
In critical situations, knowing the right steps to take can make all the difference. Preparing for certification in emergency response requires mastering a set of procedures that ensure the well-being of those in distress. The ability to quickly assess and react appropriately is key in saving lives, particularly in instances of heart failure or breathing difficulties.
Through focused study and practice, individuals can become proficient in managing these urgent scenarios. This process involves understanding techniques such as chest compressions, airway clearance, and the use of defibrillators. A thorough grasp of these skills is essential for anyone aiming to be fully prepared for real-life emergencies.
Successful preparation involves more than memorizing facts. It’s about internalizing best practices and honing the ability to stay calm under pressure. With the right knowledge and skills, you can confidently contribute to patient recovery during critical moments.
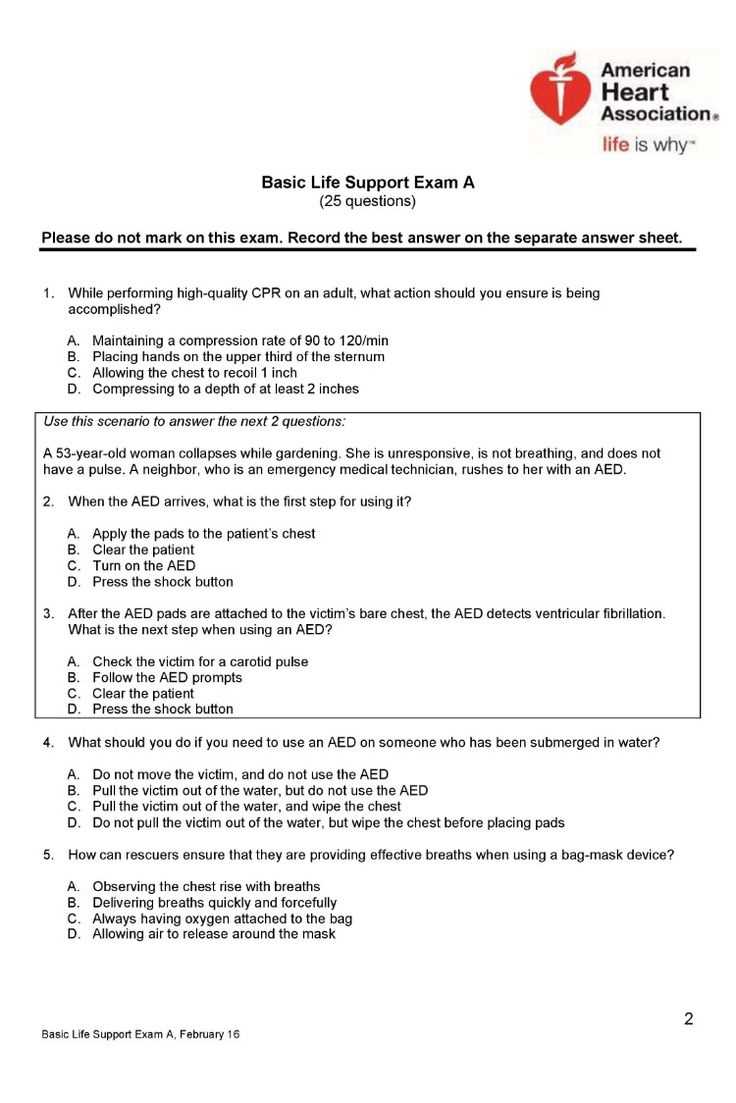
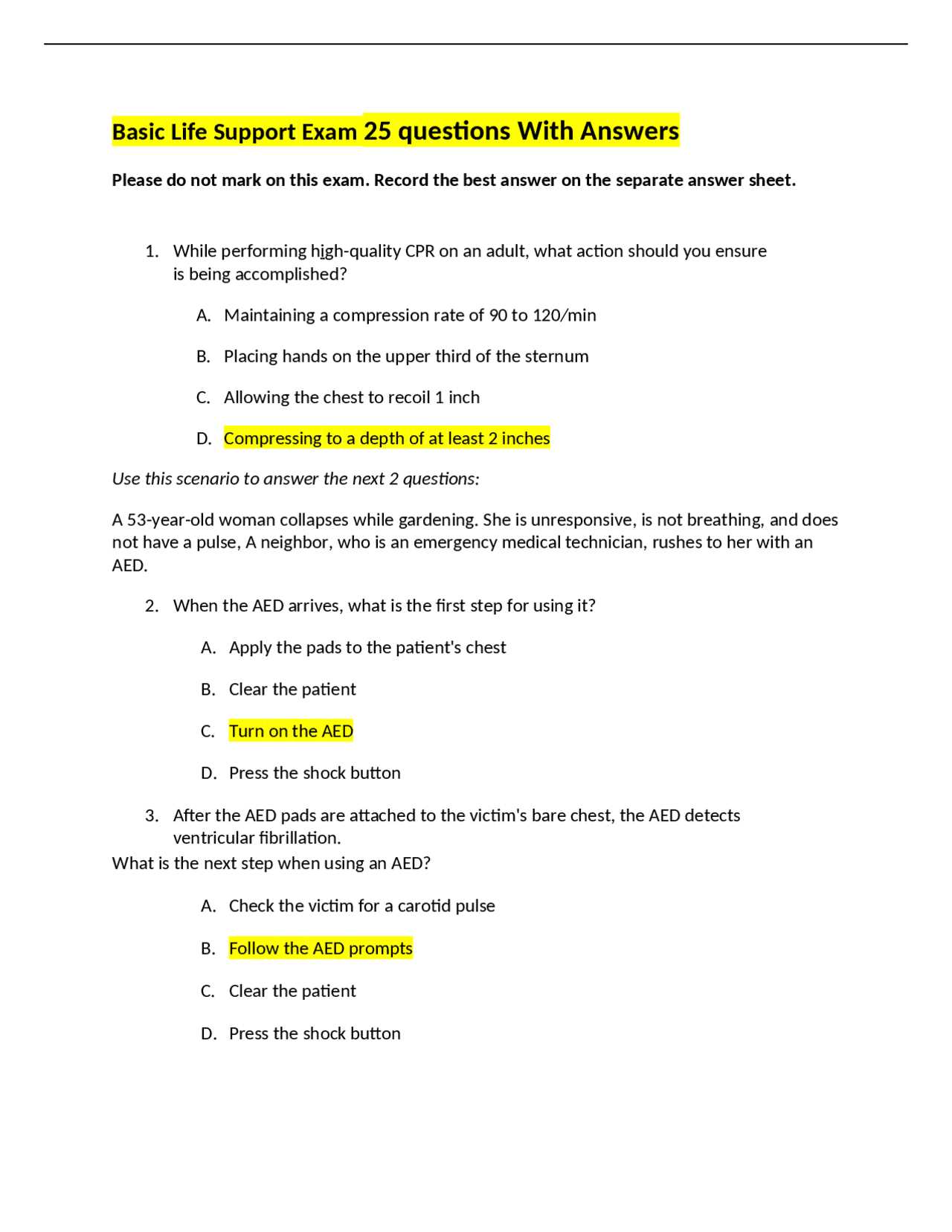
Basic Life Support Exam A Answers
In critical situations, responding swiftly and effectively can save lives. Gaining proficiency in emergency care requires not only theoretical knowledge but also practical application of key techniques. This section will guide you through essential steps and common practices tested in the certification process.
Key Procedures to Master
To be prepared for real-life emergencies, certain steps must be understood and practiced thoroughly. These are the foundational skills tested in the certification assessments:
- Chest Compressions: Proper technique for maintaining circulation when the heart stops beating.
- Airway Management: Ensuring an open airway for optimal breathing.
- Defibrillator Use: Effectively applying electrical shocks to restart the heart.
- Rescue Breathing: Providing breaths when a person is not breathing on their own.
Common Mistakes to Avoid
While preparing for certification, it’s important to be aware of the common errors people make. Understanding these pitfalls can help improve performance and increase success rates.
- Not administering chest compressions at the correct depth or rate.
- Failure to clear the airway properly before performing rescue breaths.
- Incorrect placement of defibrillator pads.
- Delaying the start of CPR due to hesitation or lack of confidence.
By practicing these essential skills and avoiding common mistakes, you will be well on your way to passing the assessment and becoming equipped to handle emergency situations effectively. The knowledge gained will serve you not only during testing but also in real-world situations where your actions can make a life-saving difference.
Key Concepts in Basic Life Support
When responding to emergencies, certain fundamental practices form the backbone of effective care. These concepts are vital to ensuring that patients receive timely and appropriate assistance, particularly in situations where the heart stops or breathing ceases. Mastering these techniques is essential for anyone involved in emergency response.
Understanding the following concepts is crucial for providing quick, efficient care:
- Chest Compressions: A core technique used to maintain blood flow to vital organs when the heart stops.
- Airway Management: Ensuring that the airway is open so that the patient can breathe effectively.
- Defibrillation: The application of an electric shock to the heart to restore normal rhythm in cases of cardiac arrest.
- Rescue Breathing: Delivering breaths manually when the patient is unable to breathe on their own.
- Circulation Assessment: Evaluating pulse and blood flow to ensure proper circulation.
These elements are interconnected, and a comprehensive understanding of each is essential for providing optimal care in urgent situations. Practicing these techniques consistently helps build confidence and ensures readiness in high-pressure moments.
In addition to these core actions, staying calm and following a systematic approach is key to reducing the risk of complications. The ability to assess the situation quickly, take the necessary steps, and continue providing care until further help arrives can significantly impact the outcome for the patient.
Understanding CPR Procedures for BLS
When an individual experiences cardiac arrest or stops breathing, prompt intervention is critical to restoring vital functions. Cardiopulmonary resuscitation (CPR) is a life-saving technique that involves a combination of chest compressions and artificial ventilation. The primary goal of CPR is to maintain blood flow to the brain and other vital organs until professional medical help can arrive.
Effective CPR requires understanding the correct procedures and performing them consistently. The following steps outline the essential components of CPR:
- Chest Compressions: Begin by performing deep, rhythmic compressions at the center of the chest. The compressions should be about 2 inches deep, at a rate of 100-120 compressions per minute.
- Airway Clearance: After ensuring the chest is compressed properly, clear the airway by tilting the head back and lifting the chin to open the airway. This ensures that breaths can be delivered effectively.
- Rescue Breaths: Administer two rescue breaths following every 30 compressions. Pinch the nose, create a tight seal over the mouth, and give one breath lasting about 1 second, ensuring the chest rises.
- Defibrillation (if available): If an automated external defibrillator (AED) is present, use it as soon as possible. The device will guide you through the necessary steps to administer a shock if required.
Timing is critical when performing CPR. In situations where a defibrillator is unavailable, continuous chest compressions are essential to maintain circulation. Practice is key to mastering CPR procedures, as proper technique can make a significant difference in patient outcomes.
Common Mistakes in Life Support Exams
In high-pressure situations, it’s easy to make errors that can impact the outcome of an emergency. When preparing for certification or practical tests, knowing what mistakes to avoid is just as important as mastering the correct techniques. Common errors often arise from a lack of understanding or practice, and these can be critical in real-life situations.
Here are some frequent mistakes made during assessments that can hinder performance:
- Incorrect Compression Depth: Failing to compress the chest deep enough can reduce blood circulation, making the procedure ineffective. It is essential to apply enough pressure (about 2 inches) during compressions.
- Inconsistent Compression Rate: Compressions should be administered at a consistent rate of 100-120 per minute. A slower or faster pace can reduce the chances of a positive outcome.
- Not Clearing the Airway Properly: Inadequately opening the airway can prevent proper ventilation. Ensure the head is tilted back, and the chin is lifted to clear the airway.
- Delayed Defibrillation: In cases where an automated external defibrillator (AED) is available, waiting too long to use it can lower survival chances. Immediate use is critical to restoring normal heart rhythm.
- Incorrect Placement of AED Pads: Improper pad placement can result in ineffective defibrillation. Be sure to follow the diagram on the pads or device to place them correctly on the chest.
Awareness of these common pitfalls allows individuals to focus on improvement and ensure that they are prepared to perform optimally during real-world emergencies. Consistent practice and a strong understanding of the procedures are essential for success in any evaluation or real-life scenario.
Essential Techniques for Chest Compressions
Chest compressions are a critical component of emergency care, especially in cases of cardiac arrest. Proper technique ensures that blood continues to flow to vital organs, such as the brain, while medical help is on the way. Mastering the correct method is essential for improving survival chances and optimizing patient outcomes.
The key to effective chest compressions lies in the following essential elements:
- Hand Placement: Position the heel of one hand on the center of the chest, just below the breastbone. Place the other hand on top, interlocking your fingers. This provides the stability and strength needed for compressions.
- Compression Depth: Press down firmly to a depth of about 2 inches (5 cm) for adults. Compressions that are too shallow will not be effective in circulating blood to the heart and brain.
- Compression Rate: Perform compressions at a steady rate of 100-120 per minute. This rhythm is crucial for maintaining adequate blood flow during resuscitation efforts.
- Allow Full Recoil: After each compression, allow the chest to return to its normal position before starting the next compression. Full recoil helps maintain proper circulation between compressions.
- Body Position: Keep your arms straight and shoulders directly over your hands. This will help you use your body weight effectively and minimize fatigue during continuous compressions.
Proper training and regular practice are necessary to ensure that chest compressions are performed efficiently. In an emergency, every second counts, and being able to apply the correct technique without hesitation is vital for the patient’s survival.
Airway Management in Life Support Tests
Effective airway management is a fundamental aspect of emergency care. In critical situations, ensuring that the airway remains clear is vital for the patient’s ability to breathe. In any assessment or real-world emergency, being able to recognize and correct airway obstructions is essential for providing proper care.
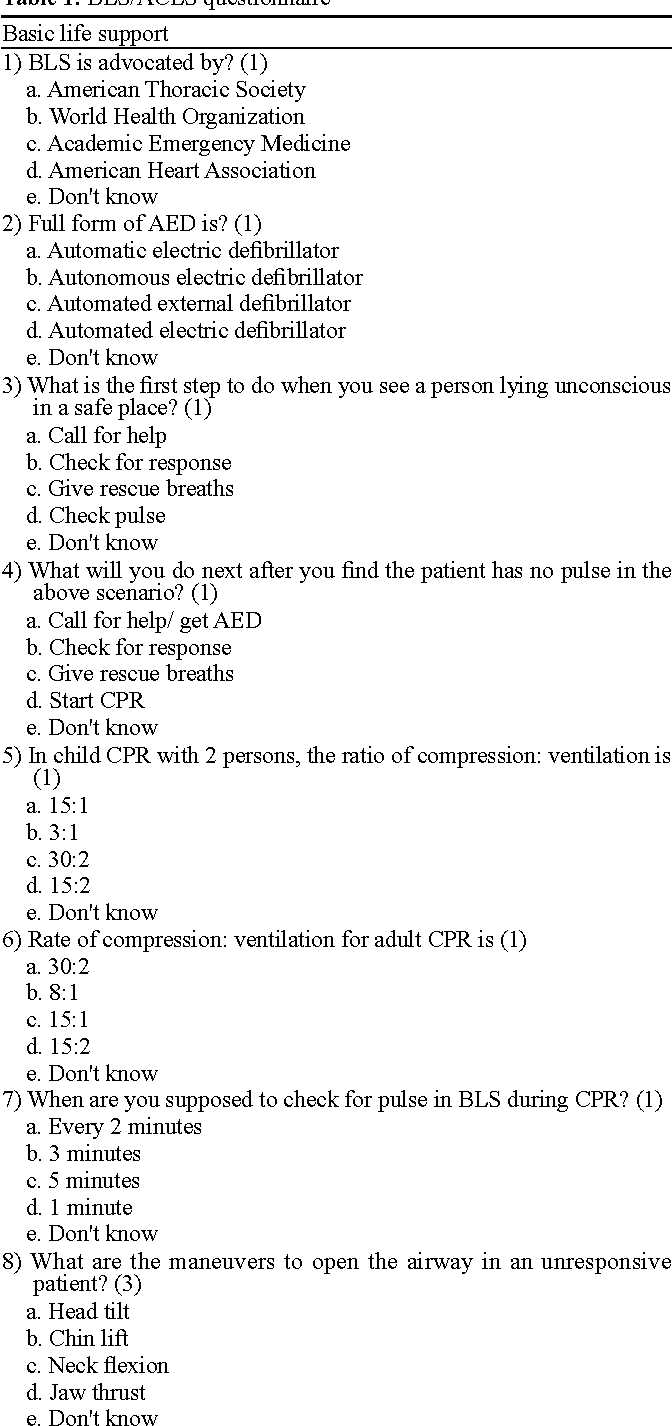
The following methods are commonly tested to ensure effective airway management:
| Technique | Description | Purpose |
|---|---|---|
| Head-Tilt, Chin-Lift | Used to open the airway by tilting the head back and lifting the chin. This is the standard method for most patients unless there is a suspected neck injury. | To clear the airway and allow air to enter the lungs. |
| Jaw-Thrust | Performed by placing your hands on both sides of the patient’s jaw and lifting it upward, without tilting the head. This method is used when spinal injury is suspected. | To open the airway while minimizing movement of the spine. |
| Oropharyngeal Airway (OPA) | A curved device inserted into the mouth to keep the tongue from blocking the airway. | To ensure a clear airway in unconscious patients with no gag reflex. |
| Nasopharyngeal Airway (NPA) | A flexible tube inserted through the nose to maintain airway patency in conscious or semi-conscious patients. | To clear the airway without stimulating the gag reflex. |
Proper technique and the ability to recognize when each method is necessary can significantly impact the patient’s ability to breathe and survive. Regular practice and understanding of these procedures are essential for ensuring quick and effective airway management during emergencies.
Role of Defibrillators in CPR
In cases of cardiac arrest, when the heart’s rhythm becomes erratic or stops altogether, a defibrillator can be a life-saving device. It is designed to restore the heart’s normal rhythm by delivering an electric shock to the chest. This process is known as defibrillation and is a crucial step in improving survival rates when combined with chest compressions and rescue breathing.
Defibrillators work by analyzing the heart’s electrical activity and determining whether a shock is necessary. If the device detects a shockable rhythm, it will instruct the user to deliver a shock. Timely defibrillation, especially within the first few minutes of arrest, can significantly increase the chances of survival. The role of defibrillators is vital in CPR protocols, particularly in situations involving ventricular fibrillation or pulseless ventricular tachycardia.
- Automated External Defibrillators (AEDs): These portable devices are often found in public spaces, making them accessible for bystanders to use in an emergency. They provide step-by-step voice instructions and analyze the heart’s rhythm automatically.
- Manual Defibrillators: Typically used by healthcare professionals, these devices allow the user to adjust settings based on the patient’s condition and provide a more tailored approach to defibrillation.
Using a defibrillator correctly and swiftly during CPR can drastically improve the outcomes for patients in cardiac arrest. However, it is essential for responders to understand when and how to use the device effectively. Training and practice are key to ensuring that the device is used correctly in critical situations.
Importance of Timing in Life Support
In emergency care, every second counts. The speed and precision with which interventions are administered can significantly impact the patient’s chances of survival. From the onset of a medical emergency to the delivery of key procedures, effective timing can be the difference between life and death. Quick action, coupled with accurate techniques, ensures that vital functions are restored promptly and efficiently.
The timing of various steps in an emergency care protocol is critical, particularly in situations involving cardiac arrest or respiratory failure. Delays in performing key procedures can result in severe consequences for the patient. Understanding the role of timing and the urgency required during specific interventions is essential for anyone involved in emergency response.
| Action | Recommended Time Frame | Consequences of Delay |
|---|---|---|
| Chest Compressions | Immediately upon recognizing cardiac arrest | Delay reduces blood flow to vital organs, especially the brain, increasing the risk of brain damage. |
| Defibrillation | Within the first 3-5 minutes | Delayed defibrillation can lower the chances of survival by up to 70%. The heart may not respond to a shock if too much time passes. |
| Rescue Breaths | Immediately after confirming airway clearance | Failure to provide oxygen can lead to hypoxia, causing irreversible damage to the brain and other organs. |
Being aware of the timing requirements for each action is fundamental to delivering optimal care in emergency situations. Delaying any step can lead to worse outcomes, making it vital for responders to act quickly and decisively to maximize the chances of survival and recovery.
Recognizing Cardiac Arrest Symptoms
Prompt recognition of cardiac arrest is crucial for effective intervention. Identifying the signs early can drastically improve the chances of survival. In an emergency situation, every second counts, and knowing what to look for allows responders to take immediate action. Recognizing the symptoms of a heart attack or sudden collapse can lead to faster implementation of life-saving procedures.
Common signs of cardiac arrest include:
- Sudden Collapse: A person may suddenly fall to the ground without warning. This is often due to the heart failing to pump blood effectively.
- Unresponsiveness: The individual may be unresponsive to verbal or physical stimuli, indicating that blood is not reaching the brain.
- No Breathing or Abnormal Breathing: The person may stop breathing altogether or exhibit irregular, gasping breaths known as agonal breathing.
- No Pulse: There may be no detectable pulse, which indicates that the heart is not pumping blood through the body.
If any of these signs are present, it is essential to act quickly. Start by calling for emergency help and begin CPR if necessary. Early intervention with chest compressions, defibrillation, and rescue breaths can significantly increase the likelihood of recovery.
Using the AED Effectively
An Automated External Defibrillator (AED) is a critical tool in the emergency response to cardiac arrest. It is designed to analyze the heart’s rhythm and, if necessary, deliver a shock to restore a normal heartbeat. The device is simple to use, even for those with minimal medical training, but understanding how to operate it efficiently can make a significant difference in saving a life.
To use the AED effectively, follow these steps:
- Turn on the Device: Press the power button to activate the AED. The device will begin giving verbal instructions for each step.
- Attach the Pads: Place the adhesive electrode pads on the person’s bare chest as instructed. One pad should be placed on the upper right side of the chest, and the other on the lower left side, below the rib cage.
- Analyze the Heart Rhythm: Allow the AED to analyze the heart’s rhythm. Do not touch the patient while this is happening. The AED will tell you if a shock is needed.
- Deliver the Shock: If the AED recommends a shock, ensure no one is touching the person and press the shock button. Follow any further instructions provided by the device.
- Continue CPR: After the shock is delivered, resume chest compressions immediately and continue until emergency personnel arrive or the patient shows signs of life.
It is essential to remain calm and follow the AED’s instructions closely. These devices are designed to guide users through each step, making them an invaluable tool in critical situations. Early defibrillation, when combined with high-quality CPR, significantly increases the chances of survival following cardiac arrest.
Assessing Breathing and Circulation
When responding to an emergency, the first step in providing effective care is assessing whether the person is breathing and if their circulation is functioning properly. Recognizing any changes in these vital signs can help determine the urgency and type of intervention needed. Accurate and quick evaluation is key to initiating the appropriate steps and ensuring the best possible outcome for the individual.
To assess breathing and circulation, follow these key steps:
- Check for Breathing: Look, listen, and feel for signs of normal breathing. Position your ear near the person’s mouth and nose, and observe their chest for any rise and fall. Agonal breathing (irregular, gasping breaths) is not normal and should be treated as if the person is not breathing.
- Look for Signs of Circulation: Check for a pulse by feeling for it at the carotid artery (on the neck) or the radial artery (at the wrist). If there is no pulse or if it is weak or irregular, immediate intervention is required.
- Time Sensitivity: If the person is not breathing or their circulation is compromised, time is critical. Begin resuscitation efforts immediately, starting with chest compressions and, if necessary, rescue breaths. Early intervention significantly improves survival chances.
In situations where both breathing and circulation are absent, the most effective response is to begin CPR right away and call for emergency help. Every moment counts, and fast action can make all the difference in saving a life.
Handling Unresponsive Patients Safely
When faced with an unresponsive individual, it is crucial to handle the situation with care to avoid further harm and ensure that timely medical help is provided. Proper technique in assessing and managing an unresponsive person is vital for both their immediate safety and for improving the chances of recovery. The actions you take in the first moments can significantly affect their outcome.
Key Considerations for Safe Handling
Before providing any treatment, it’s important to ensure that the area is safe for both you and the patient. Check for any immediate dangers and make sure the person is not at risk of further injury. Follow these steps for handling an unresponsive patient:
- Assess Responsiveness: Gently tap or shake the person’s shoulders and shout to see if they respond. If they do not react, assume they are unresponsive.
- Ensure Safety: Make sure the environment is safe for both the patient and yourself. Move the individual away from any hazards, if possible.
- Positioning: If the person is unresponsive but breathing, place them in the recovery position. This will help keep the airway open and reduce the risk of choking.
- Call for Help: Call emergency services immediately. Time is critical in such situations, so prompt assistance is essential.
What to Do Next
If the person is not breathing or does not have a pulse, begin CPR right away. Follow the appropriate steps for chest compressions and rescue breaths while awaiting professional help. Always continue performing CPR until emergency personnel arrive or the person begins to show signs of life.
Taking prompt and appropriate action when dealing with an unresponsive individual can be the difference between life and death. Act quickly, but always ensure that the actions you take are done safely to prevent further injury.
CPR for Children and Infants
When providing resuscitation to children and infants, it is essential to adjust techniques to their smaller size and unique physiological needs. The approach differs significantly from that used for adults due to the differences in anatomy, heart rate, and lung capacity. Understanding these differences is critical to ensuring effective intervention and improving the chances of survival.
Key Differences in CPR for Children and Infants
CPR for children and infants requires a modified approach in terms of compression depth, airway management, and the number of rescue breaths. Below are some key differences:
| Age Group | Compression Depth | Compression-to-Breath Ratio | Airway Position |
|---|---|---|---|
| Infants (under 1 year) | About 1.5 inches (4 cm) | 30:2 for one rescuer, 15:2 for two rescuers | Neutral or slightly extended |
| Children (1 year to puberty) | About 2 inches (5 cm) | 30:2 for one rescuer, 15:2 for two rescuers | Neutral |
Steps for Performing CPR on Children and Infants
Follow these steps to perform CPR effectively on children and infants:
- Assess Responsiveness: Gently tap the child or infant and shout to see if they respond. If they do not respond, proceed with CPR.
- Call for Help: If you are alone with the child or infant, perform CPR for about 2 minutes before calling emergency services. If someone is with you, have them call for help immediately.
- Chest Compressions: For infants, use two fingers placed just below the nipple line to compress the chest. For children, use the heel of one hand or two hands depending on the size of the child.
- Rescue Breaths: For both infants and children, ensure the airway is open and deliver gentle breaths. For infants, cover both the nose and mouth with your mouth. For children, use the same technique as for adults, covering only the mouth.
It is important to continuously monitor the child or infant while performing CPR, ensuring that chest compressions are deep enough and that breaths are given gently. As with adult CPR, it is essential to act quickly and stay calm to maximize the chances of survival.
Legal and Ethical Considerations in BLS
When providing emergency care, it is essential to understand the legal and ethical boundaries that guide actions in critical situations. Responders must act in ways that protect both themselves and the person in need of assistance, ensuring that their interventions are lawful and respectful of individual rights. Knowledge of these principles can prevent legal issues and uphold ethical standards, making a significant difference in the outcome of a medical emergency.
One of the main concerns is consent, as responders must be aware of the importance of obtaining approval to treat a patient, especially when the individual is conscious. In situations where the person is unresponsive or unable to communicate, responders are typically permitted to act in the best interest of the individual. Understanding these protocols helps responders make decisions that align with legal requirements and ethical obligations.
Consent and Legal Protection
Consent plays a crucial role in the delivery of emergency care. There are two primary forms of consent:
- Implied Consent: This occurs when a person is unconscious or unable to give explicit consent. It is assumed that the person would want life-saving assistance in such cases.
- Expressed Consent: This involves a conscious individual who agrees to receive care after being informed of the procedure and its potential risks.
In many regions, Good Samaritan laws protect responders from legal liability when they act in good faith to help someone in a life-threatening situation. These laws typically shield individuals from lawsuits as long as they do not act recklessly or exceed their training.
Ethical Responsibilities
In addition to legal considerations, responders must adhere to several ethical principles when providing emergency care. These include:
- Beneficence: The principle of doing good for the patient by taking actions that provide the greatest benefit and improve outcomes.
- Non-maleficence: Ensuring that no harm is done to the person during care. This means avoiding any actions that could worsen the person’s condition.
- Autonomy: Respecting the individual’s right to make decisions about their own care, including the right to refuse treatment, as long as they are capable of making an informed choice.
By following these ethical guidelines, responders can ensure that their actions are both morally responsible and legally sound, fostering a sense of trust and safety for the individual receiving care. Clear understanding of both ethical and legal aspects of care delivery is essential for anyone involved in emergency response and helps to create a safe, respectful environment for both the patient and the responder.
Reviewing BLS Exam Scenarios
In any emergency response situation, the ability to quickly assess and act is crucial. By practicing different scenarios, responders can better prepare themselves for the unpredictable nature of real-life events. Reviewing various case studies and test scenarios is an effective method to sharpen skills and decision-making under pressure. This process helps ensure that responders are ready to take the right actions when lives are on the line.
Common Scenario 1: Unresponsive Adult
One of the most common situations encountered involves an adult who is unresponsive and not breathing. In this scenario, the responder’s first step is to ensure the environment is safe before approaching the patient. After confirming the person is unresponsive, the responder should check for breathing and circulation. If the individual is not breathing or is only gasping, chest compressions and rescue breathing should begin immediately. It’s important to follow a structured sequence of actions to ensure the best possible outcome.
- Step 1: Ensure safety of the scene.
- Step 2: Check for responsiveness and breathing.
- Step 3: Begin chest compressions and rescue breaths if necessary.
- Step 4: Continue until professional help arrives or the patient shows signs of life.
Common Scenario 2: Child or Infant in Distress
When responding to a child or infant in distress, the procedures are adjusted to account for the smaller size and delicate nature of young patients. In this case, chest compressions should be performed with one hand or two fingers for infants, and the rescue breaths should be delivered gently. These slight changes in technique are essential to prevent causing harm while still effectively providing life-saving care. Review of these altered techniques is vital during training.
- Step 1: Check for responsiveness.
- Step 2: Assess breathing and start rescue breaths if necessary.
- Step 3: Administer chest compressions appropriate for age and size.
- Step 4: Continue care and seek advanced medical support.
By understanding and reviewing these common scenarios, responders can enhance their readiness to act swiftly and confidently. Familiarity with a range of situations helps ensure that emergency care is effective, efficient, and appropriate for the individual’s age and condition. Continual practice in simulated situations prepares responders for real-life emergencies, where time and accuracy are critical to saving lives.
Preparing for the Essential Responder Test
Preparing for any emergency care assessment requires focused practice and a clear understanding of key procedures. Success in these tests depends on the ability to respond confidently and efficiently in high-pressure situations. To achieve this, candidates must familiarize themselves with fundamental techniques, protocols, and theoretical knowledge that underpin immediate medical interventions. Effective preparation combines practical exercises with theoretical review, ensuring readiness for real-world emergencies.
Key Areas to Focus On
To excel in the test, candidates should concentrate on the following critical areas:
- Chest Compressions: Mastering the technique for delivering high-quality chest compressions is essential. Proper hand placement, depth, and rate are crucial for effective circulation during cardiac arrest.
- Airway Management: Understanding how to clear the airway and use devices such as the bag-valve mask correctly is vital for effective ventilation.
- Breathing Assessment: Practicing the ability to quickly assess whether the patient is breathing and to provide rescue breaths if necessary.
- Defibrillator Use: Familiarizing yourself with automated external defibrillators (AEDs) and understanding when and how to use them appropriately.
Practical Training Tips
While theoretical knowledge is important, hands-on practice is the key to mastering emergency care skills. Here are some practical tips to help with preparation:
- Attend Training Sessions: Participate in certified courses that include both theory and practical skills assessments.
- Practice with Manikins: Regularly practice techniques like chest compressions, rescue breaths, and defibrillator use on training manikins.
- Simulate Real-Life Scenarios: Engage in simulated emergency situations to develop your decision-making and reaction times under stress.
- Review Protocols: Revisit the guidelines and best practices, ensuring familiarity with the most current protocols.
Effective preparation is about mastering the skills necessary to save lives and building the confidence to apply them in any situation. By focusing on practical techniques, understanding theoretical principles, and simulating real-world scenarios, you will be ready for the assessment and equipped to respond in emergencies.
Test-Taking Strategies for Responder Assessments
Achieving success in any responder certification requires more than just mastering techniques; it also involves a strategic approach to taking the assessment. Knowing how to navigate the test efficiently and stay focused under pressure can make a significant difference. Developing a methodical approach allows you to manage your time, make informed decisions, and avoid common pitfalls that may arise during the assessment process.
Effective Preparation for Success
Before even stepping into the test, thorough preparation is key. Here are a few strategies that can help:
- Review Key Concepts: Familiarize yourself with core principles such as chest compressions, airway management, and defibrillation. Understanding the foundational elements will help you apply your knowledge confidently during the test.
- Simulate Test Scenarios: Practice under timed conditions to mimic the actual assessment. This helps you get comfortable with answering questions quickly and managing your time effectively.
- Focus on High-Yield Topics: Prioritize areas that are frequently tested, such as CPR procedures, emergency response protocols, and use of medical equipment like AEDs.
- Test Your Knowledge Regularly: Regularly quiz yourself on key concepts and techniques to solidify your understanding and ensure retention.
Test-Day Tips for Success
On the day of the test, the following strategies will help you maintain focus and perform at your best:
- Stay Calm and Focused: Stress can hinder performance. Practice relaxation techniques such as deep breathing to keep your mind clear and focused during the test.
- Read Questions Carefully: Always read each question thoroughly before answering. Pay attention to key words and instructions to avoid making unnecessary mistakes.
- Manage Your Time: Allocate time wisely for each section. If a question seems particularly difficult, move on and come back to it later if needed.
- Eliminate Incorrect Options: If unsure of an answer, try eliminating clearly incorrect options first. This increases your chances of selecting the correct one.
With effective preparation and the right test-taking strategies, you will be better equipped to handle the challenges of any responder assessment and demonstrate your ability to act effectively in emergency situations.