
In this section, we delve into the essential topics that form the foundation of studying microorganisms and their behaviors. By grasping these core principles, students can build a stronger understanding of how microbes interact with their environment, evolve, and affect both health and industry.
Knowledge of microbial processes is crucial for comprehending the intricate relationships between various types of organisms. From growth patterns to their responses to external stimuli, the ability to analyze these factors plays a key role in advancing scientific research and medical practices.
Additionally, a solid grasp of laboratory techniques and diagnostic methods enhances practical skills, making it easier to identify and study microorganisms. The practical application of these concepts is indispensable for anyone pursuing a career in biological sciences or healthcare.
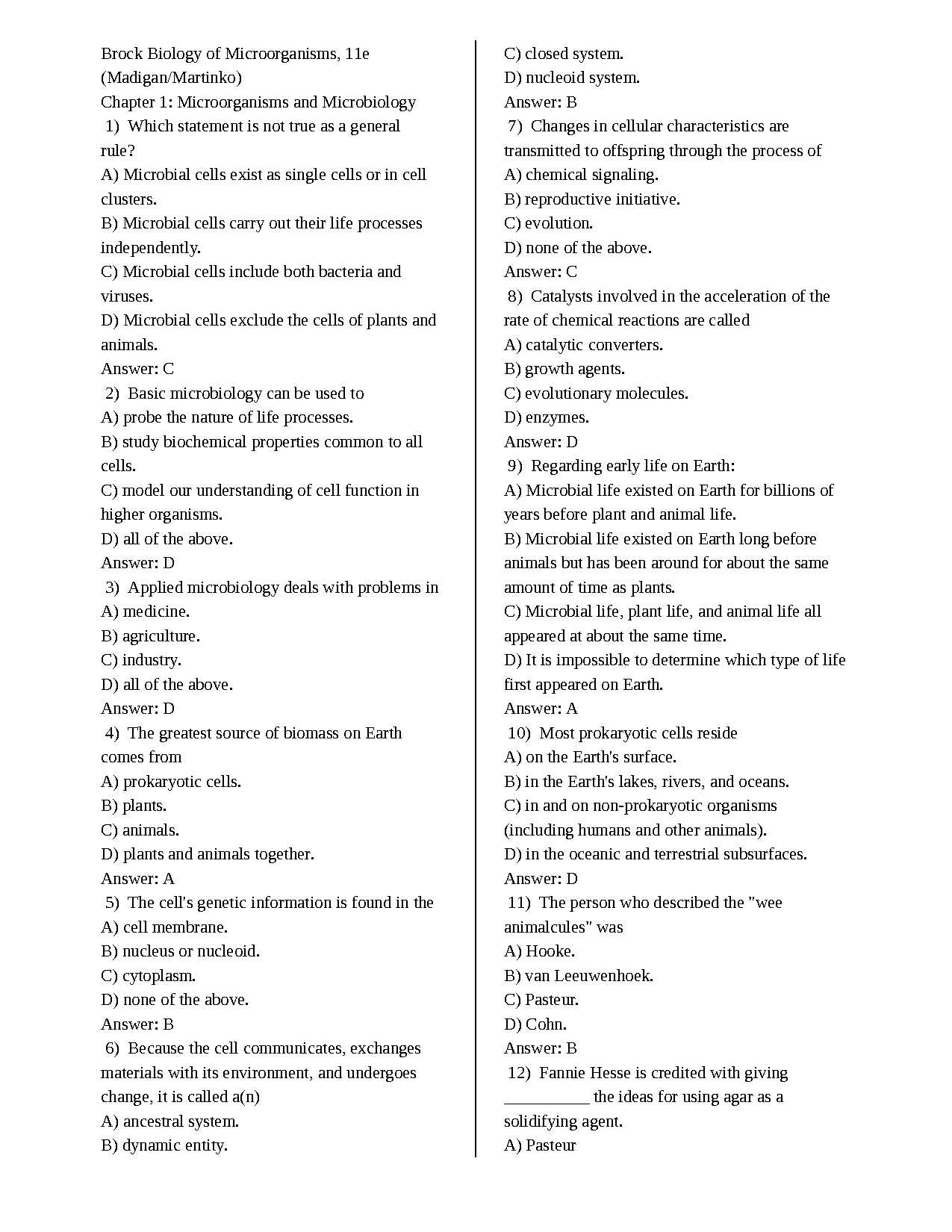
Microbiology Chapter 5 Test Answers
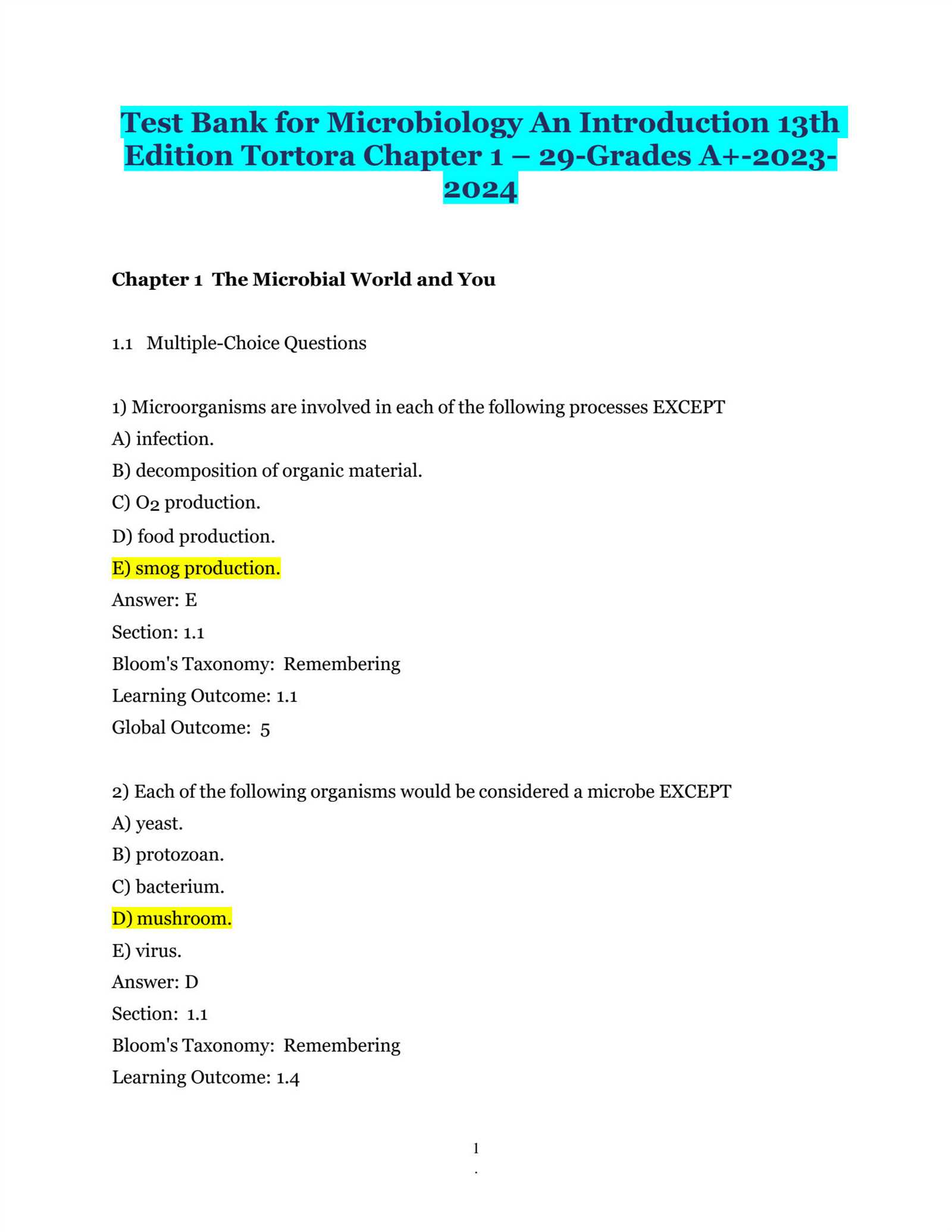
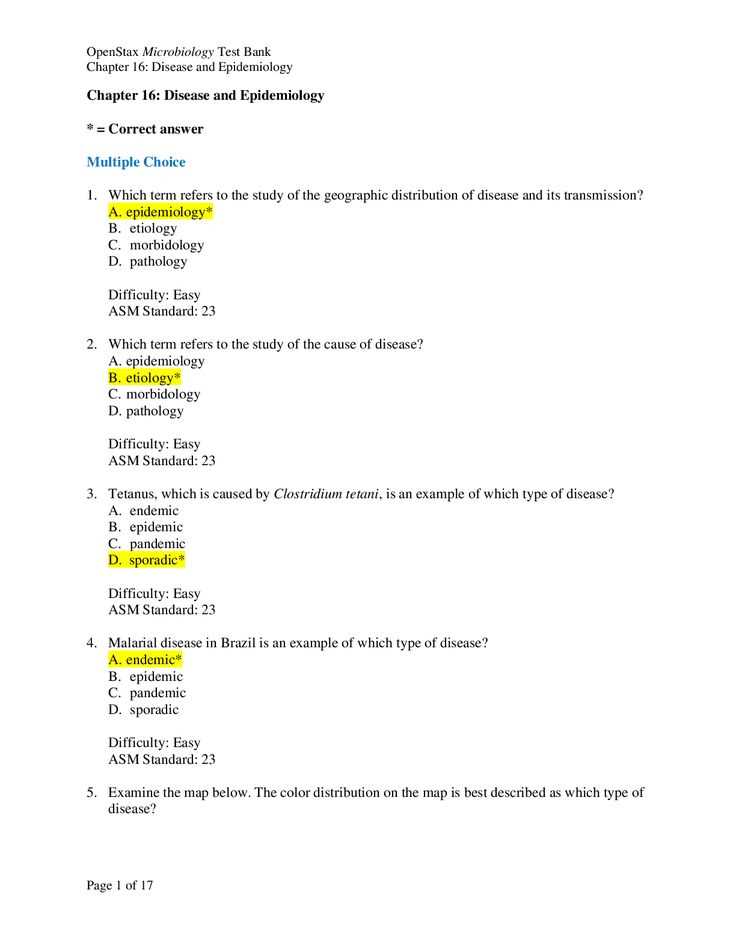
In this section, we will review the key concepts and questions that are often included in assessments on the study of microorganisms. Understanding the underlying principles and being able to apply them in various scenarios is essential for mastering the subject and performing well on exams.
Familiarity with key terminology and processes is vital for solving common problems that arise in this field. By focusing on the core topics, you can improve your ability to correctly interpret and answer related questions, ensuring a more thorough understanding of microbial behaviors and interactions.
Additionally, a review of practical applications and experimental results will further reinforce the theoretical knowledge needed to excel. Whether it’s identifying various microbial structures or understanding the environmental factors that influence growth, this section provides a comprehensive overview of what you need to know.
Key Concepts of Chapter 5
This section covers fundamental principles that are essential for understanding the behavior and characteristics of microorganisms. Grasping these core ideas will provide the foundation necessary to answer questions and solve problems related to microbial processes and interactions.
Understanding microbial classification is crucial for distinguishing between different types of organisms. Whether examining bacteria, viruses, or fungi, knowing their structural and functional differences is key to further study.
Growth and reproduction patterns play a central role in the survival of microorganisms. These processes are influenced by environmental factors, and being able to analyze them helps predict how microbes behave in different conditions.
Finally, the mechanisms of microbial resistance and their impact on human health and medicine are of significant importance. Understanding how pathogens evolve resistance to treatments is vital for developing effective strategies in disease prevention and management.
Understanding Microbial Classification
Classifying microorganisms is an essential step in understanding their diversity, structure, and function. By grouping organisms based on shared characteristics, scientists can better study their behaviors, interactions, and roles in the environment or human health.
Categories of Microorganisms
The classification system typically divides organisms into several broad categories. These groups help in identifying key features such as shape, size, genetic makeup, and metabolic processes. Some of the primary categories include:
- Bacteria: Single-celled organisms that can be found in nearly every environment.
- Viruses: Infectious agents that require a host cell to replicate.
- Fungi: Eukaryotic organisms that include yeasts, molds, and mushrooms.
- Protozoa: Single-celled organisms with complex structures.
- Algae: Photosynthetic organisms found in water and soil.
Key Classification Criteria
To distinguish between different types of microorganisms, scientists use a variety of criteria:
- Cell Structure: Whether the organism is prokaryotic (lacking a nucleus) or eukaryotic (with a nucleus).
- Genetic Information: The sequencing of DNA helps determine relationships and evolutionary history.
- Metabolic Pathways: Differences in how organisms obtain and process energy can reveal much about their classification.
- Reproduction Methods: Microorganisms can reproduce sexually or asexually, a key factor in classification.
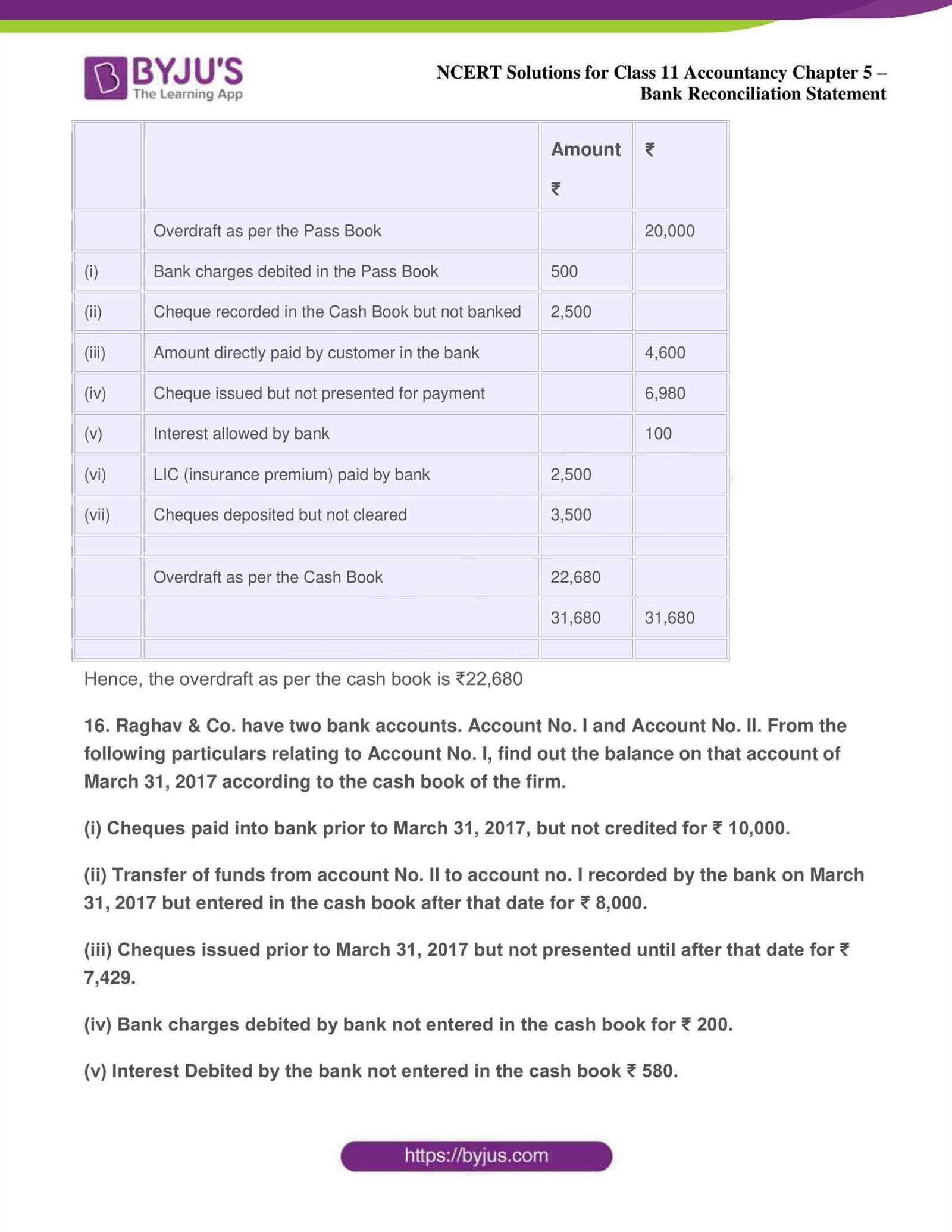
Overview of Microbial Growth Factors
The growth and reproduction of microorganisms are influenced by a variety of environmental and internal factors. These elements determine how effectively microbes can multiply and thrive under different conditions. Understanding these factors is key to controlling microbial populations in both natural and clinical settings.
Essential Environmental Factors
Microbes require specific environmental conditions to grow optimally. The availability of nutrients, temperature, pH, and oxygen levels all play a crucial role in microbial proliferation. These factors vary depending on the type of microorganism and its preferred habitat.
| Factor | Impact on Growth |
|---|---|
| Temperature | Most microbes have an optimal temperature range where growth is most rapid. Extremes in temperature can inhibit or kill microbial cells. |
| pH | Microbial enzymes work best within a specific pH range. Too acidic or too alkaline conditions can limit growth or disrupt cellular functions. |
| Oxygen | Some microbes require oxygen (aerobic), while others can grow without it (anaerobic). Some can adapt to both environments (facultative anaerobes). |
| Nutrients | The availability of carbon, nitrogen, sulfur, and other minerals is essential for cellular growth, energy production, and replication. |
Internal Factors Influencing Growth
Aside from external environmental factors, internal conditions such as genetic makeup and metabolic processes also determine how well a microbe can grow and reproduce. Adaptations to external stressors, as well as the presence of specific enzymes and molecules, further contribute to the microorganism’s ability to thrive.
Types of Bacterial Reproduction
Bacterial organisms reproduce in various ways to ensure the continuation of their species. The mechanisms through which they multiply are crucial for understanding their behavior, spread, and the development of resistance to treatments. These processes can vary significantly depending on the type of bacteria and environmental conditions.
The most common form of bacterial reproduction is binary fission, where a single bacterium divides into two genetically identical offspring. This asexual process allows for rapid population growth under favorable conditions.
Another method of reproduction is budding, where a new organism grows out of the parent organism, eventually detaching and forming an independent bacterium. Although less common, this process can be observed in certain species of bacteria.
In addition to these, some bacteria can exchange genetic material through conjugation, a process that involves the transfer of DNA between two bacterial cells, enhancing genetic diversity and sometimes leading to the acquisition of beneficial traits like antibiotic resistance.
Examining Microscopic Techniques
The ability to observe microorganisms requires specialized techniques to enhance their visibility and detail. Since most microbes are too small to be seen with the naked eye, using advanced optical tools is essential for studying their structure, behavior, and interactions. These techniques allow scientists to uncover the complexities of microbial life and make precise observations in research and clinical settings.
Types of Microscopic Methods
Various microscopic methods are employed to examine microorganisms, each offering unique advantages depending on the specific research objectives. Some of the most commonly used techniques include:
- Brightfield Microscopy: A standard method where light passes through the specimen, allowing for clear images of stained microorganisms.
- Phase Contrast Microscopy: Enhances contrast in transparent specimens, allowing detailed observation of live cells without staining.
- Electron Microscopy: Uses electron beams instead of light to reveal detailed structures at the molecular level, ideal for observing viruses and fine cellular components.
Staining Techniques for Clarity
Staining is a critical technique in microscopy that helps distinguish different types of microorganisms and structures within them. By applying specific dyes, scientists can highlight features like cell walls, nuclei, or internal organelles, improving clarity and contrast for observation. Common staining methods include:
- Gram Staining: Differentiates bacteria based on their cell wall composition, classifying them as Gram-positive or Gram-negative.
- Acid-Fast Staining: Used primarily to identify certain bacterial species, such as Mycobacterium, which resist conventional staining methods.
Importance of Gram Staining

Gram staining is a critical technique in the study of bacteria, used to differentiate between types of microbial cells based on their cell wall composition. This simple yet powerful method provides valuable insights into bacterial classification and plays a significant role in guiding treatment options, especially in clinical settings.
Identifying bacterial types through Gram staining allows researchers and healthcare professionals to quickly categorize organisms as either Gram-positive or Gram-negative. These categories help determine the most effective antibiotics to combat bacterial infections, as the cell wall structure influences how bacteria respond to certain drugs.
Gram-positive bacteria have thick cell walls that retain the crystal violet stain, resulting in a purple appearance under the microscope. In contrast, Gram-negative bacteria possess thinner walls and an outer membrane that does not hold the stain, causing them to appear pink after a counterstaining procedure.
The ability to rapidly distinguish between these two groups provides vital information for diagnosing infections, guiding treatment decisions, and understanding bacterial resistance mechanisms. Thus, Gram staining remains an indispensable tool in microbiological analysis and research.
Viral Structure and Classification
Understanding the structure and classification of viruses is crucial for studying their behavior, replication, and impact on hosts. Viruses are unique entities that differ significantly from living organisms, yet their ability to infect and replicate within host cells is what makes them of great interest to researchers and healthcare professionals alike.
Viral Structure

The structure of a virus is relatively simple but highly efficient for its purpose of infecting host cells. A typical virus consists of the following components:
- Capsid: A protein shell that protects the genetic material inside. It is made up of protein subunits called capsomers.
- Genome: The viral genetic material, which can be either DNA or RNA, and encodes the instructions for making new virus particles.
- Envelope: Some viruses have an additional lipid membrane derived from the host cell. This outer layer helps the virus to enter host cells.
- Spikes: Protein structures on the surface of certain viruses that facilitate attachment to host cells.
Viral Classification

Classifying viruses is more complex than for other microorganisms due to their vast diversity. The classification is primarily based on:
- Type of Genome: Whether the virus contains RNA or DNA, and whether the genome is single-stranded or double-stranded.
- Symmetry of the Capsid: Viruses can have helical, icosahedral, or complex capsid shapes.
- Presence of Envelope: Viruses can be enveloped or non-enveloped, depending on whether they possess the lipid layer.
- Host Range: Some viruses are specific to particular hosts, such as animals, plants, or bacteria (bacteriophages).
These factors are essential for determining the viral family’s name, its pathogenic potential, and the methods used to combat infections caused by that virus.
Host-Parasite Relationships Explained
The interaction between a host organism and a parasitic entity is a fundamental aspect of many biological systems. In this relationship, the parasite benefits at the expense of the host, often causing harm in the process. Understanding how these interactions unfold is essential for grasping the impact of parasitic organisms on their hosts, including the potential for disease transmission and the development of resistance.
There are several types of relationships between hosts and parasites, each with varying degrees of harm or benefit to the organisms involved. In many cases, the parasite exploits the host’s resources for its survival and reproduction. While some parasitic relationships are highly specialized, others can involve more generalist interactions.
Types of Host-Parasite Relationships
- Mutualism: In some cases, both the host and the parasite benefit from the relationship. For example, certain bacteria in the gut help with digestion while receiving nutrients in return.
- Commensalism: Here, the parasite benefits without harming the host. The host remains unaffected, while the parasite gets a free ride or access to resources.
- Parasitism: The classic form of this relationship, where the parasite derives benefits from the host, often at its expense. This can lead to disease, malnutrition, or other health complications for the host.
Impact of Parasites on Hosts
Parasites can have various effects on their hosts. Some cause immediate physical damage or illness, while others may weaken the host over time. The degree of harm depends on factors such as the parasite’s virulence, the host’s immune system, and environmental conditions.
In some cases, parasites can manipulate the host’s behavior or physiology to enhance their own survival and reproduction. This makes the study of host-parasite dynamics critical for both medical science and environmental biology, as it informs strategies for preventing and treating parasitic infections.
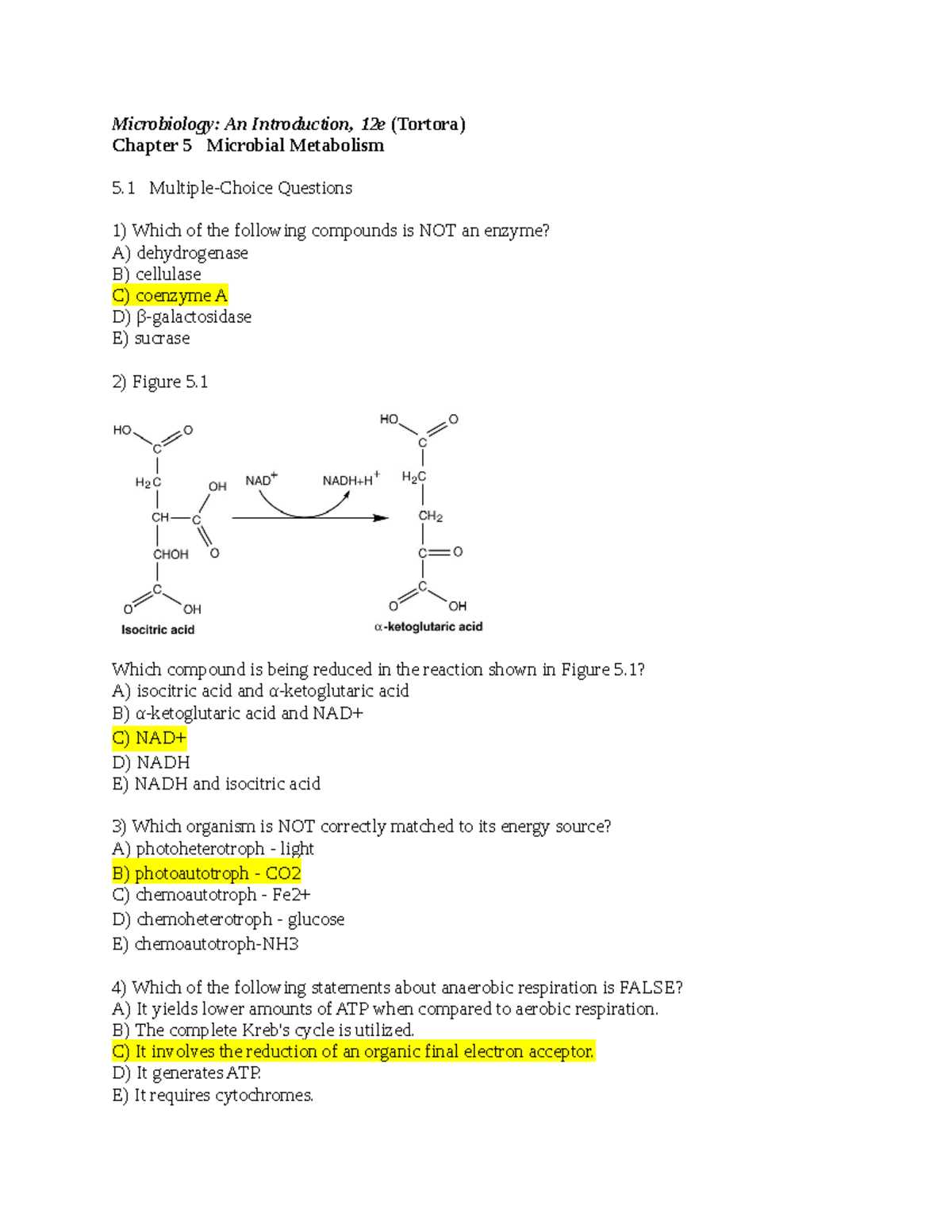
Metabolic Pathways in Microorganisms
Microorganisms exhibit a variety of metabolic pathways that allow them to extract energy and nutrients from their environment. These pathways are crucial for survival, enabling microbes to thrive in different habitats, whether they are living in extreme environments or symbiotically within a host. By converting raw materials into usable forms of energy, microorganisms support their growth, reproduction, and adaptation to changing conditions.
Metabolic processes in microorganisms can be broadly categorized into two types: catabolic pathways, which break down molecules to release energy, and anabolic pathways, which build complex molecules using energy. Both types of processes are intricately linked and regulated, ensuring that the microorganism maintains a balance between energy production and usage.
Common Metabolic Pathways
Some key metabolic pathways in microorganisms include:
| Pathway | Function | End Products |
|---|---|---|
| Glycolysis | Breaks down glucose to produce energy (ATP) and pyruvate. | ATP, Pyruvate |
| Citric Acid Cycle (Krebs Cycle) | Further breaks down products from glycolysis to produce more ATP and electron carriers. | ATP, NADH, FADH2, CO2 |
| Fermentation | Occurs when oxygen is scarce; converts pyruvate into various products to regenerate NAD+. | Lactic acid, Ethanol, ATP |
| Respiration (Aerobic and Anaerobic) | Uses oxygen or other molecules as the final electron acceptor to generate a large amount of ATP. | ATP, Water (aerobic), Various end products (anaerobic) |
Understanding these metabolic pathways is essential for grasping how microorganisms adapt to their environment and respond to external stresses, such as nutrient availability or oxygen levels. This knowledge is also pivotal in biotechnology, medicine, and environmental sciences, where manipulating these pathways can lead to practical applications, such as antibiotic production or waste treatment.
Antibiotic Resistance Overview
Antibiotic resistance occurs when microorganisms evolve mechanisms to resist the effects of drugs that once successfully treated infections. This phenomenon poses a significant challenge to healthcare systems worldwide, as it reduces the effectiveness of treatments for common and severe diseases. The rise of resistant strains is driven by several factors, including the overuse and misuse of antibiotics, as well as the natural mutation process that allows microbes to adapt to their environment.
When resistance develops, previously treatable infections can become more difficult or even impossible to cure, leading to longer hospital stays, increased medical costs, and higher mortality rates. Understanding the mechanisms behind antibiotic resistance is crucial for developing strategies to combat this growing threat.
Mechanisms of Antibiotic Resistance
Microorganisms can acquire resistance to antibiotics through several mechanisms, including:
| Mechanism | Description |
|---|---|
| Enzyme Production | Some bacteria produce enzymes that break down or inactivate antibiotics, rendering them ineffective. For example, beta-lactamases can destroy beta-lactam antibiotics like penicillin. |
| Target Modification | Changes in the bacterial target sites, such as cell wall components or ribosomes, can prevent antibiotics from binding effectively. |
| Efflux Pumps | Certain bacteria can actively pump out antibiotics from their cells before they can exert their effect, making them less susceptible to treatment. |
| Reduced Permeability | Some microorganisms alter their cell membranes to prevent antibiotics from entering, effectively blocking the drug’s action. |
The spread of antibiotic-resistant strains is accelerated by the inappropriate use of antibiotics, such as taking them for viral infections or not completing prescribed courses of treatment. Moreover, agricultural practices that involve the use of antibiotics to promote growth in healthy animals further contribute to resistance development. Efforts to combat antibiotic resistance include improved antibiotic stewardship, infection prevention practices, and the development of new antimicrobial agents. Addressing this issue requires a collaborative approach from healthcare providers, researchers, policymakers, and the general public to slow the spread and preserve the effectiveness of antibiotics.
Immune System Response to Infections

The body’s defense mechanisms are activated when harmful microorganisms invade, triggering a series of complex processes designed to neutralize and eliminate the threat. This intricate system involves various cells, proteins, and organs working together to recognize, attack, and remember infectious agents. The response is typically divided into two primary stages: the innate immune response, which provides immediate defense, and the adaptive immune response, which takes longer to develop but offers more targeted protection.
Each stage of the immune response plays a critical role in defending the body. The innate response acts as a first line of defense, involving physical barriers such as skin and mucous membranes, as well as white blood cells that recognize and attack invaders. If the infection persists, the adaptive response kicks in, involving specialized cells that specifically target and remember the pathogen for faster recognition during future encounters.
Innate Immune Response
The innate immune system provides a rapid but generalized defense against pathogens. Key components include:
- Phagocytes: White blood cells, such as macrophages and neutrophils, engulf and digest foreign particles.
- Complement System: A group of proteins that work together to enhance the immune response by marking pathogens for destruction and promoting inflammation.
- Inflammation: A localized response to infection that increases blood flow and attracts immune cells to the site of infection.
Adaptive Immune Response
The adaptive immune system targets specific pathogens and creates long-lasting immunity. Key elements of this response include:
- B-cells: These cells produce antibodies that bind to pathogens, neutralizing them or marking them for destruction.
- T-cells: Helper T-cells coordinate the immune response, while cytotoxic T-cells directly kill infected cells.
- Memory Cells: After an infection is cleared, memory cells remain in the body, allowing the immune system to respond more quickly if the same pathogen is encountered again.
Effective immune responses depend on the timely activation of both innate and adaptive mechanisms. However, in some cases, infections can evade or suppress immune defenses, leading to chronic infections or the development of diseases. Understanding the immune system’s response to infections is crucial for developing new vaccines, treatments, and therapies to combat infectious diseases.
Common Microbial Diseases
Infections caused by various microorganisms are widespread and can affect individuals of all ages. These diseases range from mild illnesses to severe conditions that can result in long-term health complications or even death. The pathogens responsible for these diseases can include bacteria, viruses, fungi, and parasites, each with unique characteristics that enable them to infect and spread in the host organism.
Common microbial diseases can be transmitted through a variety of means, including direct contact, contaminated food or water, airborne particles, and vectors like insects. Recognizing the symptoms and understanding the causative organisms are essential for timely diagnosis and treatment. Below are some of the most prevalent infectious diseases caused by microorganisms:
Bacterial Infections
- Streptococcal Pharyngitis: Caused by *Streptococcus* bacteria, commonly known as strep throat, leading to sore throat, fever, and swollen lymph nodes.
- Tuberculosis: A serious lung infection caused by *Mycobacterium tuberculosis*, which can spread to other organs if untreated.
- Salmonellosis: A foodborne illness caused by *Salmonella* bacteria, leading to gastrointestinal distress, fever, and diarrhea.
- Pneumonia: A respiratory infection often caused by *Streptococcus pneumoniae*, which results in symptoms like cough, fever, and difficulty breathing.
Viral Infections
- Influenza: Caused by the influenza virus, this disease is marked by fever, chills, body aches, and respiratory symptoms.
- Hepatitis: A viral infection affecting the liver, with types A, B, C, D, and E causing symptoms like jaundice, fatigue, and abdominal pain.
- Common Cold: A viral upper respiratory infection that leads to a runny nose, sore throat, and mild fever.
- COVID-19: Caused by the SARS-CoV-2 virus, this disease has symptoms ranging from mild respiratory issues to severe pneumonia and organ failure.
Fungal Infections

- Ringworm: A common skin infection caused by fungi, characterized by itchy, red, circular patches on the skin.
- Candidiasis: An overgrowth of *Candida* fungi, often affecting the mouth, throat, or genital areas, causing itching, burning, and discharge.
- Athlete’s Foot: A fungal infection of the feet that leads to itching, burning, and cracked skin between the toes.
Parasitic Infections
- Malaria: A deadly disease caused by *Plasmodium* parasites, transmitted through the bite of an infected mosquito, causing fever, chills, and anemia.
- Giardiasis: Caused by the *Giardia* parasite, this intestinal infection leads to diarrhea, stomach cramps, and nausea.
- Lice Infestation: Caused by the *Pediculus* parasite, lice infest the scalp and cause itching and discomfort.
While these microbial diseases are common, many can be prevented through vaccination, good hygiene practices, and proper sanitation. Early detection and treatment are crucial in reducing the spread and impact of these infections. With advances in medicine, many microbial diseases are now treatable or preventable, though challenges like antimicrobial resistance continue to complicate global health efforts.
Microbial Control Methods
Controlling harmful microorganisms is essential in preventing infections and maintaining public health. Various methods can be employed to either eliminate or reduce microbial populations in different environments, such as in medical settings, food production, and everyday hygiene. The techniques used depend on the type of microorganism, the environment, and the desired level of sterilization or disinfection. Below, we explore some of the most common approaches for microbial control.
Physical Control Methods
- Heat Sterilization: This method involves using high temperatures to kill microorganisms. Autoclaving and boiling are common techniques used in laboratories and healthcare settings to sterilize equipment.
- Cold Storage: Lowering the temperature can slow down or stop the growth of microorganisms. Refrigeration and freezing are often used to preserve food and prevent spoilage.
- Radiation: Ultraviolet (UV) light and gamma rays are used to destroy microorganisms by damaging their DNA. UV radiation is commonly used to disinfect water and air in hospitals and laboratories.
- Filtration: This method physically removes microorganisms from liquids and air. It is often used in water treatment plants and in the preparation of sterile solutions for medical use.
Chemical Control Methods
- Antiseptics: These are chemicals used on living tissues to kill or inhibit the growth of harmful microorganisms. Common antiseptics include alcohol, iodine, and hydrogen peroxide, which are used in wound care and hand sanitizers.
- Disinfectants: Disinfectants are used on inanimate objects and surfaces to reduce or eliminate microbial populations. Household cleaners, bleach, and phenols are examples of disinfectants commonly used in healthcare and home environments.
- Antibiotics: These are chemical agents that specifically target and kill bacterial cells. Antibiotics are widely used to treat bacterial infections, although antibiotic resistance is a growing concern.
- Gaseous Agents: Gaseous chemicals such as ethylene oxide are used to sterilize equipment that cannot withstand heat. This method is often applied in medical and laboratory equipment sterilization.
In addition to these methods, proper hygiene practices, such as regular hand washing and the use of personal protective equipment, play an essential role in controlling the spread of microorganisms. The choice of control method is influenced by several factors, including the type of microorganism, the surface or medium to be treated, and the potential risks of resistance. By employing a combination of these methods, we can significantly reduce the risks posed by harmful pathogens in our environment.
Understanding Genetic Mutations
Genetic mutations are alterations in the DNA sequence that can occur naturally or be induced by environmental factors. These changes may affect the structure and function of genes, leading to various outcomes for the organism. While some mutations have no significant effect, others can be harmful or beneficial. The understanding of these mutations is crucial for comprehending how organisms evolve, how diseases develop, and how they can be treated or prevented.
Mutations can take several forms, including point mutations, where a single nucleotide is altered, and insertions or deletions, where additional nucleotides are added or removed from the sequence. These alterations can result in the production of dysfunctional proteins, which may lead to diseases, or they can drive evolutionary changes that allow an organism to better adapt to its environment.
Types of Genetic Mutations
- Silent Mutations: These mutations do not result in any change to the protein produced, as the altered codon still codes for the same amino acid.
- Missense Mutations: A single nucleotide change leads to the substitution of one amino acid for another in the protein sequence, which can alter the protein’s function.
- Nonsense Mutations: These mutations introduce a premature stop codon, resulting in a truncated and usually nonfunctional protein.
- Frameshift Mutations: Insertions or deletions that alter the reading frame of the gene, usually leading to a completely different protein sequence.
While mutations can be harmful, they are also a source of genetic variation and can contribute to the development of new traits. In some cases, beneficial mutations can give an organism a survival advantage, which may be passed on to future generations. However, harmful mutations can result in genetic disorders or increase the organism’s susceptibility to certain diseases.
Understanding how mutations occur and their potential impacts is essential for fields such as genetics, medicine, and evolutionary biology. By studying these changes, scientists can develop new treatments for genetic disorders, improve disease prevention methods, and gain deeper insights into the mechanisms of heredity and evolution.
Practical Lab Techniques in Microbiology

Laboratory techniques are essential tools for studying microorganisms, providing accurate data on their behavior, growth patterns, and characteristics. These techniques are used in various fields, including research, medicine, and environmental science, to isolate, identify, and analyze microbial specimens. Mastery of these methods is vital for conducting experiments, diagnosing infections, and advancing scientific knowledge.
Among the most common lab techniques, some are fundamental to working with microorganisms, while others are specialized for specific tasks. These methods include culturing, staining, and microscopy, which allow scientists to observe microorganisms, understand their structure, and determine their properties.
Key Laboratory Techniques
- Culturing Techniques: The process of growing microorganisms under controlled conditions. Common methods include agar plates, broth cultures, and selective media, which help isolate specific types of organisms.
- Staining Methods: Staining allows for better visualization of microorganisms under a microscope. Techniques such as Gram staining and acid-fast staining help differentiate between bacterial species based on their cell wall composition.
- Microscopy: Various types of microscopes, including light and electron microscopes, are used to examine microorganisms. Microscopy allows for detailed observation of cell structure, shape, and size.
- Inoculation: Introducing microorganisms into a medium to grow and study their behavior. This can be done through streak plating, spreading, or serial dilution.
Each of these methods plays a critical role in microbial research. Culturing techniques enable scientists to obtain pure samples of microorganisms for further study, while staining methods provide clarity when viewing organisms under a microscope. Proper inoculation and media preparation are fundamental for successful experimentation, ensuring that researchers can grow and maintain microbial cultures.
In addition to basic techniques, more advanced methods such as PCR (Polymerase Chain Reaction) and gel electrophoresis allow for the detection and analysis of microbial DNA, enhancing the ability to identify specific pathogens or genetic traits.
By applying these techniques in a systematic and controlled manner, researchers can uncover important information about microbial life, leading to advances in disease diagnosis, treatment, and environmental management.
Microbiology Test Preparation Tips
Preparing for an exam in the field of microbial science requires a combination of effective study techniques and a deep understanding of core concepts. Mastering the material not only helps improve your grades but also strengthens your ability to apply knowledge in practical settings. Whether you are reviewing for a quiz, midterm, or final exam, a structured approach to preparation is key to success.
1. Organize Your Study Material
Before diving into studying, gather all the necessary resources. This includes lecture notes, textbooks, online materials, and any practice questions provided. Organizing your materials into key topics will help ensure that you cover everything efficiently and avoid missing crucial areas of study.
- Focus on Key Areas: Identify the main concepts that are frequently covered in exams, such as microbial classification, growth conditions, and immune responses. These topics are often the most emphasized in questions.
- Break Down Complex Information: Microbial processes and pathogen behavior can be complex. Create simplified summaries or diagrams to help break down complicated processes into manageable parts.
- Review Lecture Notes Regularly: Regularly revisit your class notes to reinforce what you’ve learned and fill in any gaps in your understanding.
2. Active Learning Strategies
Rather than passively reading through your notes or textbook, engage with the material in an active way. This approach has been proven to improve retention and understanding.
- Practice with Flashcards: Create flashcards to help memorize important terms, definitions, and processes. Digital flashcard apps can make it easy to review on the go.
- Teach the Material: Explaining key concepts to a study partner or even to yourself can deepen your understanding. Teaching forces you to clarify your thinking and reinforce your grasp of the material.
- Do Practice Questions: Working through sample questions, quizzes, or past exam papers will familiarize you with the format and help identify areas where you need more review.
By organizing your study material effectively and engaging in active learning strategies, you will be better prepared to tackle exam questions with confidence. Combining these techniques with proper time management will help ensure that you can approach the exam with a clear, focused mind.
Frequently Asked Questions on Chapter 5
When studying complex biological topics, it is common to have questions that arise during the learning process. These questions often focus on key concepts, terminology, and processes that require clarification. Below, we address some of the most frequently asked questions related to the current subject matter, providing clear explanations to help reinforce understanding and aid in your studies.
1. What is the importance of understanding microbial classification?
Understanding how different microorganisms are classified is essential because it helps identify their characteristics, behaviors, and potential impacts on the environment and human health. This knowledge allows researchers and healthcare professionals to better target treatments, manage diseases, and understand the ecological roles of various microbes.
2. How do environmental factors affect microbial growth?
Environmental conditions such as temperature, pH, oxygen levels, and nutrient availability play a crucial role in microbial growth. By understanding these factors, scientists can manipulate conditions in lab settings or clinical environments to control microbial populations for both research and medical purposes.
| Factor | Effect on Microbial Growth |
|---|---|
| Temperature | Microbes have optimal temperature ranges for growth. Extreme temperatures can inhibit or kill them. |
| pH Levels | Most microbes prefer a neutral pH, but some thrive in acidic or alkaline environments. |
| Oxygen Availability | Aerobic microbes need oxygen, while anaerobic ones grow in its absence. |
| Nutrient Availability | Adequate nutrients are essential for microbial growth and reproduction. |
By understanding these factors, we can better control microbial growth in various contexts, from clinical settings to industrial applications.