mg/kg | Intravenous |
| Atropine | 0.02 mg/kg | Intravenous |
| Lidocaine | 1 mg/kg | Intravenous |
| Magnesium Sulfate | 25 mg/kg | Intravenous |
Important Considerations
While knowing the correct doses is vital, healthcare professionals must also be aware of factors that could affect drug effectiveness, such as the timing of administration and possible drug interactions. Reassessment of the patient’s condition is important to ensure that the treatment plan remains appropriate as the situation evolves. Additionally, the use of weight-based calculations is essential for achieving accurate dosing, especially in emergency pediatric care.
Common Mistakes to Avoid in Pediatric Emergencies
In critical care situations, especially when handling urgent pediatric cases, avoiding common mistakes can significantly improve outcomes. Many errors arise from miscalculations, lack of proper preparation, or misunderstanding of protocols. Being aware of these pitfalls and learning how to prevent them is essential for providing the best possible care to children in emergencies.
Failure to Perform Accurate Weight-Based Dosing
One of the most frequent mistakes is administering incorrect doses of medication due to improper weight-based calculations. Pediatric doses are often determined by a child’s weight, so failing to obtain an accurate weight or calculating it incorrectly can lead to underdosing or overdosing, both of which can have serious consequences.
Delaying Critical Interventions
In emergency situations, every second counts. Delaying critical interventions such as airway management, medication administration, or defibrillation can worsen a child’s condition. Rapid assessment and prompt action are key to stabilizing patients quickly.
Ignoring Updated Guidelines
Medical protocols and guidelines can change over time. Failing to stay updated with the latest guidelines and recommendations can lead to the use of outdated practices, which may not be as effective in treating patients as current methods. Regular training and review of the latest standards are essential to avoid this error.
Overlooking the Importance of Team Communication
Effective communication among team members is crucial during pediatric emergencies. Miscommunication or lack of clarity between team members can lead to confusion, incorrect actions, and delays in treatment. Ensuring that every team member understands their role and communicates effectively can help prevent these issues.
Inadequate Monitoring
During critical care, it is essential to monitor the patient’s vital signs continuously. Inadequate monitoring can lead to missed changes in the patient’s condition that require immediate attention. Ensure that all necessary equipment is set up and functioning, and continuously assess the child’s response to treatment.
Post-Test Tips and Certification Process
After completing a certification assessment, it is essential to take the right steps to ensure both a successful review of performance and understanding of the next steps in the credentialing process. This stage is crucial for consolidating knowledge and moving forward in one’s professional development. Whether you pass or need to retake the assessment, knowing how to proceed can help you stay on track.
Review Your Performance
Once the assessment is over, review any feedback or results you receive. Focus on the areas where you struggled and look for patterns in the questions or topics that caused difficulty. This process will help you identify gaps in knowledge that may need further study. Use this opportunity to reinforce weak areas and enhance your preparedness for the future.
Understand the Certification Process
Upon successful completion of the assessment, you will typically receive a certification that confirms your proficiency in critical pediatric care. This certificate is often valid for a set period, after which recertification is required. Ensure that you understand the recertification requirements, as well as the frequency and any continuing education credits needed to maintain your credentials.
For those who do not pass the assessment on the first attempt, remember that retaking the test is often allowed. Take the time to review the materials thoroughly before scheduling the next attempt. Utilize practice questions and participate in review courses if necessary to boost your confidence and performance.