For those pursuing certification in emergency medical response, understanding the core concepts and protocols is crucial. This guide is designed to assist candidates in navigating through the most important aspects of the assessment, helping them prepare effectively. Whether you are a first-time candidate or looking to refresh your knowledge, mastering these topics is key to achieving success.
Preparation requires more than just memorizing procedures; it involves a deep understanding of the skills and techniques that can save lives. Knowing the correct steps to take in critical situations, from managing breathing difficulties to administering medications, is vital. This section will cover the essential principles that you need to focus on, ensuring you are ready for real-world application.
Mastering these principles will help you gain confidence and perform well during the evaluation process. With thorough preparation, you can feel confident that you are equipped to respond appropriately in high-pressure situations, meeting all the necessary requirements for your certification.
ALS Certification Preparation Guide
Achieving certification in emergency medical procedures requires a strong understanding of key concepts, protocols, and practical skills. The assessment process is designed to evaluate your readiness to handle life-threatening situations with confidence and precision. This guide will provide essential insights and recommendations to help you navigate through the evaluation process and master the necessary skills.
To succeed in the certification process, it’s important to focus on the following areas:
- Comprehending critical patient care protocols
- Understanding the importance of quick decision-making in emergencies
- Mastering key medical procedures, from airway management to medication administration
- Building teamwork and communication skills for coordinated responses
In preparation for the evaluation, candidates should dedicate time to thoroughly review the course material. This includes understanding emergency response sequences, learning how to assess patient conditions accurately, and applying theoretical knowledge to practical scenarios. Practice is also essential to build muscle memory for performing critical interventions under pressure.
Moreover, successful completion requires familiarity with protocols for specific conditions, such as cardiac arrest, trauma, respiratory failure, and shock. Each of these requires precise and rapid intervention, and being familiar with the procedures will ensure that you can respond effectively.
It’s important to stay calm, focused, and aware during the assessment. Understanding the test format and practicing common scenarios will give you an edge, allowing you to demonstrate your knowledge and readiness in real-life situations. The more you practice, the more confident you will feel during the assessment, ensuring you meet all the required standards for certification.
What to Expect in the Assessment
When preparing for the evaluation, it’s essential to understand the structure and components that make up the process. The assessment is designed to test your knowledge, skills, and ability to perform under pressure in emergency situations. You can expect a combination of theoretical questions and practical scenarios that will challenge your ability to apply what you’ve learned.
The evaluation typically consists of two main parts: a written portion and a skills assessment. The written portion will cover various topics related to patient care, protocols, and procedures. The skills portion will test your hands-on ability to perform specific interventions accurately and efficiently. Both parts are crucial for demonstrating your competency in critical care situations.
| Assessment Component | Description |
|---|---|
| Written Test | Questions based on theory, protocols, and procedures to assess your understanding of key concepts. |
| Skills Evaluation | Practical scenarios where you demonstrate your ability to perform medical interventions under simulated conditions. |
| Team-Based Exercises | Group activities to evaluate communication, coordination, and teamwork during emergencies. |
It’s important to review all course materials thoroughly, as questions may cover a wide range of topics. Expect to be tested on your ability to prioritize tasks, assess patient conditions, and make critical decisions quickly. Additionally, you will be evaluated on your ability to collaborate with others, as effective communication is key in real-world emergency scenarios.
While the assessment may feel intense, it is designed to ensure that you are fully prepared to handle high-pressure situations in a professional and competent manner. With proper preparation and practice, you will be ready to demonstrate your skills and knowledge confidently.
Key Concepts for Critical Care Training
In the process of obtaining certification for emergency response, there are several essential principles that form the foundation of effective patient care. Understanding these core concepts is crucial for handling medical emergencies with efficiency and precision. This section will cover the most important areas of focus, from patient assessment to intervention strategies, that will help you successfully navigate the certification process.
Patient Assessment and Prioritization
One of the first steps in managing any emergency situation is assessing the patient’s condition accurately. This involves identifying the severity of their symptoms and prioritizing interventions accordingly. Key techniques include evaluating airway patency, breathing, circulation, and neurological status. The ability to quickly and correctly assess a patient’s condition can be the difference between successful recovery and deterioration.
Critical Interventions and Protocols
Knowing the correct medical procedures to apply in life-threatening situations is paramount. This includes understanding how to manage respiratory distress, cardiac arrest, shock, and other severe conditions. Each protocol provides specific guidelines for action, such as drug administration, airway management, and the use of equipment like defibrillators. Familiarity with these protocols ensures that you respond promptly and correctly in high-stress environments.
Mastering these core concepts, along with regular practice, will enable you to perform with confidence and competence when faced with emergencies. The ability to make informed decisions quickly, based on these fundamental principles, is essential for ensuring positive patient outcomes in critical care situations.
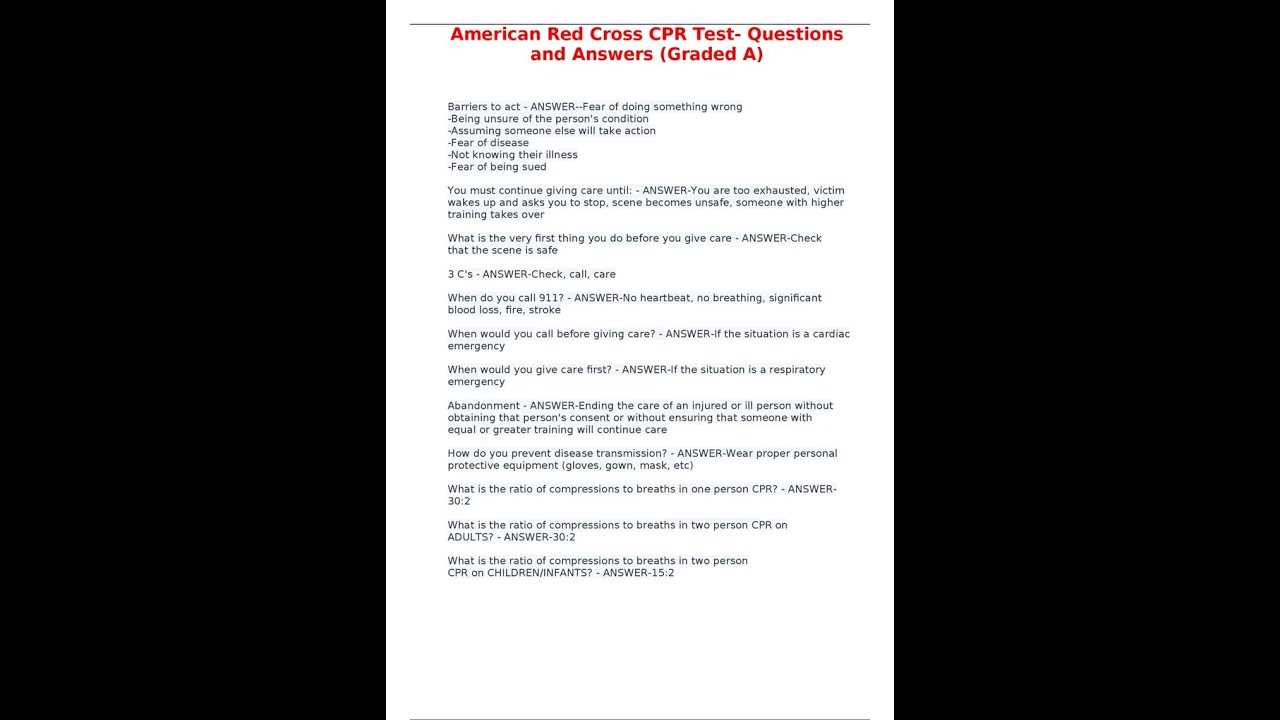
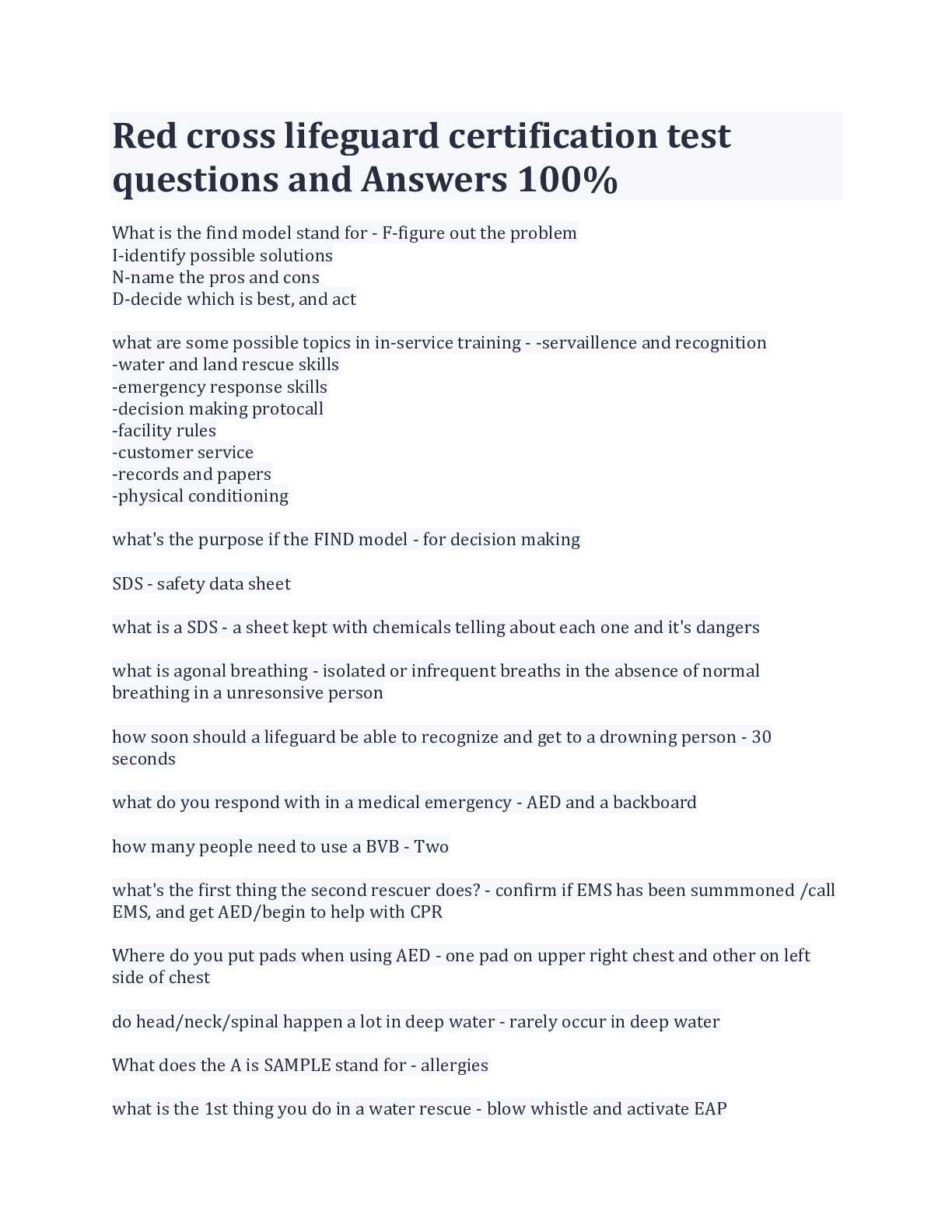
Commonly Asked Questions in ALS Evaluation
During the certification process for emergency care, candidates can expect to encounter a variety of questions that test their knowledge of essential medical protocols and procedures. These questions are designed to assess your understanding of both theoretical concepts and practical application. Being familiar with the most commonly asked questions can help you prepare effectively and build the confidence needed to succeed in the assessment.
Typical questions may cover a range of topics, including patient assessment techniques, treatment priorities, and intervention strategies. You might be asked to identify the correct steps to take in various emergency situations, such as cardiac arrest or severe trauma. Additionally, questions may focus on the use of medical equipment and medications, as well as the proper sequence of actions to optimize patient outcomes.
Understanding these key areas and practicing with sample questions can help you approach the evaluation with a clear strategy. It’s important to focus on both the theoretical knowledge and the practical skills that are essential for delivering high-quality care in critical situations.
How to Prepare Effectively for the Test
Proper preparation is key to performing well in any certification assessment for emergency response. It requires a structured approach that combines both theoretical study and hands-on practice. Focusing on core concepts, understanding key protocols, and mastering practical skills will give you the confidence needed to succeed in the evaluation process.
Study Key Concepts Thoroughly
Begin by reviewing the core material that will be covered in the assessment. Ensure that you understand the essential concepts, such as:
- Patient assessment and prioritization techniques
- Intervention strategies for various medical emergencies
- Proper use of medical tools and equipment
- Pharmacology and drug administration protocols
- Team coordination and communication during critical situations
Use study guides and textbooks to reinforce your knowledge and fill in any gaps. Pay special attention to areas where you may feel less confident, and review any relevant case studies to deepen your understanding.
Practice Hands-On Skills
While theoretical knowledge is important, being able to perform medical interventions effectively in real-world scenarios is equally crucial. Practice the following:
- Airway management techniques, such as intubation and oxygen administration
- Performing CPR and defibrillation procedures
- Administering medications according to established protocols
- Coordinating with a team to manage emergencies effectively
Participate in hands-on workshops, simulation exercises, or mock drills to apply your skills in controlled settings. Practicing under pressure helps build muscle memory and prepares you for the fast-paced environment of an actual emergency.
By combining focused study with practical training, you will be well-prepared to handle the challenges of the certification assessment and demonstrate your ability to respond to medical emergencies with competence and confidence.
Study Tips for Passing the Certification Assessment
Preparing for an emergency care certification involves more than just memorizing facts. It requires a strategic approach to ensure that you understand the key concepts and are able to apply them effectively during the evaluation. With the right study habits and focus, you can significantly improve your chances of success.
Here are some practical tips to guide your study process:
- Create a Study Schedule: Plan out your study sessions in advance. Allocate time for each topic and stick to your schedule to ensure you cover all areas thoroughly.
- Use Practice Questions: Practice with sample questions or mock tests to familiarize yourself with the format and types of questions you might encounter. This will help build your confidence and identify any weak areas.
- Focus on Key Procedures: Ensure you fully understand the critical interventions and protocols. Pay special attention to high-priority skills like CPR, airway management, and drug administration.
- Group Study: Studying with peers can be an effective way to reinforce your knowledge. Discuss complex scenarios and test each other’s understanding to solidify your learning.
- Visual Aids and Diagrams: Using visual aids such as charts, diagrams, and flowcharts can help simplify complex concepts and make them easier to remember.
- Review Real-Life Scenarios: Consider real-world applications of the concepts you’re learning. Understanding how theoretical knowledge is applied in actual emergency situations will make it easier to recall information during the assessment.
By adopting these study techniques and staying consistent with your preparation, you’ll be better equipped to perform well during the assessment and demonstrate your ability to handle high-pressure situations with confidence.
Understanding Cardiac Arrest Protocols
Cardiac arrest is one of the most critical medical emergencies, requiring immediate and effective action. The protocols for managing this condition are designed to stabilize the patient and restore normal heart function as quickly as possible. Understanding these protocols is crucial for anyone involved in emergency care, as they outline the specific steps to follow in high-pressure situations.
Initial Assessment and Immediate Response
The first step in managing a patient in cardiac arrest is to assess their condition rapidly. This involves checking for responsiveness and signs of breathing. If the patient is unresponsive and not breathing normally, immediate intervention is necessary. The protocol typically involves:
- Calling for help and activating the emergency response system
- Beginning chest compressions to circulate blood to vital organs
- Using an automated external defibrillator (AED) if available to assess the need for a shock
These actions must be performed without delay to improve the chances of survival, as the lack of oxygenated blood flow to the brain and heart can lead to irreversible damage within minutes.
Advanced Interventions and Ongoing Care
If initial interventions are unsuccessful, advanced protocols may be employed. These include the administration of medications, advanced airway management, and continuous monitoring of the patient’s vital signs. The primary goal is to stabilize the patient enough to transfer them to more advanced care, such as a hospital, where specialized treatment can be provided.
Protocols also emphasize the importance of teamwork and coordination, as multiple responders may be involved in the care of the patient. Clear communication and effective delegation of tasks are essential for optimizing patient outcomes in these high-stakes situations.
Respiratory Emergencies in ALS Training
Respiratory emergencies are among the most common and critical situations faced in emergency care. They require quick, precise interventions to restore adequate oxygenation and prevent further complications. Effective training in managing respiratory distress is essential for all healthcare professionals involved in critical care, as it enables them to identify and address respiratory issues before they lead to life-threatening consequences.
In this section, we will cover the primary types of respiratory emergencies and the key steps involved in their management. Properly assessing the airway, breathing, and circulation is vital for ensuring that the patient’s respiratory function is supported adequately.
Common Respiratory Emergencies
Respiratory distress can arise from a variety of conditions, each requiring different interventions. Some of the most common emergencies include:
- Airway Obstruction: Partial or complete blockage of the airway, often caused by foreign objects, swelling, or injury. Immediate clearing of the airway is crucial.
- Asthma Attacks: Severe narrowing of the airways due to inflammation, causing difficulty in breathing. Medication and oxygen therapy are typically used for management.
- Pneumothorax: The presence of air in the chest cavity, which can collapse the lung and impair breathing. Emergency needle decompression may be required to relieve pressure.
- Respiratory Failure: Inability of the lungs to exchange oxygen and carbon dioxide effectively, which may require advanced airway management or mechanical ventilation.
Steps for Managing Respiratory Emergencies
The primary goal in handling respiratory emergencies is to ensure that the patient receives sufficient oxygenation and ventilation. The following steps are typically taken:
- Initial Assessment: Quickly evaluate the patient’s airway, breathing, and circulation. Look for signs of distress such as labored breathing, cyanosis, or altered mental status.
- Airway Management: If the airway is compromised, clear any obstructions and secure the airway using techniques like suctioning or advanced airway devices.
- Oxygen Therapy: Administer oxygen through a mask or other devices to improve oxygen saturation levels, especially if the patient is hypoxic.
- Medication Administration: For conditions like asthma or allergic reactions, medications such as bronchodilators or corticosteroids may be required to reduce inflammation and improve airflow.
- Advanced Care: In cases of severe respiratory failure, advanced interventions like intubation or mechanical ventilation may be necessary to maintain the patient’s breathing.
Through focused training and hands-on practice, healthcare providers can develop the skills needed to respond rapidly and efficiently to respiratory emergencies, ultimately improving patient outcomes in critical care situations.
Advanced Airway Management Strategies
Proper airway management is a cornerstone of critical care, particularly in emergency situations. When a patient’s airway is compromised, immediate intervention is essential to ensure oxygenation and prevent further deterioration of their condition. Advanced techniques are often required when basic methods, such as simple airway positioning or the use of oxygen masks, fail to maintain adequate airflow.
In this section, we will discuss several advanced methods used to secure and manage an airway effectively, ensuring that healthcare providers can intervene quickly and appropriately when faced with life-threatening conditions.
Endotracheal Intubation
Endotracheal intubation is one of the most commonly used methods to secure a patient’s airway in cases of respiratory failure. It involves the insertion of a tube through the mouth or nose into the trachea, which allows for direct ventilation and provides a secure route for oxygen delivery. This method is especially crucial in situations where the airway is at risk of complete obstruction or where long-term airway support is necessary.
- Indications: Respiratory failure, unconsciousness, trauma, or significant airway obstruction.
- Procedure: After sedating the patient, a tube is inserted into the trachea, often guided by a laryngoscope. Proper placement must be confirmed through techniques such as capnography or auscultation.
- Advantages: Provides a secure airway, allows for mechanical ventilation, and protects the lungs from aspiration.
- Risks: Trauma to the airway, incorrect placement, and possible complications such as infection.
Supraglottic Airways
Supraglottic airways are an alternative to endotracheal intubation when immediate access to the trachea is not possible or when intubation proves difficult. These devices, such as the laryngeal mask airway (LMA) or the i-gel, sit above the glottis and provide an unobstructed passage for air to flow into the lungs.
- Indications: Difficult intubation, respiratory distress in an unconscious patient, or situations where a less invasive airway is preferable.
- Procedure: The device is inserted into the pharynx and secured, providing a seal around the airway without the need for advanced visualization or tube placement in the trachea.
- Advantages: Easier to insert compared to endotracheal tubes, less invasive, and can be used in emergencies when intubation is not possible.
- Risks: May not provide as secure a seal as intubation, and there is a potential for aspiration if not properly positioned.
Cricoid Pressure and Surgical Airway Techniques
In some critical situations, where conventional methods fail, cricoid pressure or surgical interventions may be required to establish a secure airway. Cricoid pressure involves applying pressure to the cricoid cartilage to prevent aspiration during intubation or in cases of severe trauma.
- Indications: When airway obstruction is severe or other methods have been unsuccessful in securing the airway.
- Procedure: Cricoid pressure is applied to the cricoid ring during intubation, and surgical airways like cricothyrotomy are used in extreme cases.
- Advantages: Provides a definitive airway when other methods are not effective.
- Risks: Surgical interventions carry inherent risks of infection, bleeding, and damage to surrounding structures.
In each of these strategies, the goal is to restore airway patency quickly and effectively. Mastery of these techniques is critical for healthcare professionals, ensuring they can provide optimal care in emergency and life-threatening situations.
Pharmacology in Advanced Life Support
The role of medications in critical care is essential for stabilizing patients in life-threatening situations. Pharmacological interventions are used to manage and treat a variety of conditions, such as cardiac arrest, respiratory failure, and shock. Understanding the appropriate use of medications, their effects, dosages, and potential side effects is crucial for healthcare providers in emergency scenarios.
In this section, we explore key pharmacological agents commonly used in critical care and their specific indications, mechanisms of action, and administration methods. Mastery of pharmacology allows providers to make informed decisions and deliver timely interventions to improve patient outcomes.
Commonly Used Medications
- Adrenaline (Epinephrine): Often used in cases of cardiac arrest to stimulate the heart and increase blood pressure.
- Adenosine: Used to treat certain types of abnormal heart rhythms by slowing down the electrical activity of the heart.
- Amiodarone: An antiarrhythmic agent used to stabilize irregular heart rhythms, particularly in cases of ventricular fibrillation.
- Lidocaine: Used as an alternative to amiodarone in certain arrhythmias to stabilize the heart’s electrical activity.
- Atropine: Helps in cases of bradycardia (slow heart rate) by blocking parasympathetic signals and increasing heart rate.
Dosage and Administration
Correct dosage and timely administration are critical in ensuring the effectiveness of pharmacological treatments. Medications are typically delivered intravenously in emergency settings for rapid action, though some can be administered via other routes, such as intraosseous or endotracheal tube. Accurate calculation of dosages based on patient weight, age, and clinical condition is essential to avoid complications.
- Administration Routes: Intravenous (IV), intraosseous (IO), endotracheal (ET), and sublingual.
- Dosage Calculations: Proper understanding of weight-based dosing, especially in pediatric cases, to avoid under or overdosing.
- Monitoring: Continuous monitoring of vital signs is crucial to assess the effectiveness of the drug and adjust dosages as needed.
Side Effects and Contraindications
While medications are often lifesaving, they can also carry potential risks. It is important for healthcare providers to be aware of possible side effects and contraindications, especially when dealing with patients with underlying conditions or multiple comorbidities.
- Adverse Reactions: These can include tachycardia, hypotension, arrhythmias, or allergic reactions. Providers must recognize these reactions and act promptly.
- Contraindications: Certain medications may not be suitable for patients with specific medical conditions, such as renal failure or severe hypotension. For example, amiodarone should be used cautiously in patients with thyroid disease.
- Drug Interactions: Be mindful of other medications the patient may be taking, as interactions can either diminish the effectiveness of the treatment or cause harmful effects.
Pharmacology plays a pivotal role in managing critical situations, and understanding the actions, indications, and potential risks associated with each drug allows healthcare providers to make informed decisions in high-pressure scenarios. Ongoing education and clinical practice are key to ensuring safe and effective use of medications in emergency care.
Recognizing and Treating Shock
Shock is a life-threatening condition that occurs when the body is not receiving adequate blood flow, leading to oxygen deprivation in vital organs. Recognizing the early signs of shock is crucial for providing immediate care and preventing further complications. Early intervention can significantly improve the chances of recovery and reduce the risk of permanent damage.
There are different types of shock, each with its own underlying causes, including hypovolemic, cardiogenic, neurogenic, and septic shock. Understanding these variations is important for selecting the right treatment approach based on the specific circumstances and patient needs.
Signs and Symptoms of Shock
Identifying shock requires careful observation of the patient’s symptoms. Some of the common signs include:
- Rapid heart rate: The body tries to compensate for low blood pressure by increasing the heart rate.
- Weak or thready pulse: Blood flow becomes insufficient, making the pulse difficult to feel or weak.
- Pale, cool, and clammy skin: Reduced circulation can cause the skin to appear pale and feel cold to the touch.
- Rapid or shallow breathing: The body attempts to increase oxygen intake due to reduced oxygen delivery.
- Confusion or disorientation: The brain is deprived of oxygen, leading to altered mental status.
- Low blood pressure: As blood volume decreases, blood pressure drops, which can be a critical indicator of shock.
Treatment for Shock
Prompt and appropriate treatment is essential to managing shock effectively. The goal is to restore blood circulation, increase oxygen delivery, and stabilize the patient’s condition.
- Positioning the patient: Lay the person down with their legs elevated to help improve blood flow to vital organs. In cases of suspected spinal injury, avoid unnecessary movement.
- Administer oxygen: Providing oxygen can help improve oxygen saturation in the blood and prevent organ damage.
- Control bleeding: If shock is caused by significant blood loss, apply direct pressure to stop bleeding and, if necessary, use a tourniquet.
- IV fluids: Administering intravenous fluids can help restore blood volume and improve circulation.
- Medications: Depending on the type of shock, medications may be used to support heart function, manage infection, or increase blood pressure.
In some cases, more advanced interventions may be required, such as the use of vasopressors to raise blood pressure or other specific treatments based on the type of shock. Monitoring vital signs, such as heart rate, blood pressure, and oxygen levels, is critical throughout the treatment process.
Recognizing shock in its early stages and providing immediate care are vital steps in improving patient outcomes. Medical personnel must act swiftly and decisively to restore normal circulation and prevent organ failure.
Effective Chest Compressions Techniques
Chest compressions are a critical component of resuscitation efforts during cardiac arrest. Proper technique is essential to maximize the efficiency of blood circulation, ensuring oxygen reaches vital organs. By understanding the mechanics and the appropriate force required, responders can provide effective chest compressions that significantly improve patient survival rates.
When performed correctly, chest compressions help maintain blood flow to the brain and heart, preventing irreversible organ damage. The following key principles guide the delivery of effective compressions.
Key Principles of Effective Chest Compressions
| Technique | Explanation |
|---|---|
| Hand Position | Place the heel of one hand in the center of the chest, just below the sternum. The other hand should be placed on top, interlocking fingers. This positioning ensures that force is applied directly to the chest. |
| Compression Depth | Compress the chest to a depth of at least 2 inches (5 cm) in adults. This depth is necessary to effectively pump blood to vital organs. |
| Compression Rate | The ideal rate is 100 to 120 compressions per minute. This rhythm is consistent with the body’s natural heart rate during resuscitation. |
| Allow Full Recoil | Allow the chest to fully recoil between compressions. This ensures that the heart refills with blood and maximizes the effectiveness of each compression. |
| Minimize Interruptions | Interruptions in compressions should be kept to a minimum. Consistent compressions increase the chances of a successful resuscitation. |
It is important to note that during cardiac arrest, it may be necessary to switch compressors regularly. This helps to avoid fatigue and maintain consistent pressure on the chest, especially in prolonged resuscitation attempts.
In addition to manual chest compressions, mechanical devices may be used in certain settings to assist with consistency and force, though manual compression remains the most commonly used technique in emergency situations.
By following these guidelines, responders can deliver effective chest compressions that contribute to the patient’s recovery or successful transition to advanced medical care. Prompt and effective action can mean the difference between life and death in critical situations.
Common Mistakes to Avoid During the Test
When preparing for a critical assessment, being aware of common pitfalls can make a significant difference in your performance. Many individuals make small yet impactful errors that can affect their understanding and application of key concepts. Recognizing these mistakes and learning how to avoid them is crucial for success. In this section, we will explore some of the most frequent issues that can arise during the evaluation process.
Understanding the content is not enough; it’s also important to demonstrate the ability to apply the knowledge effectively under pressure. Below are a few typical mistakes to be mindful of as you approach your assessment:
Pacing Yourself
One of the most common mistakes is rushing through the material without taking time to fully understand the questions. Speed may seem like an advantage, but rushing can lead to overlooking crucial details. Take your time to read each question carefully and consider all options before making a decision.
Misinterpreting Instructions
Another frequent issue is misunderstanding the instructions. Whether it’s a question asking for the best course of action in a specific scenario or a simple multiple-choice format, failing to follow instructions precisely can lead to incorrect answers. Always pay attention to keywords like “select all that apply” or “choose the most appropriate option.” These cues are designed to guide your responses.
Overlooking Practice Questions
Many test-takers focus only on theory and neglect practice questions. While theory is essential, applying that knowledge in a practical context is what will be tested. Practice questions allow you to familiarize yourself with the format and help identify areas where you may need more focus. Make sure to dedicate time to solving these questions and review the solutions carefully.
Second-Guessing Yourself
It’s natural to have doubts, but second-guessing yourself too often can be detrimental. If you have thoroughly thought through your response, stick with your initial answer. Overthinking can introduce unnecessary errors. Trust your training and instincts–more often than not, your first choice is the right one.
Failure to Manage Time
Time management is another key factor in performing well. Not allocating enough time to each section or spending too long on difficult questions can leave you with insufficient time to complete the test. Try to maintain a steady pace throughout the assessment and avoid getting bogged down on any single question for too long.
By avoiding these mistakes, you can approach your evaluation with greater confidence and clarity. Understanding the importance of careful consideration, following instructions, and practicing effectively will lead to a stronger performance. Keep these tips in mind, and you’ll be better prepared to succeed.
Role of Team Dynamics in ALS
In any emergency situation requiring complex medical interventions, effective teamwork is essential to achieving optimal outcomes. The ability to collaborate, communicate clearly, and make swift decisions can significantly impact the success of a critical event. In high-stress environments, especially those involving life-threatening conditions, understanding team dynamics is crucial for ensuring all roles are performed efficiently and correctly.
Team members must be prepared to work in harmony, each focusing on their specific responsibilities while supporting others. Successful coordination, mutual respect, and clear communication are the pillars that hold a team together during high-pressure scenarios. Below are some of the key aspects of team dynamics that contribute to effective management in critical situations:
Clear Role Definition
Each team member should have a well-defined role. Clarity on who is responsible for what ensures that no critical task is missed and helps avoid confusion. For example, one team member may be responsible for administering medication, while another might be focused on airway management. By clearly delineating roles, the team can work in sync to stabilize the patient.
Effective Communication
Communication is the foundation of team success. In emergency situations, clear and concise communication ensures that information is shared quickly and accurately. Miscommunication can lead to delays, errors, and potentially worse outcomes. Establishing protocols for communication, such as using concise phrases or specific cues, can help reduce misunderstandings during stressful moments.
Collaborative Decision-Making
In high-stakes situations, rapid decision-making is crucial. Teams must collaborate to assess the situation, weigh the options, and decide on the best course of action. This collaborative approach requires trust and mutual respect, as each team member brings unique expertise to the table. When decisions are made together, everyone can contribute, and there is less likelihood of missed opportunities for intervention.
Maintaining Calm Under Pressure
Remaining calm under pressure is a critical aspect of successful teamwork. High-stress environments can lead to confusion, anxiety, or poor judgment. However, when team members maintain composure, it sets a positive tone and encourages others to do the same. This calm demeanor allows for better focus, decision-making, and coordination.
Regular Debriefing
After a critical situation has been handled, it is important to conduct a debriefing session. This allows the team to reflect on what went well, what could have been improved, and how to enhance coordination for future incidents. Regularly discussing and reviewing past events strengthens the team’s cohesion and helps identify areas for further training and improvement.
- Clarify individual roles ahead of time
- Practice clear and concise communication techniques
- Foster an environment of trust and mutual respect
- Encourage collaboration in decision-making
- Remain composed in high-pressure situations
- Conduct post-event debriefs to learn and improve
By understanding and applying effective team dynamics, teams can ensure a more coordinated and efficient response during critical interventions. This collaboration plays a vital role in the overall success of managing emergencies and improving patient outcomes.
Managing Pediatric Emergencies in ALS
When dealing with critical conditions in young patients, healthcare providers must adapt their approaches to suit the unique physiological characteristics of children. Pediatric emergencies require specific knowledge, skills, and techniques to address the differences in anatomy, growth stages, and responses to medical interventions. Proper management of these situations is crucial, as the approach for adults does not always directly apply to children. Understanding these differences ensures the best possible care and outcome for pediatric patients in distress.
Key Considerations in Pediatric Care
Children are not just smaller versions of adults. Their bodies respond differently to trauma, illness, and medical treatments. Some important factors to consider include:
- Anatomical Differences: Children have a smaller airway, higher metabolic rate, and less developed organs compared to adults. These differences require modifications to techniques like intubation, CPR, and medication dosages.
- Age-Appropriate Dosing: Medications must be adjusted according to the child’s weight and age. Inappropriate dosages can lead to severe complications or insufficient treatment.
- Psychological Impact: Young patients may be scared or confused during emergencies. Providing comfort and reassurance is important, along with using strategies to minimize trauma during interventions.
Key Techniques for Pediatric Emergencies
Effective management of pediatric emergencies demands specialized techniques for intervention. Healthcare providers must be familiar with the following methods:
- Cardiopulmonary Resuscitation (CPR): For children, the approach to CPR differs from that for adults, particularly in terms of compression depth and the use of rescue breaths. The depth of chest compressions should be one-third of the chest’s diameter, and breath delivery must be gentle yet sufficient.
- Airway Management: Airway techniques should be adapted to the child’s age, with careful attention to the size and shape of their airway. Inserting an airway device may require special pediatric equipment, such as smaller-sized tubes or masks.
- Intravenous Access: When establishing IV access in children, it is often more challenging due to their smaller veins. Providers must know the proper technique to avoid injury while ensuring the patient receives fluids or medications as needed.
Furthermore, recognizing early warning signs of deterioration in children is crucial. Pediatric patients may not always present with the classic signs of distress observed in adults, making it important to stay vigilant for subtle changes such as altered behavior, increased irritability, or rapid breathing.
In summary, managing pediatric emergencies in critical care situations requires specific knowledge, appropriate techniques, and a careful, individualized approach. By adapting interventions to the unique needs of children, healthcare providers can enhance their ability to respond effectively and improve the chances of a positive outcome for young patients in need of urgent care.
ALS Certification Renewal Requirements
Maintaining the validity of professional credentials is essential for individuals working in emergency healthcare and critical care settings. Certification renewal ensures that practitioners are up-to-date with the latest protocols, practices, and guidelines necessary for effective patient care. The process typically involves a combination of continuing education, practical skill assessments, and sometimes a re-evaluation of theoretical knowledge to confirm that all required competencies are still met. Below is a guide to the renewal process for those seeking to keep their credentials current in this field.
Renewal Timeline and Frequency
For most certifications, renewal is required every two years. This period allows practitioners to refresh their skills and knowledge while keeping pace with changes in medical standards and protocols. Some key points about the renewal timeline include:
| Renewal Period | Required Actions | Notes |
|---|---|---|
| Every 2 Years | Complete Continuing Education (CE) courses | Ensures that practitioners remain current with evolving techniques and guidelines. |
| Every 2 Years | Complete Skill Demonstration and Competency Evaluation | Hands-on skills tests are often required to verify clinical abilities. |
| Varies by Certification | Submit a Renewal Application | Specific organizations may have different submission guidelines and deadlines. |
Key Requirements for Renewal
The following criteria are typically needed to complete the certification renewal process:
- Continuing Education: Completing a specific number of hours in relevant educational courses or workshops. This can include online modules, in-person classes, or simulation-based learning.
- Skills Competency: Demonstrating proficiency in key techniques and procedures through hands-on assessments. These may be conducted through practical scenarios or simulations designed to replicate real-life emergencies.
- Application Submission: Submitting the necessary documentation, including proof of education and skill assessments, to the certifying body before the expiration of the current certification.
It is also important to stay informed about changes to the certification standards, as guidelines and renewal procedures may evolve to reflect advancements in medical care or regulatory requirements.
By fulfilling these requirements, healthcare professionals ensure their continued competence and eligibility to perform in critical care environments, ultimately enhancing patient safety and care outcomes.
Final Review: Key Focus Areas
Preparing for an assessment in critical care involves identifying the most important topics to ensure comprehensive readiness. Focused study and review of the essential concepts can significantly improve performance, especially under pressure. This section highlights the major areas of knowledge that candidates should prioritize in their preparation. By concentrating on these key topics, you can ensure that you are equipped to handle a variety of emergency situations effectively.
Below are the crucial areas that require special attention as you prepare for the assessment:
- Cardiac Arrest Protocols: Understanding the correct sequence of actions, including chest compressions, defibrillation, and drug administration, is vital for managing patients in cardiac arrest.
- Airway Management: Effective techniques for maintaining and securing an airway, such as intubation and the use of airway adjuncts, should be reviewed thoroughly.
- Pharmacological Interventions: A deep understanding of common medications used in critical care, their dosages, and indications is essential. This includes drugs for managing arrhythmias, pain, and shock.
- Shock Recognition and Treatment: Knowing how to identify different types of shock (e.g., hypovolemic, cardiogenic, septic) and the appropriate interventions is crucial for successful outcomes.
- Team Communication and Roles: Effective communication and clear role delegation within a healthcare team are key to ensuring coordinated and efficient care during emergencies.
Focusing on these topics will provide a strong foundation for handling high-stakes situations, which is central to passing the assessment and delivering quality care in real-world scenarios. With careful review and practice, you will be ready to approach the assessment confidently and competently.