As a healthcare professional, understanding the complexities of medications is essential for providing effective patient care. This section delves into the core principles related to drugs, focusing on their actions, interactions, and impacts on various conditions. Mastering this knowledge helps ensure safe and informed decision-making in clinical settings.
Key areas covered include the classification of medicines, their proper usage, side effects, and the importance of precise dosages. The ability to identify potential drug interactions is crucial for preventing adverse outcomes and optimizing treatment plans for diverse patient groups.
By exploring these critical concepts, you will gain a deeper understanding of how to assess, administer, and monitor therapeutic agents. This foundation supports not only patient safety but also contributes to enhancing the quality of care delivered in any healthcare environment.
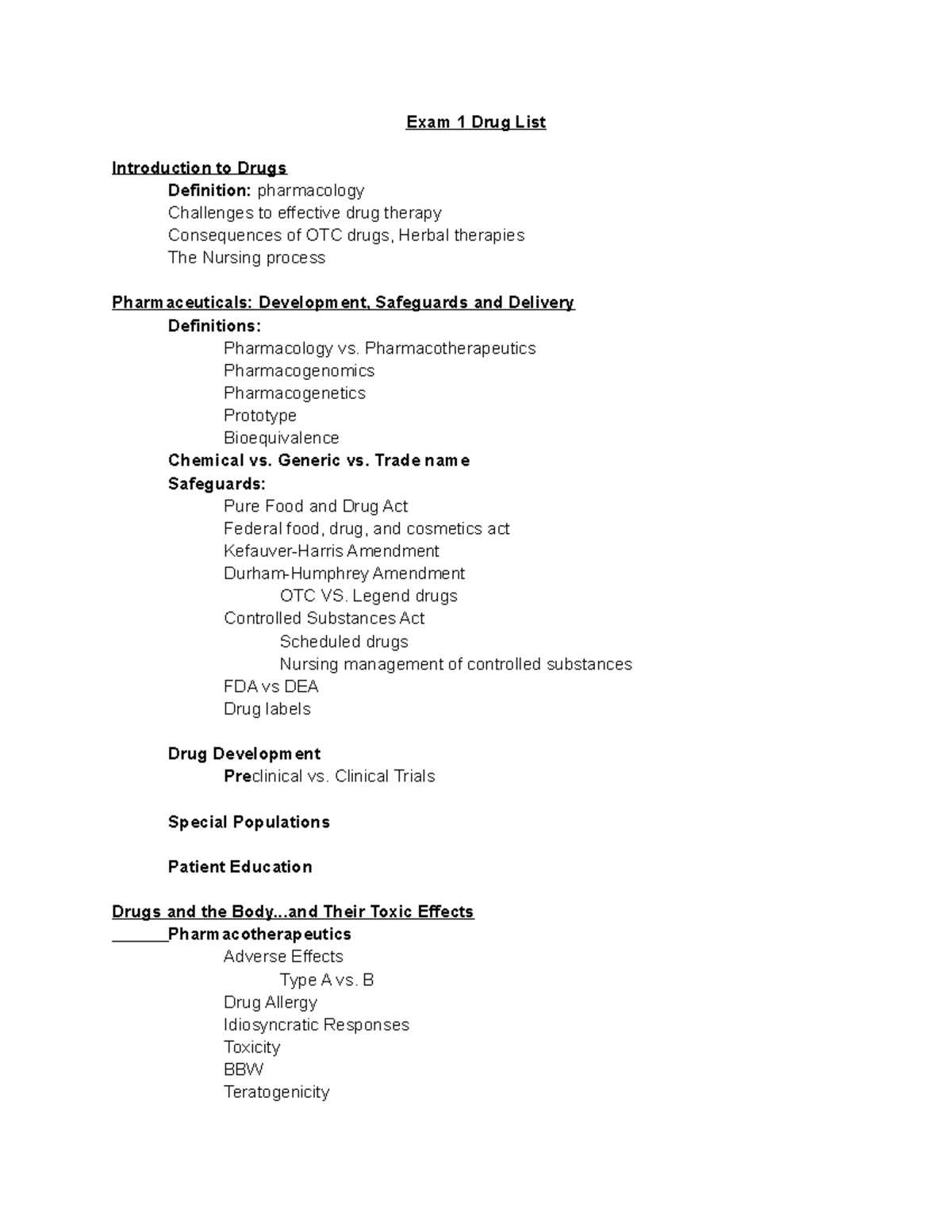
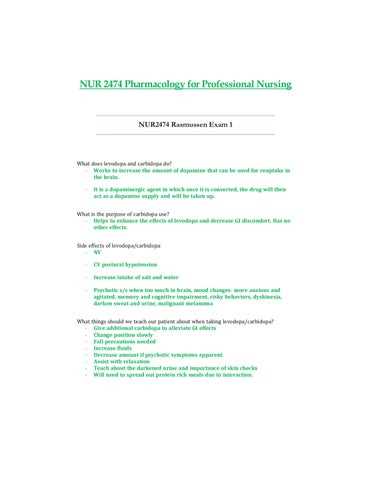
Nursing Pharmacology Exam 1 Study Guide
Mastering the principles of medication management is vital for healthcare professionals. This guide provides a structured approach to help you navigate the most important concepts related to drugs, their mechanisms, and proper usage. The following sections cover essential topics to ensure a solid understanding of how medications work, their side effects, and how to make informed clinical decisions.
Understanding Drug Classifications
One of the foundational elements is knowing how drugs are categorized. Various classes of medications serve different therapeutic purposes. Below are key categories you should focus on:
- Antibiotics
- Analgesics
- Antihypertensives
- Antidiabetics
- Cardiac agents
Key Concepts to Focus On
When preparing for assessments, focusing on the following concepts will help solidify your understanding:
- Mechanism of action
- Common side effects and adverse reactions
- Drug interactions and their impact on treatment
- Proper dosages and administration routes
- Monitoring and evaluating patient responses
By concentrating on these topics, you will be better equipped to handle complex clinical scenarios and ensure that patients receive the safest and most effective care possible.
Essential Concepts for Pharmacology Exams
To succeed in understanding medication management, it is crucial to grasp several key principles that form the backbone of therapeutic practices. These concepts serve as the foundation for safe and effective patient care, ensuring that professionals can administer, monitor, and adjust treatments accordingly. Focusing on these core areas will enhance your ability to navigate the complexities of drug therapies and interactions.
Among the most important concepts are drug classifications, the mechanisms through which drugs exert their effects, and the potential side effects that may arise during treatment. Additionally, understanding how different factors like age, weight, and medical conditions influence drug effectiveness and safety is essential. By mastering these principles, healthcare providers can make well-informed decisions, preventing complications and optimizing outcomes.
Key Drug Classes You Should Know
In clinical practice, knowing the major categories of medications is essential for understanding their specific actions and therapeutic uses. These drug classes not only help in identifying the right treatment but also provide insight into how different substances interact within the body. Below are some key drug categories that healthcare providers should be familiar with to ensure effective patient management.
Commonly Used Drug Classes
| Drug Class | Common Uses | Examples |
|---|---|---|
| Antibiotics | Treat bacterial infections | Amoxicillin, Ciprofloxacin |
| Analgesics | Relieve pain | Ibuprofen, Acetaminophen |
| Antihypertensives | Lower blood pressure | Amlodipine, Lisinopril |
| Antidiabetics | Control blood sugar levels | Metformin, Insulin |
| Cardiac Agents | Manage heart conditions | Digoxin, Beta-blockers |
Additional Classes to Study
In addition to the basic categories, it is also important to familiarize yourself with medications used for more specialized purposes. Understanding these agents ensures better clinical outcomes, especially when treating complex or chronic conditions. These may include:
- Anticoagulants – Used to prevent blood clots
- Antidepressants – For managing mood disorders
- Anticonvulsants – For seizure management
- Immunosuppressants – To manage autoimmune conditions
By mastering these drug classes and their applications, healthcare professionals can provide comprehensive care and enhance their ability to treat a wide range of conditions effectively.
Commonly Tested Pharmacology Terms
Understanding key terminology related to medications is crucial for effective clinical practice. These terms help professionals communicate clearly about drug actions, dosages, and patient management. Below are some essential terms that are frequently encountered in the study and practice of medicine, which will enhance your ability to work with various therapeutic agents.
Important Medication Terminology
- Absorption: The process by which a drug enters the bloodstream.
- Bioavailability: The proportion of a drug that reaches the systemic circulation.
- Half-life: The time it takes for the concentration of a drug in the body to reduce by half.
- Therapeutic Index: The ratio between the dose that causes a toxic effect and the dose that provides a therapeutic effect.
- Contraindication: A condition or factor that serves as a reason to withhold a certain treatment.
Key Drug Mechanism Terms
- Agonist: A substance that activates a receptor to produce a biological response.
- Antagonist: A substance that blocks or dampens the action of a receptor.
- Side Effect: A secondary, typically unwanted effect of a drug.
- Synergistic Effect: When two drugs work together to produce a stronger effect than the sum of their individual effects.
- Tolerance: A decrease in the effectiveness of a drug after repeated use.
Familiarizing yourself with these terms will help you better understand medication-related concepts, making it easier to administer treatments and monitor patient progress effectively.
Understanding Drug Mechanisms of Action
Comprehending how medications exert their effects on the body is crucial for effective patient care. Each drug interacts with specific biological targets to produce a desired therapeutic outcome. These interactions can involve receptors, enzymes, or other molecular structures, influencing various physiological processes. Understanding these mechanisms helps healthcare professionals predict how a drug will behave in the body and how it will interact with other treatments.
At the core of this understanding is the ability to recognize the different ways drugs influence biological systems. Some medications mimic or enhance natural body functions, while others block or inhibit certain processes. This knowledge allows for more precise prescribing and better management of patient responses to treatment.
Important Dosage Calculations for Nurses
Accurate medication dosing is essential to ensure patient safety and therapeutic effectiveness. Proper calculations are necessary to administer the correct amount of a drug based on a patient’s weight, age, and specific medical needs. Even small errors in dosage can lead to serious consequences, so it is crucial to have a solid understanding of dosage principles and methods.
Healthcare providers must be proficient in converting between different units of measurement, adjusting doses for special populations, and ensuring that prescriptions align with safe dosage guidelines. Mastering these calculations is an integral part of delivering high-quality care and preventing medication errors.
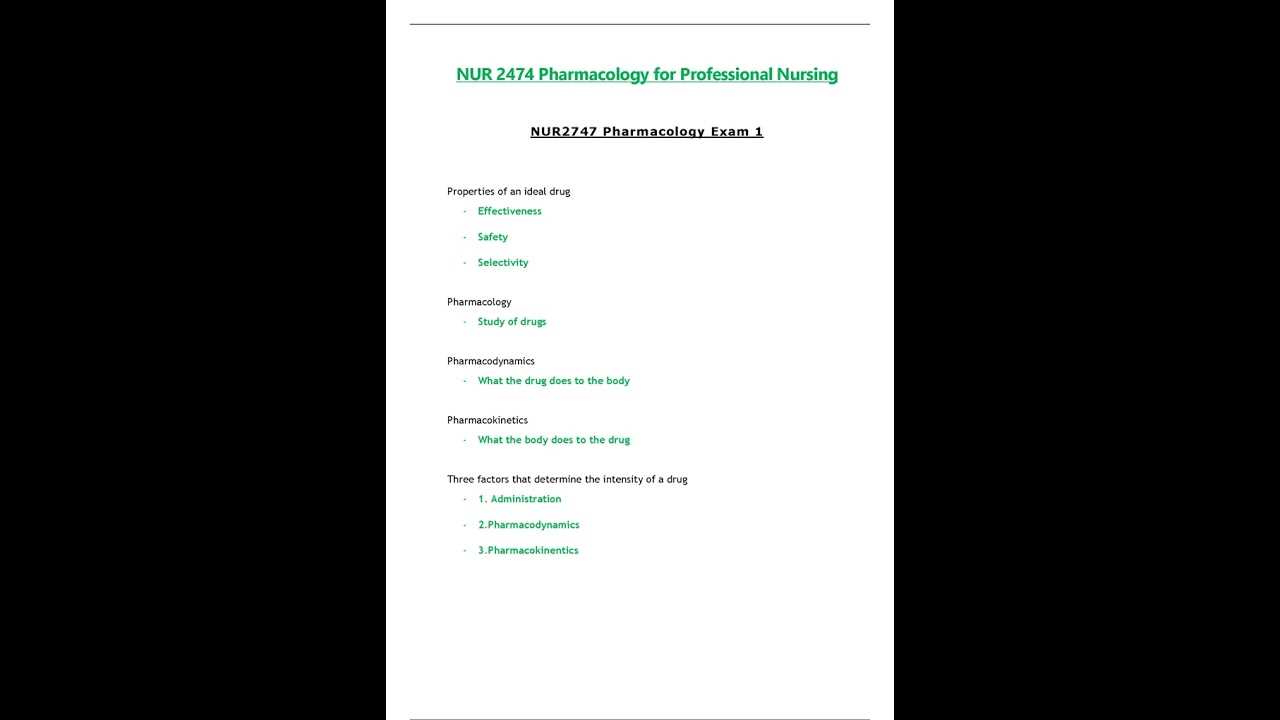
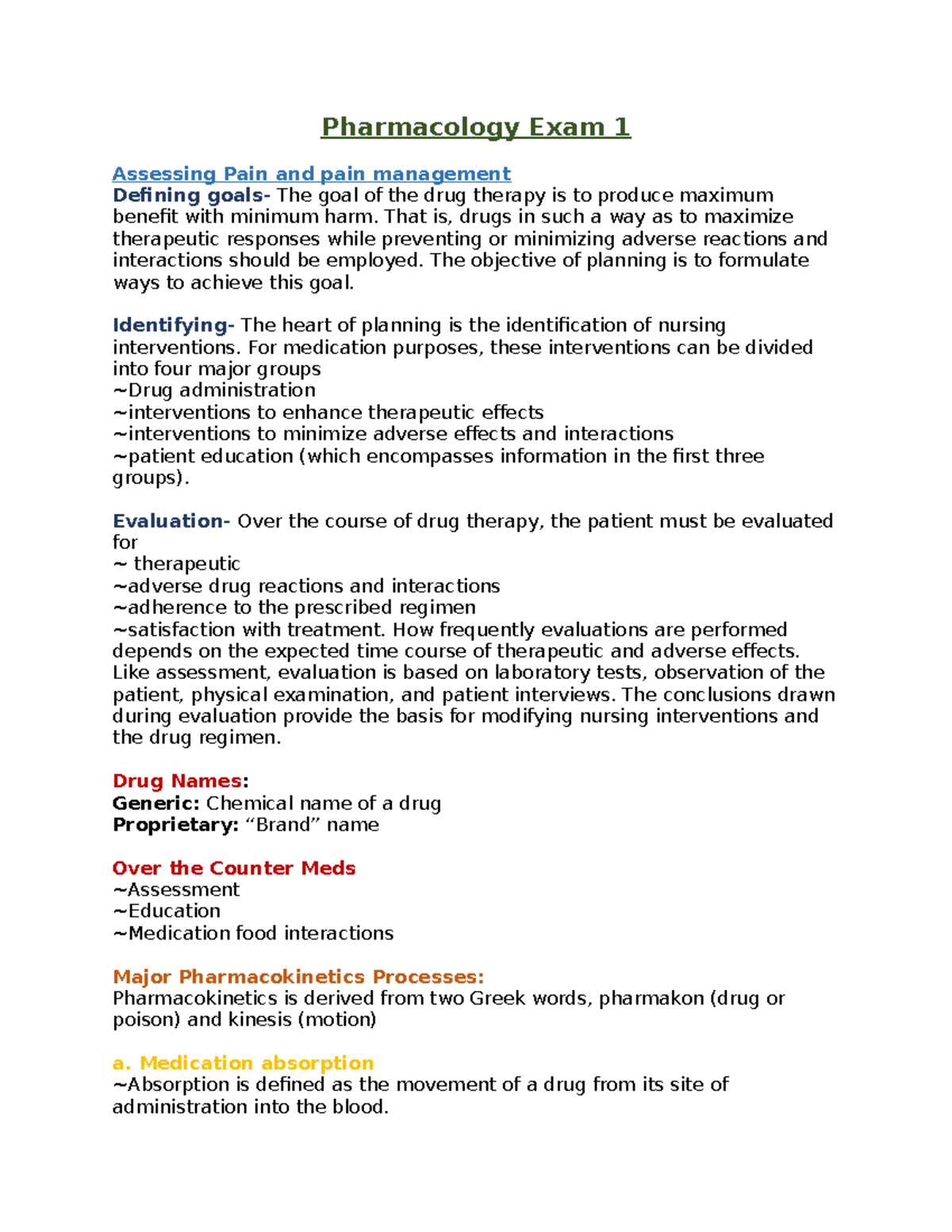
Pharmacokinetics and Its Relevance
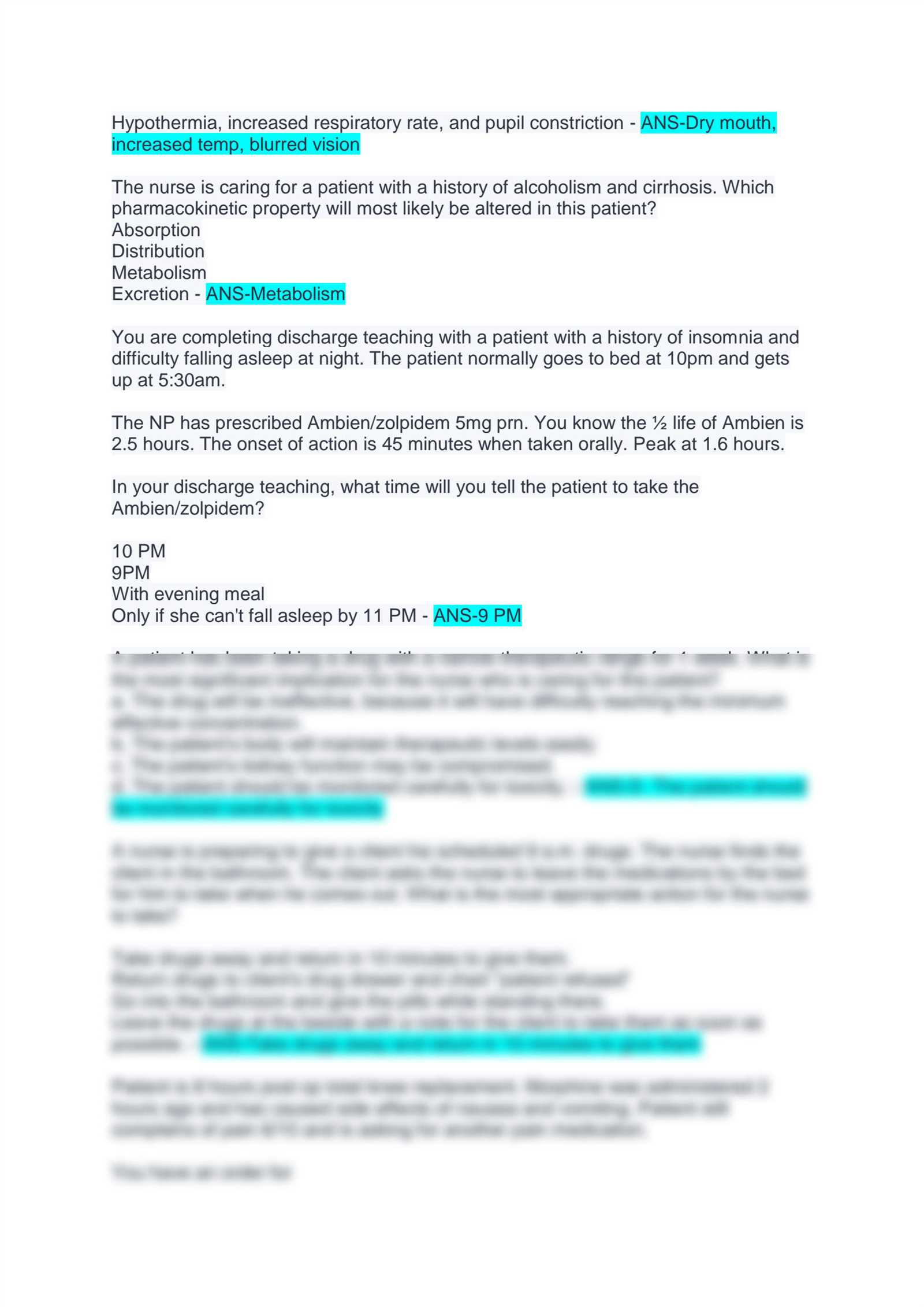
Understanding how the body processes medications is essential for ensuring effective treatment and minimizing risks. The movement of a drug through the body–from absorption to excretion–determines its action and therapeutic effect. The study of this process, known as pharmacokinetics, provides critical insights into how drugs are absorbed, distributed, metabolized, and eliminated.
Pharmacokinetics is particularly relevant in tailoring treatments to individual patients, as various factors such as age, liver and kidney function, and concurrent medications can affect how a drug behaves in the body. Knowing how these processes work helps healthcare providers optimize dosing and prevent potential complications.
Key Phases of Pharmacokinetics
- Absorption: The process by which a drug enters the bloodstream after administration.
- Distribution: The way the drug spreads throughout the body, reaching different tissues and organs.
- Metabolism: How the body breaks down the drug, often in the liver, making it easier to excrete.
- Excretion: The removal of the drug from the body, usually through the kidneys or liver.
By understanding these stages, healthcare professionals can predict the timing and duration of a drug’s effect, adjust dosages accordingly, and manage side effects more effectively.
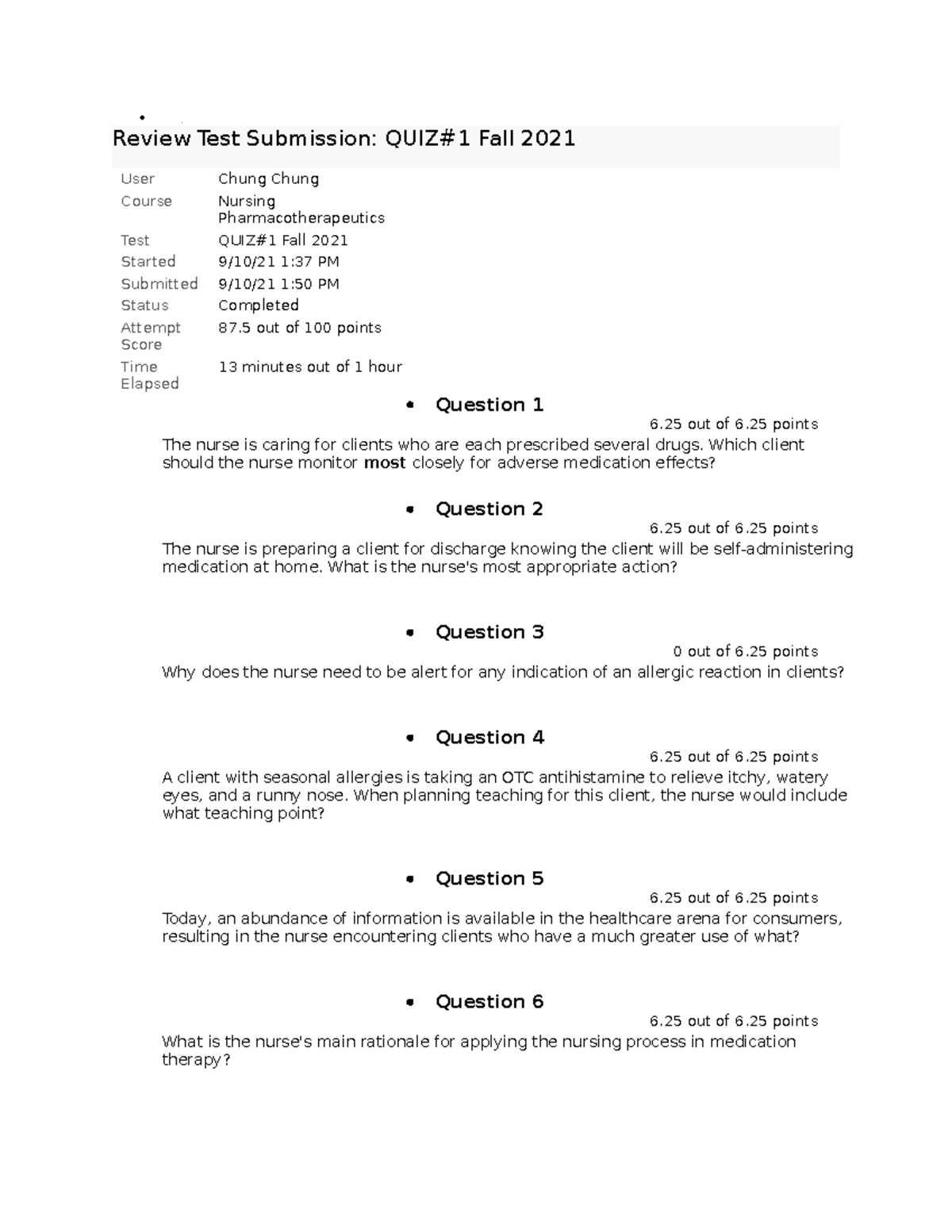
Top Nursing Pharmacology Practice Questions
Practice questions are an invaluable tool for mastering the concepts related to medication management. They help reinforce key knowledge and identify areas that may require further study. By regularly testing yourself on various topics, you can improve your understanding of drug actions, dosage calculations, and therapeutic applications.
This section provides some of the most frequently tested questions related to medication administration and treatment protocols. These questions cover a wide range of topics, from drug interactions to patient safety, and will help you prepare for real-world clinical situations.
Sample Practice Questions
- What is the first step when administering a new medication to a patient?
- How should the dosage of a medication be adjusted for elderly patients?
- Which of the following medications is most likely to cause an allergic reaction?
- What factors affect drug absorption in patients with gastrointestinal issues?
- What is the primary purpose of using a drug with a long half-life in treatment?
Answering Strategies
- Read each question carefully: Ensure that you understand what is being asked before selecting your answer.
- Apply clinical knowledge: Think about how the medication is used in practice, considering its mechanism and typical outcomes.
- Eliminate incorrect choices: Use logic to rule out answers that don’t fit the context or patient scenario.
- Review explanations: After answering, always check the explanations to deepen your understanding.
Regular practice with these types of questions will help you become more comfortable with drug-related scenarios, enabling you to make confident and informed decisions in clinical settings.
How to Approach Drug Interactions
Understanding drug interactions is crucial for ensuring patient safety and maximizing therapeutic efficacy. When multiple medications are taken together, they can influence each other’s effects, either enhancing or diminishing their action. These interactions can lead to unintended side effects, toxicity, or reduced effectiveness, making it essential to carefully assess the potential risks when prescribing or administering multiple treatments.
Approaching drug interactions requires a methodical strategy, considering factors such as the mechanism of action of each drug, the timing of administration, and the patient’s individual health status. Healthcare professionals must be aware of common interaction types and how they might affect patient outcomes.
Types of Drug Interactions
- Pharmacokinetic Interactions: These occur when one drug affects the absorption, distribution, metabolism, or excretion of another.
- Pharmacodynamic Interactions: These involve changes in the drug’s effect at the receptor site, which can either increase or decrease the drug’s action.
- Food-Drug Interactions: Certain foods can alter the effectiveness of medications by affecting their absorption or metabolism.
- Drug-Disease Interactions: Underlying medical conditions can modify the body’s response to specific medications.
Strategies for Managing Drug Interactions
- Thorough Assessment: Always review a patient’s current medication regimen, including over-the-counter drugs and supplements.
- Educate Patients: Make sure patients understand the potential risks of combining certain medications and encourage them to disclose all substances they are taking.
- Use of Drug Interaction Resources: Utilize reliable drug databases and tools to check for potential interactions before prescribing or administering medications.
- Monitor Patient Responses: Regularly assess for any unexpected side effects or therapeutic failures when multiple medications are prescribed.
By staying vigilant and informed about potential interactions, healthcare providers can significantly reduce the risks associated with polypharmacy and enhance patient care outcomes.
Pharmacology for Different Patient Populations
When administering medications, it’s essential to consider how various patient groups may respond differently to treatments. Factors such as age, gender, genetics, and underlying health conditions can significantly influence the way drugs are absorbed, distributed, metabolized, and eliminated. Understanding these variations helps healthcare providers tailor treatment plans to achieve optimal outcomes and minimize risks.
Specific patient populations, including children, the elderly, pregnant individuals, and those with chronic conditions, require special attention when it comes to drug therapy. These groups may have unique physiological characteristics that affect drug efficacy and safety, necessitating adjustments in dosing, frequency, or choice of medications.
Key Considerations for Different Populations
- Children: Pediatric patients may metabolize drugs faster or slower than adults. Drug dosages need to be adjusted based on weight and developmental stage.
- Elderly: Aging often leads to changes in kidney and liver function, which can affect drug clearance. Medications may need to be given at lower doses to avoid toxicity.
- Pregnant Individuals: Certain drugs can cross the placenta, potentially affecting fetal development. It’s important to assess the risks and benefits of any medication during pregnancy.
- Chronic Illness: Patients with liver, kidney, or heart disease may require adjusted doses or different medications due to impaired organ function.
By recognizing and addressing these factors, healthcare professionals can optimize therapeutic interventions and improve the safety and effectiveness of treatments for diverse patient populations.
Managing Adverse Drug Reactions
Adverse drug reactions (ADRs) are unwanted or harmful effects that occur when taking a medication, which can range from mild to severe. Recognizing and managing these reactions is critical for ensuring patient safety and improving therapeutic outcomes. ADRs can occur for a variety of reasons, including incorrect dosage, drug interactions, or an individual’s unique response to a particular medication.
Proper management of ADRs requires timely identification, appropriate intervention, and thorough monitoring. Healthcare providers must remain vigilant when administering medications, ensuring that any adverse effects are promptly addressed to avoid further complications. Education on potential side effects and patient monitoring are essential components of effective drug therapy management.
Strategies for Managing ADRs
- Early Detection: Regularly assess patients for signs of adverse reactions, especially after the introduction of a new medication.
- Adjust Dosage: In cases of mild reactions, reducing the dosage or switching to a different drug may be necessary.
- Discontinuation: In severe cases, stopping the drug and substituting it with a safer alternative may be required to prevent harm.
- Patient Education: Inform patients about the possible side effects of their medication and encourage them to report any unusual symptoms promptly.
- Monitoring and Follow-up: After any ADR is identified, continuous monitoring is crucial to assess the patient’s recovery and prevent further complications.
By addressing adverse reactions quickly and effectively, healthcare professionals can minimize risks and ensure that medications remain safe and effective for their intended use.
Critical Side Effects in Nursing Practice
In clinical practice, certain drug side effects pose significant risks to patients and require immediate attention. These critical reactions can lead to serious health complications, and recognizing them early is essential for effective patient care. Some side effects are rare but can be life-threatening, making it crucial for healthcare providers to understand their signs and manage them promptly.
Understanding and identifying these critical side effects can help prevent harm and improve patient outcomes. In many cases, healthcare professionals must make quick decisions to either adjust the treatment plan, discontinue the medication, or take other emergency measures to mitigate risks.
Common Critical Side Effects
| Side Effect | Description | Immediate Action |
|---|---|---|
| Respiratory Depression | Reduced breathing rate, possibly leading to hypoxia. | Administer oxygen, consider antidote or respiratory support. |
| Anaphylaxis | Severe allergic reaction, can cause swelling, breathing difficulty. | Administer epinephrine, provide emergency airway management. |
| Arrhythmias | Abnormal heart rhythms that can affect blood circulation. | Monitor vital signs, consider antiarrhythmic drugs or defibrillation. |
| Hepatotoxicity | Damage to the liver, often indicated by jaundice or elevated liver enzymes. | Discontinue the drug, monitor liver function, consider alternative treatments. |
| Severe Hypotension | Dangerously low blood pressure, which can result in shock. | Administer IV fluids, monitor blood pressure, adjust medication. |
It is essential for healthcare providers to continuously monitor for signs of these critical side effects, especially in high-risk patients. Early intervention can prevent complications and improve patient outcomes.
Antibiotics and Their Pharmacology
Antibiotics are essential medications used to treat infections caused by bacteria. These drugs work by targeting specific processes or structures in bacterial cells, leading to the destruction or inhibition of bacterial growth. Understanding the mechanism of action, proper use, and potential side effects of antibiotics is crucial for their effective application in clinical settings.
Different classes of antibiotics are designed to target different bacterial processes. Some work by interfering with cell wall synthesis, while others inhibit protein synthesis or disrupt bacterial DNA replication. The choice of antibiotic depends on the type of infection, the sensitivity of the bacteria, and the patient’s overall health condition.
Common Antibiotic Classes and Mechanisms
- Beta-lactams: These include penicillins and cephalosporins, which work by inhibiting bacterial cell wall synthesis, causing cell lysis.
- Macrolides: This class includes drugs like azithromycin, which target bacterial protein synthesis, preventing bacteria from reproducing.
- Fluoroquinolones: These antibiotics, such as ciprofloxacin, inhibit bacterial DNA replication, preventing bacteria from multiplying.
- Tetracyclines: Drugs like doxycycline interfere with protein synthesis by binding to bacterial ribosomes.
- Aminoglycosides: These medications, including gentamicin, disrupt bacterial protein synthesis, leading to bacterial death.
While antibiotics are powerful tools against bacterial infections, they must be used appropriately to avoid complications such as resistance or adverse reactions. Overuse and misuse can lead to antibiotic resistance, making infections harder to treat. It is essential for healthcare professionals to prescribe antibiotics based on accurate diagnosis and susceptibility testing to ensure their effectiveness and minimize risks.
Common Cardiovascular Drugs for Nurses
Cardiovascular drugs are essential in the management of various heart and blood vessel conditions. These medications help regulate blood pressure, heart rhythm, and fluid balance, and they can also be used to treat heart failure, arrhythmias, and prevent stroke. Understanding these medications and their mechanisms is crucial for safe administration and optimal patient outcomes.
There are several classes of cardiovascular drugs, each targeting different aspects of cardiovascular health. These medications can either relax blood vessels, regulate heart rate, or reduce fluid retention, all contributing to better heart function and circulation.
Common Classes of Cardiovascular Drugs
- Angiotensin-Converting Enzyme (ACE) Inhibitors: ACE inhibitors, such as enalapril and lisinopril, help relax blood vessels by blocking the conversion of angiotensin I to angiotensin II, leading to lowered blood pressure and reduced strain on the heart.
- Beta-Blockers: Drugs like metoprolol and atenolol are used to slow the heart rate and reduce blood pressure by blocking the effects of adrenaline, helping to prevent heart attacks and manage arrhythmias.
- Calcium Channel Blockers: Medications such as amlodipine and diltiazem work by preventing calcium from entering heart and blood vessel cells, which helps relax blood vessels and control heart rate.
- Diuretics: Drugs like furosemide and hydrochlorothiazide help reduce fluid retention by increasing urine production, which lowers blood pressure and reduces the workload on the heart.
- Antiplatelet and Anticoagulants: Aspirin and warfarin are examples of these drugs, which help prevent blood clot formation, reducing the risk of heart attacks and strokes in patients with cardiovascular conditions.
When using cardiovascular drugs, it is essential for healthcare professionals to consider each patient’s specific condition and medication interactions. Regular monitoring of blood pressure, heart rate, and kidney function is critical to ensure the effectiveness of the treatment and to detect any potential side effects early. Proper patient education regarding medication adherence and lifestyle changes is also key to achieving optimal cardiovascular health.
Pharmacology in Pain Management
Pain management is an essential aspect of healthcare, requiring the use of various medications to alleviate suffering and improve patients’ quality of life. Different types of pain–whether acute or chronic–necessitate tailored treatments, with medications playing a central role in providing relief. Understanding the different drug classes and their mechanisms of action is key to effectively managing pain while minimizing potential risks.
Medications used in pain relief can be broadly classified into several categories, each designed to target specific pain pathways or conditions. These include opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, and adjuvant medications such as antidepressants and anticonvulsants. Each class has its benefits, risks, and ideal indications, and choosing the right one depends on the type of pain and the patient’s overall health status.
Common Classes of Pain-Relief Medications
- Opioids: Medications like morphine and oxycodone are powerful pain relievers used for severe pain, often after surgery or injury. They work by binding to opioid receptors in the brain and spinal cord, reducing pain perception. However, they carry the risk of dependence and should be used with caution.
- NSAIDs: Drugs such as ibuprofen and naproxen reduce inflammation and relieve pain by inhibiting cyclooxygenase enzymes (COX-1 and COX-2). These are commonly used for mild to moderate pain caused by conditions like arthritis or muscle strain.
- Acetaminophen: This non-inflammatory pain reliever, commonly known as Tylenol, is effective for mild pain and fever but does not reduce inflammation. It is often used for headaches, dental pain, and mild arthritis.
- Antidepressants and Anticonvulsants: Certain medications like amitriptyline and gabapentin can be used for neuropathic pain. These drugs alter neurotransmitter levels in the brain, helping to manage nerve-related pain conditions such as diabetic neuropathy or fibromyalgia.
Considerations in Pain Management
While pain relief is essential, healthcare providers must carefully monitor and adjust medications to avoid adverse effects. Long-term opioid use, for example, can lead to tolerance, dependence, and potential overdose. Non-opioid medications may be more appropriate for chronic pain management, particularly in patients with a history of substance use disorder.
In addition, patient education plays a vital role in pain management. Understanding the proper use of medications, potential side effects, and when to seek further help is essential for successful treatment. A multidisciplinary approach, combining pharmacological and non-pharmacological therapies such as physical therapy or cognitive-behavioral therapy, can enhance overall pain management outcomes.
Legal and Ethical Considerations in Pharmacology

The use of medications in healthcare is not only a matter of clinical effectiveness but also involves a complex framework of legal and ethical principles. Healthcare professionals must ensure that they are adhering to legal regulations while respecting patients’ rights and providing safe and effective treatments. The balance between these responsibilities is crucial in maintaining both professional standards and patient trust.
Legal considerations in the administration of drugs include ensuring that prescribed treatments are compliant with local laws and regulations, such as those governing controlled substances. Healthcare providers must be knowledgeable about the classification of drugs, prescription requirements, and limitations on their use. Violations of these laws, whether intentional or accidental, can result in severe consequences, including legal actions, professional discipline, and loss of licensure.
On the ethical side, practitioners are required to prioritize patient autonomy and informed consent. This means that patients must be fully informed about the potential risks, benefits, and alternatives of any treatment plan. The healthcare professional’s responsibility extends to ensuring that prescriptions and drug choices align with the patient’s individual values, preferences, and clinical needs.
Furthermore, ethical principles such as non-maleficence (doing no harm) and beneficence (acting in the best interest of the patient) guide professionals in their decisions regarding medication. This is especially important when dealing with high-risk treatments, such as potent pain relievers or treatments with significant side effects. Ensuring that the benefits outweigh the risks requires a deep understanding of both the drug’s actions and the patient’s specific circumstances.
Lastly, professionals must always maintain confidentiality when dealing with patients’ medical information, including prescription details. This obligation is not only a legal requirement but also a cornerstone of trust in the patient-provider relationship. Safeguarding patient privacy ensures that individuals feel secure in their healthcare decisions and interactions.
Study Tips for Pharmacology Exams
Successfully mastering the complex material related to medication and treatment processes requires more than just basic memorization. Effective studying in this field involves understanding key concepts, recalling important information quickly, and applying knowledge to clinical scenarios. A structured study plan and active learning techniques can greatly enhance retention and understanding, ensuring you are well-prepared for assessments.
Active Learning Strategies
One of the most effective ways to prepare for tests in this area is to engage in active learning. Instead of passively reading through textbooks or notes, try methods such as:
- Practice Questions: Solve practice questions and review the correct answers. This reinforces your knowledge and helps identify areas that need more attention.
- Flashcards: Use flashcards to test your memory on drug names, mechanisms of action, and side effects. This is a great way to retain important facts.
- Group Study: Collaborate with peers to discuss challenging topics. Explaining concepts to others reinforces your own understanding.
Time Management and Consistency
Another crucial aspect of studying is time management. Break your study sessions into manageable chunks, focusing on one drug class or concept at a time. Consistency is key, so schedule daily study sessions instead of cramming all the information into one night. Create a study calendar that outlines what to review each day, ensuring you cover all necessary material before the assessment.
Additionally, prioritizing topics that are most likely to appear on tests can help you focus your efforts. Pay special attention to high-yield topics, such as drug classifications, common side effects, and interactions, as these often form the foundation of many questions.
By integrating active learning and effective time management, you’ll be better equipped to master the material and approach any challenge with confidence.