Accurate medical classification is essential for effective healthcare management and insurance processing. Professionals in the field must be adept at interpreting various conditions, procedures, and diagnoses to ensure proper documentation and reimbursement. A clear understanding of these processes is critical for minimizing errors and maximizing efficiency in patient care and billing systems.
As medical standards evolve, so too do the frameworks that govern classification practices. These updates bring new challenges, but also present opportunities for professionals to enhance their expertise. By examining real-world examples and engaging with new changes, healthcare providers can remain at the forefront of industry standards and offer the highest level of accuracy in their practices.
In this section, we will explore practical situations that showcase typical classification challenges, offering valuable insights into how to approach them. By addressing these examples in detail, we aim to strengthen your ability to tackle various cases confidently and proficiently.
ICD-10-CM Coding Scenarios with Answers 2025
Effective classification in healthcare requires precision, as every diagnosis and procedure must be matched to the appropriate code. This process is vital for proper billing, patient record-keeping, and insurance claims. Navigating this system can be complex, especially when new updates introduce changes to existing classifications. To gain mastery, it’s crucial to engage with practical examples and challenges, refining the ability to identify and apply the correct codes under varying circumstances.
In this section, we explore several real-world examples, presenting typical challenges faced by healthcare professionals when assigning medical classifications. These situations reflect common issues that may arise in daily practice, illustrating both the reasoning behind certain decisions and the potential pitfalls. By reviewing these examples thoroughly, you will enhance your understanding of the system’s nuances and increase your confidence in tackling similar cases.
Each example is followed by an explanation, allowing you to test your knowledge and reasoning skills. This approach not only helps in understanding the mechanics of the classification process but also in applying that knowledge in a practical, real-world context.
Understanding ICD-10-CM Coding Updates
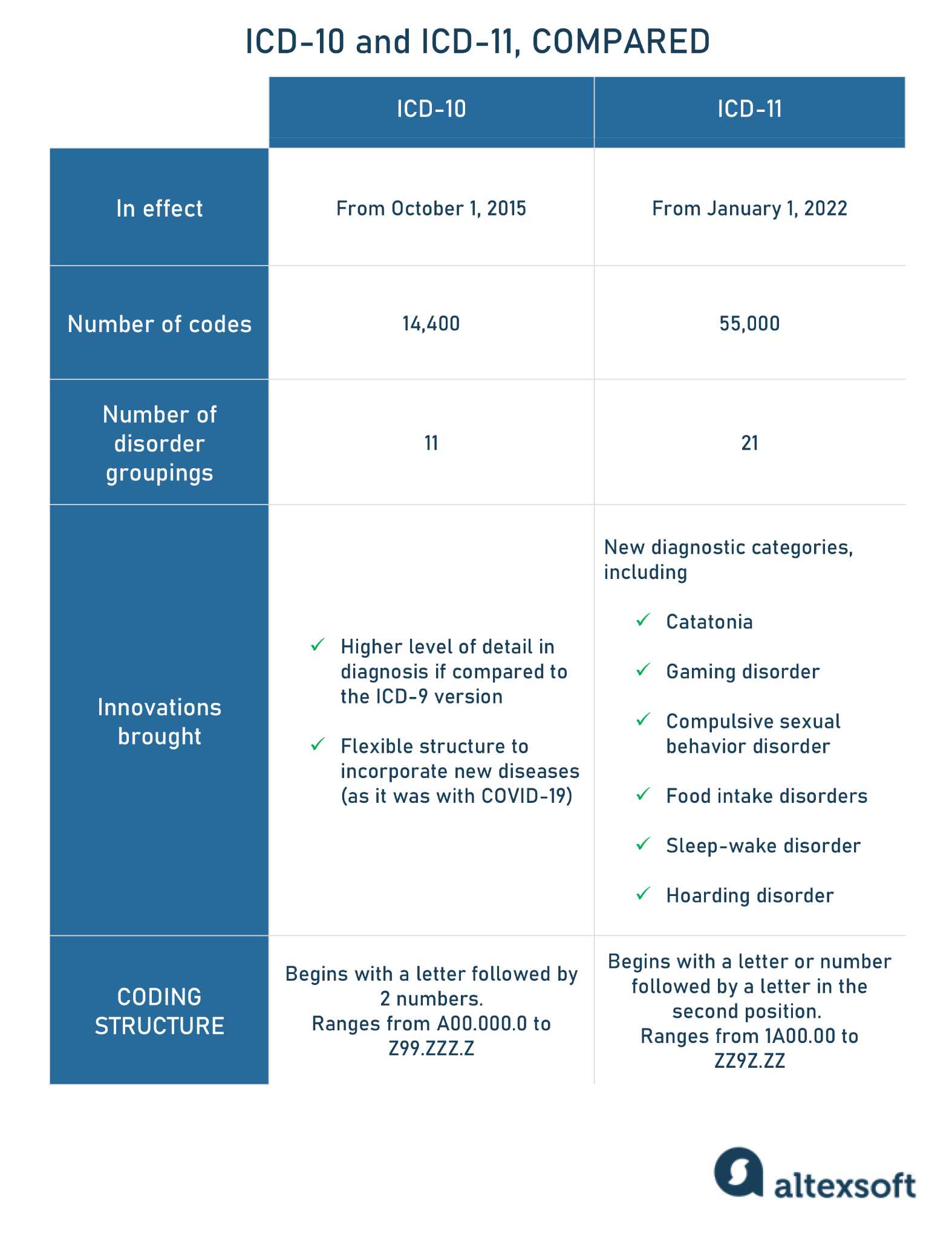
Healthcare classification systems are continually evolving to reflect advances in medicine, technology, and clinical practice. As new conditions, procedures, and treatments emerge, it’s essential for healthcare professionals to stay informed about updates to the standards that govern the way medical data is organized and recorded. These changes impact how diagnoses are documented, billed, and processed, making it crucial to understand the latest revisions.
Key Changes in Recent Updates
The most recent updates have introduced modifications to various codes, with some categories seeing expansions or reclassifications. This helps ensure that the system remains relevant and accommodates newly recognized medical conditions. Some updates also address common issues, such as the need for more precise or detailed classifications in certain areas of healthcare.
Impact on Healthcare Providers
For medical practitioners, the updates require not only a comprehension of the new rules but also a proactive approach to integrating these changes into daily workflows. Understanding the rationale behind these modifications can enhance the efficiency of documentation and reduce the risk of coding errors. Moreover, staying updated ensures compliance and smooth reimbursement processes for healthcare organizations.
Common Coding Mistakes to Avoid
While assigning medical classifications, accuracy is paramount. Even small errors can lead to significant issues, from incorrect billing to miscommunication in patient care. Many mistakes occur due to misunderstanding the guidelines, overlooking key details, or simply rushing through the process. Recognizing common pitfalls and actively working to avoid them is a critical step in improving overall efficiency and ensuring compliance with healthcare standards.
Top Mistakes to Watch Out For
- Using outdated codes: Failing to update codes according to the latest revisions can lead to inaccurate documentation and processing delays.
- Misinterpreting patient diagnoses: It’s crucial to ensure that diagnoses are accurately matched with the correct classification, considering all relevant details.
- Overlooking modifier usage: Ignoring the importance of modifiers or using them incorrectly can result in missed reimbursements or claim rejections.
- Incorrect sequence of codes: Assigning codes in the wrong order can affect how the condition or procedure is understood, potentially altering the reimbursement or treatment protocol.
How to Prevent Mistakes
- Stay updated: Regularly review the latest updates and revisions to ensure compliance with the newest standards.
- Double-check details: Always verify patient diagnoses and procedures before finalizing the classification to avoid errors.
- Utilize available resources: Make use of coding tools, reference guides, and expert advice to clarify any uncertainties.
- Prioritize accuracy over speed: Taking the time to thoroughly check each entry can prevent many common mistakes that occur under time pressure.
Key Changes in 2025 ICD-10-CM Codes
The medical classification system undergoes periodic revisions to reflect advances in medical research, new disease classifications, and emerging treatments. The 2025 updates introduce significant changes that healthcare professionals must understand to ensure accurate documentation and compliance. These modifications enhance the specificity of codes, improve efficiency, and address gaps in previous versions.
Notable Modifications and Additions
- Expanded diagnostic categories: New conditions and diseases have been added to accommodate emerging health concerns, ensuring more precise categorization of diagnoses.
- Updated code descriptions: Some codes now include more detailed descriptions, which provide clearer guidance on correct usage and reduce ambiguity.
- Revised codes for common procedures: Adjustments have been made to the codes for frequently performed medical procedures to reflect new methodologies and improved technologies.
- New subcategories for specific conditions: Some illnesses and conditions now have subcategories that allow for better differentiation and more accurate classification.
Impact on Healthcare Practice
- Improved precision: With these updates, healthcare providers can more accurately record patient conditions, reducing the risk of errors.
- Enhanced reimbursement: Correct application of new codes ensures smoother insurance claims and higher chances of full reimbursement.
- Faster processing times: By using more specific codes, the documentation process becomes more efficient, leading to quicker claim resolutions.
Step-by-Step Guide for Code Assignment
Assigning the correct medical classification requires a systematic approach to ensure accuracy and compliance. Each step must be carefully followed to avoid errors that could impact patient care, billing, and insurance claims. A structured process helps ensure that the right code is selected based on the available clinical information and guidelines.
1. Review the Documentation
Before selecting any codes, thoroughly review the patient’s medical record. Pay close attention to the diagnosis, procedures, and any additional notes that provide context. This ensures that you have a complete understanding of the patient’s condition or treatment plan, which is essential for accurate classification.
2. Identify the Key Terms
Once the documentation is reviewed, identify the key terms related to the condition or procedure. Look for specific details such as the type of illness, severity, and any complications. These terms will guide you in narrowing down the available code options.
3. Select the Appropriate Code
Using the identified terms, search for the corresponding classification in the official coding system. Ensure that the code selected reflects the precise nature of the condition or treatment. If there are multiple codes that could apply, choose the one that most accurately matches the documentation and guidelines.
4. Verify Code Accuracy
After selecting a code, double-check its description to confirm that it accurately reflects the medical record. Additionally, ensure that any modifiers or additional codes are correctly applied to capture all relevant aspects of the case.
5. Finalize and Document
Once the correct code has been selected, document it properly in the system. Ensure that all related information, including the code and any relevant details, is correctly entered into the patient’s record for future reference and billing purposes.
Effective Strategies for Accurate Coding
Achieving accuracy in medical classification requires more than just a basic understanding of the guidelines. It involves careful attention to detail, ongoing learning, and a proactive approach to addressing potential challenges. By adopting effective strategies, healthcare professionals can significantly reduce errors and improve the quality of documentation, which ultimately ensures proper reimbursement and compliance.
Key Approaches to Enhance Accuracy
- Regularly review updates: Keep up-to-date with the latest revisions and changes to the classification system to avoid using outdated codes.
- Double-check documentation: Always verify the details in the patient’s medical record to ensure that you are assigning the correct code for the diagnosis or procedure.
- Use coding tools and resources: Leverage available guides, software, and expert resources to assist in finding the correct code and to clarify any doubts you may have.
- Follow a structured process: Adopt a step-by-step approach to classification, ensuring that every relevant detail is considered before selecting a code.
- Minimize distractions: Create an environment that minimizes interruptions, allowing for focused and accurate code assignment.
Tools to Improve Accuracy
- Coding software: Use digital tools designed to streamline the classification process and automatically flag potential errors.
- Reference manuals: Keep updated manuals or online resources readily available for quick cross-checking of codes and definitions.
- Peer reviews: Engage in regular review sessions with colleagues or experts to ensure that the selected codes meet all relevant criteria.
Practical Examples of ICD-10-CM Codes
Understanding how medical classifications apply in real-world situations can enhance accuracy and comprehension. By looking at practical examples, healthcare professionals can gain insight into how specific conditions, treatments, and procedures are documented in the classification system. These examples provide a clear understanding of the correct application of codes in various scenarios, ensuring precise and efficient record-keeping.
For instance, when documenting a patient diagnosed with a common respiratory infection, it is essential to select the appropriate code that describes the type and severity of the infection. A code that simply mentions “respiratory infection” may not capture the full scope of the diagnosis. Instead, a more specific code reflecting the infection’s precise nature will ensure accurate billing and patient care.
Another example involves chronic conditions like diabetes. The selected code must reflect whether the diabetes is type 1 or type 2, as well as any complications such as neuropathy or retinopathy. By including these additional details, healthcare providers ensure that all aspects of the patient’s health are adequately documented, leading to better treatment outcomes and compliance with reimbursement standards.
In each case, carefully reviewing the documentation and applying the most specific code is key to accurate medical record-keeping and minimizing the risk of errors in insurance claims or patient care protocols.
How to Handle Complex Coding Scenarios
Complex medical cases often involve multiple conditions, treatments, or complications, making it challenging to select the correct classification codes. These situations require extra care and attention to detail to ensure accurate documentation and compliance. Properly handling these cases not only supports efficient billing processes but also ensures that patients receive the appropriate care based on their unique health circumstances.
Step-by-Step Approach
When faced with complex situations, a systematic approach is essential. Follow these steps to ensure that all relevant factors are considered:
- Gather all necessary information: Ensure that you have access to complete and up-to-date medical records, including diagnoses, procedures, and any relevant patient history.
- Identify primary and secondary conditions: Determine which condition is the primary reason for treatment, as this will typically guide your code selection. Secondary conditions or complications must also be documented separately.
- Review the guidelines: Each classification system provides specific guidelines for how to handle complicated cases. Make sure you understand the rules for selecting additional codes, modifiers, and sequenced conditions.
- Consider co-morbidities: Co-existing conditions may impact treatment and outcomes. These should be documented accurately to reflect the full complexity of the case.
Key Considerations
- Use of combination codes: Some complex cases can be captured with a single code that describes both the condition and its complications. Always check for these options to simplify the process.
- Clarify ambiguities: If there is any uncertainty about which code to use, consult with colleagues or refer to authoritative resources. Ambiguities should be resolved before finalizing the documentation.
- Accurate sequencing: The order in which codes are assigned is important, particularly for cases involving multiple conditions or treatments. Follow the correct sequencing rules to avoid errors.
By following these steps and maintaining attention to detail, healthcare professionals can ensure that even the most complex cases are accurately documented, reducing the risk of errors and improving overall patient care.
Impact of ICD-10-CM on Healthcare Providers
The adoption of a more detailed classification system has significantly transformed how healthcare providers document and manage patient information. This system enables a more precise representation of diagnoses and procedures, ultimately leading to improvements in patient care, billing accuracy, and overall healthcare management. However, the transition also presents challenges that require adaptation and consistent effort from all healthcare staff involved.
One of the primary benefits of the new classification system is its ability to enhance the specificity and granularity of medical records. This allows providers to capture a more comprehensive picture of a patient’s health, including the nuances of their conditions and any co-existing factors that may influence treatment plans. Such detailed documentation supports better clinical decision-making, as it ensures that all aspects of a patient’s health are considered.
On the flip side, the implementation of this system also brings about a significant increase in administrative workload. Healthcare providers must ensure that they are properly trained in using the classification system, keeping up with regular updates, and staying accurate in their code assignments. This can be time-consuming and may require additional resources, such as specialized software and ongoing staff training programs.
Furthermore, the accuracy of the classification system directly impacts financial operations. Correct coding is essential for proper reimbursement from insurance companies. Errors in documentation can lead to delays, claim denials, and financial losses for healthcare organizations. As such, healthcare providers are increasingly focusing on improving coding accuracy and efficiency to mitigate these risks.
Overall, while the shift to a more detailed classification system brings numerous benefits, it also requires careful attention and continuous effort to ensure that it positively impacts patient care and organizational success.
Tools to Improve Coding Efficiency
In today’s fast-paced healthcare environment, accuracy and speed in documenting patient diagnoses and procedures are essential. To streamline this process, various tools and technologies have been developed to help healthcare professionals enhance their efficiency and reduce the likelihood of errors. These tools not only improve productivity but also ensure that the documentation meets regulatory and reimbursement standards.
One of the most widely used tools is specialized software designed to assist in the selection and application of classification codes. These systems offer user-friendly interfaces, auto-suggestions, and real-time code validation, ensuring that the correct codes are applied quickly and accurately. With the help of such software, healthcare providers can reduce the time spent on manual lookup and improve overall coding precision.
Another valuable tool is the use of online databases and coding reference guides. These resources are regularly updated and provide detailed information on code updates, guidelines, and specific coding rules. By utilizing these references, healthcare professionals can stay informed about the latest changes and apply the most accurate classifications to each patient case.
Automated systems and artificial intelligence are also emerging as powerful allies in the healthcare industry. These technologies use machine learning to analyze patient records and suggest appropriate codes based on clinical data. As AI tools become more advanced, they hold the potential to significantly reduce the administrative burden on healthcare providers, allowing them to focus more on patient care.
Additionally, ongoing training and professional development play a crucial role in improving coding efficiency. Regular educational sessions, workshops, and certification programs ensure that medical coders stay up to date with the latest guidelines and best practices. This helps foster a culture of accuracy and continuous improvement in coding procedures across healthcare organizations.
By integrating these tools and practices, healthcare providers can enhance their workflow, reduce errors, and ensure that patients receive the best care possible while maintaining compliance with industry standards.
Tips for Mastering ICD-10-CM Guidelines
Becoming proficient in healthcare classification standards requires a deep understanding of the official guidelines and their applications. With the complexity of modern medical records and the precision needed for accurate documentation, mastering these guidelines is essential for healthcare professionals. In this section, we will explore strategies that can help you excel in applying classification rules effectively.
Stay Updated with Regular Revisions
One of the key aspects of mastering classification rules is staying up-to-date with regular revisions. These guidelines undergo updates and changes each year, making it crucial to follow official sources for the latest information. Make it a habit to check for updates from regulatory bodies and incorporate the changes into your practice. This will ensure that your knowledge remains current and you can avoid potential coding errors resulting from outdated information.
Utilize Available Resources and Tools
There are numerous resources available to help you navigate complex guidelines. Online coding tools, interactive manuals, and software solutions are designed to simplify the process by providing quick access to classifications and their respective rules. Take full advantage of these tools to enhance your accuracy and speed. These resources are designed to complement your knowledge and improve your efficiency in selecting the correct classifications.
Additionally, regularly reviewing official documentation and guides is crucial for reinforcing the rules. Consider creating a personalized cheat sheet for frequently used classifications and their application guidelines to improve your recall during practice.
Practice Consistently and Seek Feedback
Consistent practice is the key to mastering any set of guidelines. Engage in simulated case studies or work through practice examples regularly. This will help you become familiar with the structure and nuances of the classification system, allowing you to apply the rules more effectively in real-world scenarios. Don’t hesitate to seek feedback from more experienced colleagues or mentors to identify areas where you can improve your skills and understanding.
By integrating these strategies into your routine, you can build a strong foundation for mastering the classification guidelines and applying them accurately in your daily work.
Understanding Code Modifiers and Usage
In medical documentation, precision and clarity are critical, and modifiers play a key role in achieving this. These tools provide additional information about a procedure, diagnosis, or service, enhancing the level of detail recorded. When applied correctly, modifiers help to clarify nuances in patient care, enabling more accurate reimbursement and better tracking of healthcare services. This section explains the role of modifiers and how they are used to ensure a more precise and complete record of medical services.
What Are Modifiers?
Modifiers are symbols or numbers added to a primary code to provide more specific information about a procedure, diagnosis, or service. They may indicate that a service was altered in some way but not changed in its basic definition. For instance, they might denote a service performed in a different setting, a procedure that was partially completed, or a condition that requires more detailed attention. Understanding the various types of modifiers and their correct application is essential for maintaining accuracy in medical records.
Common Types of Modifiers
| Modifier | Definition | Example of Usage |
|---|---|---|
| 25 | Significant, separately identifiable evaluation and management service | Used when a physician performs a procedure in addition to a separate, distinct service on the same day. |
| 50 | Bilaterally performed procedure | Applied when a procedure is performed on both sides of the body, such as bilateral knee replacement. |
| 59 | Distinct procedural service | Indicates that a procedure or service was distinct or independent from other services performed on the same day. |
| LT | Left side | Used to indicate that a procedure was performed on the left side of the body. |
| RT | Right side | Used when a procedure is performed on the right side of the body. |
These examples illustrate how modifiers provide essential context, making it easier for healthcare professionals, insurers, and others involved in the care process to understand the full scope of the services provided. By correctly applying modifiers, providers ensure that patient records are more accurate, which can lead to better care, appropriate billing, and improved outcomes.
Mastering the use of modifiers is an essential part of effective medical documentation. When you understand when and how to apply them, you can contribute to more precise, accurate, and efficient healthcare practices. Always refer to the latest guidelines for modifiers and stay current on updates to ensure compliance and optimal use in practice.
How to Address Coding Challenges in 2025
As the healthcare industry evolves, so do the complexities of accurately documenting medical diagnoses and services. In 2025, coding professionals will face new obstacles, ranging from updates in classification systems to the increasing demand for detailed and precise data. Overcoming these challenges requires a combination of understanding the latest changes, utilizing effective tools, and developing strong attention to detail. This section explores strategies for addressing the most common issues that arise in medical documentation and offers tips for navigating the complexities ahead.
One of the primary challenges in the upcoming year is ensuring compliance with the revised guidelines. Healthcare providers and coders must stay updated on the most recent revisions and nuances to avoid errors. Additionally, the increasing volume of data means that professionals must be equipped to handle large amounts of information while maintaining accuracy and efficiency. Effective communication between clinical staff and coding professionals is essential for ensuring that all services are documented correctly and comprehensively.
To overcome these challenges, it’s important to focus on continuous education and leveraging advanced tools, such as coding software and decision support systems, which can help streamline the process. Additionally, fostering a collaborative environment where questions are encouraged and knowledge is shared can reduce the likelihood of mistakes. Regular training, practice, and awareness of common pitfalls can make a significant difference in ensuring that medical documentation remains accurate and compliant with current standards.
ICD-10-CM Coding Resources for Professionals
Professionals in the healthcare documentation field need reliable resources to stay updated and efficient in their work. As the landscape of medical classification systems evolves, it’s crucial for coders and healthcare administrators to have access to accurate, current materials that help them perform their tasks with precision. This section provides a guide to essential resources that can enhance the effectiveness and efficiency of medical coding professionals.
Key Resources for Healthcare Coders
- Official Coding Guidelines: The official documentation provided by regulatory bodies outlines the standards and best practices for accurate classification. Keeping up-to-date with these guidelines is critical for avoiding errors.
- Online Databases and Tools: Many tools allow professionals to search for specific codes, definitions, and updates. Websites like the CDC’s National Center for Health Statistics provide helpful resources for navigating coding systems.
- Professional Organizations: Associations such as the AAPC and AHIMA offer membership benefits, including access to webinars, newsletters, and professional forums where coders can stay informed about new developments.
- Training Programs: Formal educational resources are available through online courses, certifications, and workshops that provide in-depth understanding of coding practices and systems.
Using Technology to Enhance Accuracy
- Medical Coding Software: Advanced software solutions help professionals reduce human error by offering automated suggestions and identifying potential issues in documentation.
- Clinical Decision Support Systems: These systems can assist coders by providing insights into complex medical conditions and offering suggestions for proper classifications.
- Code Lookup Apps: Many mobile applications allow professionals to quickly reference codes, saving time and ensuring accuracy during the coding process.
By utilizing these tools and resources, healthcare professionals can enhance their accuracy, streamline workflows, and maintain compliance with evolving standards. Continuous learning and staying connected to the coding community will empower coders to overcome challenges and thrive in their roles.
Training and Certification for ICD-10-CM
Obtaining the proper training and certification is essential for professionals working with medical classification systems. As the standards for documentation and reporting evolve, it is vital for practitioners to stay current with industry expectations. Structured educational programs and certification paths not only enhance a professional’s understanding of medical coding practices but also increase their credibility in the healthcare field. This section covers essential training resources and the importance of certification for career development and success in healthcare administration.
Essential Training Programs
There are various training opportunities available to professionals looking to deepen their knowledge and improve their skills. These programs offer both fundamental and advanced levels of instruction, catering to individuals at all stages of their careers. Training can be obtained through online courses, in-person workshops, or community college programs, each designed to offer practical knowledge and a deep understanding of the systems used for medical classification.
- Online Courses: Many platforms provide flexible, self-paced learning environments that allow students to learn at their own pace, often leading to certification upon completion.
- Workshops and Seminars: These live sessions, either virtual or in-person, offer hands-on experience and insights from experienced professionals. They are ideal for individuals seeking real-world applications of medical classification systems.
- Community College Programs: Colleges often provide comprehensive programs that combine classroom learning with practical experience, preparing individuals for certification exams.
Certification Paths and Benefits
Certification plays a pivotal role in establishing credibility within the healthcare industry. Recognized certifications demonstrate a professional’s knowledge, competence, and adherence to the highest standards of medical classification. Some of the most well-known certifying bodies include the American Academy of Professional Coders (AAPC) and the American Health Information Management Association (AHIMA).
- AAPC Certification: AAPC offers various certifications that focus on different aspects of healthcare documentation, such as Certified Professional Coder (CPC) and Certified Inpatient Coder (CIC).
- AHIMA Certification: AHIMA offers certifications like Certified Coding Specialist (CCS) and Certified Health Data Analyst (CHDA), which focus on data management and coding expertise.
- Ongoing Education: Many certification programs require continuing education credits to maintain certification, ensuring that professionals stay up-to-date with industry standards and regulations.
Through proper training and certification, individuals can not only enhance their professional skills but also open doors to higher-paying roles and greater career opportunities in the healthcare sector. These credentials validate the knowledge necessary for accurate and efficient medical reporting, ensuring that healthcare organizations comply with current guidelines and regulations.
Commonly Asked Questions About ICD-10-CM
As healthcare documentation evolves, professionals frequently encounter questions regarding the use and application of medical classification systems. These inquiries often arise from the need to understand how to correctly report diagnoses, procedures, and services. This section provides answers to some of the most common questions, offering clarity on complex topics and ensuring accuracy in the application of coding rules and guidelines.
Frequently Encountered Inquiries
Below are some of the most common questions that healthcare providers, coders, and administrators have when working with medical classification systems:
| Question | Answer |
|---|---|
| What is the purpose of using a classification system? | The system is used to provide accurate and consistent reporting of diagnoses, procedures, and medical services, ensuring proper billing and effective patient care management. |
| How often do the coding guidelines get updated? | Updates typically occur annually, though occasional revisions may be made during the year to address emerging healthcare trends, technology, or regulatory changes. |
| Why is it important to follow coding conventions? | Following conventions ensures uniformity across the healthcare system, enabling accurate patient records, proper reimbursement, and compliance with legal and regulatory standards. |
| What should be done if a specific code does not apply? | If no specific code is available for a particular condition or service, coders should consult guidelines for appropriate alternatives, and sometimes report with an unspecified or other specified code. |
| How can healthcare professionals stay current with coding changes? | Healthcare professionals should engage in continuous education, attend training workshops, and refer to official updates and publications issued by authoritative organizations in the field. |
Understanding the Impact of Coding Decisions
Each decision made in the classification process can have significant implications for healthcare providers. From reimbursement to patient outcomes, it is crucial to ensure that coding practices adhere to the latest standards. Inaccurate reporting can lead to payment denials, compliance issues, or miscommunication of patient conditions.
By understanding these commonly asked questions and applying best practices, healthcare professionals can help ensure accurate, efficient, and effective reporting within their organizations.