In the field of healthcare, understanding the complex relationship between regulations, patient rights, and professional conduct is essential. This knowledge not only helps in ensuring safe practices but also prepares individuals for the rigorous assessments they must face. A thorough grasp of the core principles is crucial for passing the required assessments in this area of study.
Healthcare professionals are often required to make difficult decisions that balance legal responsibilities and moral considerations. With this in mind, preparation for the related evaluations involves reviewing the foundational concepts that govern practice, focusing on responsibility, patient autonomy, and professional accountability. Mastering these topics is key to both academic success and effective patient care.
Understanding how legal standards influence healthcare decisions and how ethical guidelines shape interactions with patients is vital for anyone aiming to excel. These principles guide practitioners in navigating everyday situations, from simple procedures to complex treatments, ensuring that all actions are in the best interest of those under their care. Knowing how to handle these principles under pressure is what this assessment ultimately tests.
Medical Law and Ethics Final Exam

In healthcare practice, professionals are regularly faced with situations where the right course of action must be determined based on a combination of regulations and moral principles. The ability to navigate these challenges effectively is crucial, not just for patient care, but for maintaining professional standards and legal compliance. This section is designed to help individuals prepare for assessments that test their understanding of these critical concepts.
Core Concepts and Key Areas of Focus
Successful preparation involves mastering the foundational concepts that guide decision-making in healthcare settings. This includes understanding patient rights, confidentiality, informed consent, and the professional responsibilities that practitioners must uphold. Additionally, the balance between personal morals and public duties is a central theme that requires careful attention during the evaluation process. Strong knowledge of these areas ensures that individuals are prepared to make ethical decisions in complex scenarios.
Test Preparation Strategies
Effective revision is essential for success in these assessments. Focus on case studies, real-world scenarios, and the application of theoretical knowledge in practical situations. Use practice questions and mock tests to refine understanding and improve critical thinking skills. This approach helps in not only recalling key concepts but also applying them to challenging situations in a high-pressure environment.
Familiarizing oneself with the structure of the test and understanding the types of questions asked can further boost confidence. This strategy enables individuals to approach each topic systematically and confidently, ensuring thorough preparation.
Key Principles of Medical Law
In healthcare, professionals must adhere to a set of guiding principles that ensure safety, fairness, and respect for individuals. These principles shape the way practitioners interact with patients, make decisions, and comply with standards that protect both parties. A solid understanding of these concepts is essential for anyone navigating the complexities of healthcare practice.
Fundamental Concepts in Healthcare Regulation
Several key ideas provide the foundation for professional behavior and responsibility in medical settings. Among them are:
- Patient Autonomy: The right of individuals to make informed decisions about their care, free from coercion or undue influence.
- Beneficence: The obligation to act in the best interest of patients, promoting their well-being and preventing harm.
- Non-maleficence: The principle of “do no harm,” ensuring that actions taken do not cause unnecessary injury or suffering.
- Justice: Ensuring fairness in treatment and resource allocation, regardless of personal characteristics or status.
Responsibilities of Healthcare Professionals

Healthcare providers are entrusted with a great deal of responsibility. Their duties include:
- Maintaining patient confidentiality and respecting privacy rights at all times.
- Providing accurate, truthful information to patients about their condition and treatment options.
- Ensuring informed consent is obtained before any intervention or procedure.
- Complying with relevant regulations and standards of care set by regulatory bodies.
By understanding and applying these principles, healthcare practitioners ensure that they are acting in the best interests of their patients while staying within the boundaries set by the healthcare system.
Ethical Dilemmas in Healthcare Practice
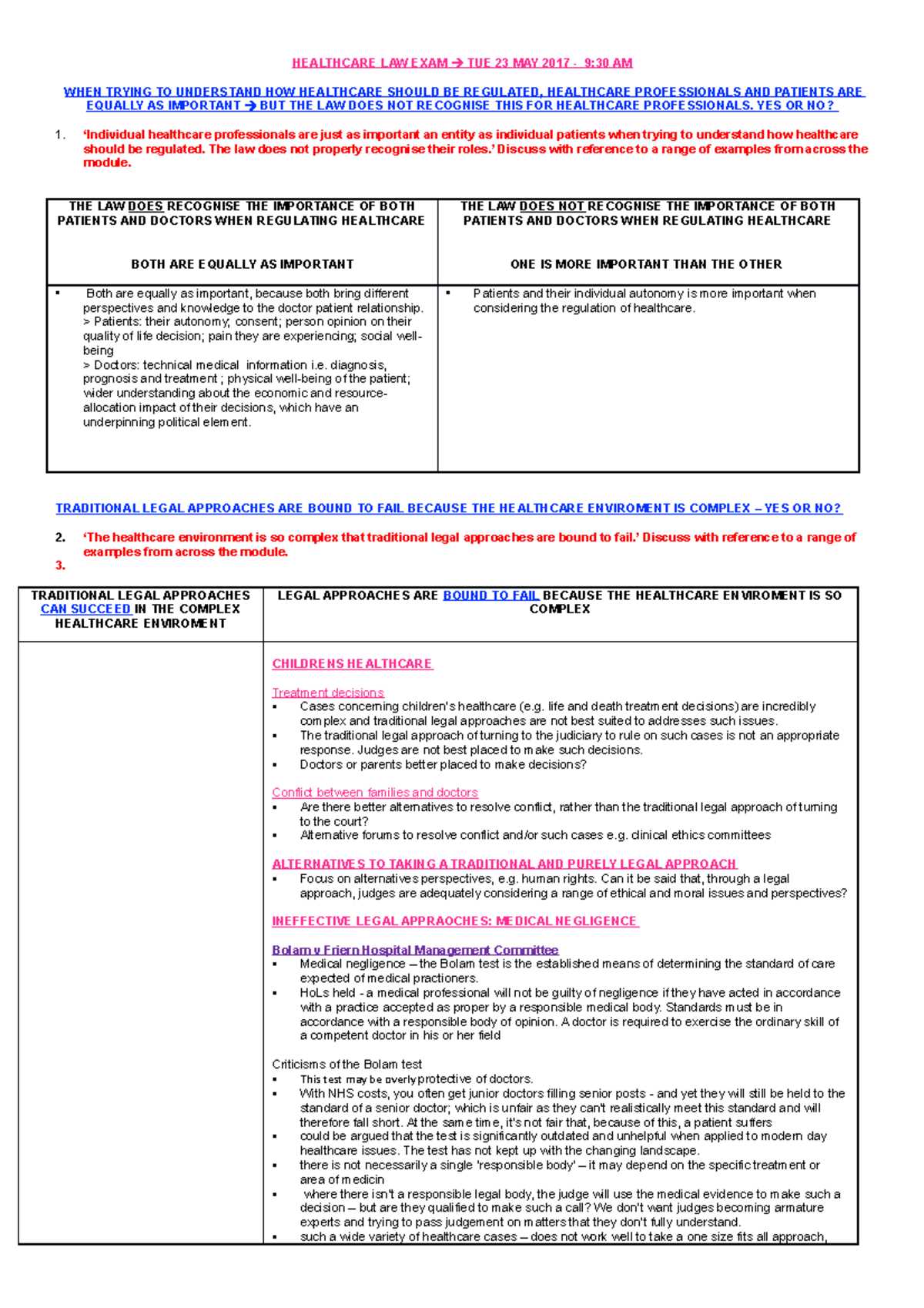
In the healthcare field, professionals often face situations where the right course of action is unclear, with competing interests and conflicting principles at play. These complex scenarios require careful consideration and decision-making, balancing the needs and rights of patients with broader social and professional responsibilities. Navigating these dilemmas is essential for maintaining trust, respect, and integrity in patient care.
One of the key challenges is managing situations where personal values might conflict with professional obligations. For example, a healthcare provider may have to decide whether to respect a patient’s wish for a treatment that contradicts their professional judgment or best interests. Such decisions demand not only knowledge of regulatory frameworks but also a deep understanding of moral principles.
Common ethical challenges in healthcare include:
- End-of-life decisions: Determining when to continue or withdraw life-sustaining treatments, respecting patient autonomy while considering quality of life.
- Confidentiality breaches: Balancing the need to maintain patient privacy against circumstances where disclosure is necessary for the safety or well-being of others.
- Resource allocation: Deciding how to fairly distribute limited medical resources, such as organs for transplant or ICU beds, especially during crises.
- Consent in vulnerable populations: Obtaining informed consent from individuals who may not fully understand the implications of medical procedures, such as minors or those with cognitive impairments.
Each of these challenges requires healthcare professionals to carefully consider the implications of their actions and make decisions that prioritize patient well-being while aligning with societal and professional values. Ethical reasoning, communication with patients, and collaboration with colleagues are all essential components of navigating these difficult scenarios.
Understanding Patient Rights and Consent
In healthcare, respecting the rights of patients is fundamental to ensuring safe and compassionate care. Central to these rights is the principle of consent, which grants individuals the autonomy to make informed decisions about their treatment. Understanding how to properly obtain consent, while also respecting personal boundaries, is a vital responsibility for all healthcare providers.
Patients have the right to be fully informed about their medical condition, treatment options, and the risks involved. This ensures that they can make decisions that align with their values and preferences. Healthcare providers must ensure that this process is transparent, respectful, and thorough.
| Type of Consent | Description |
|---|---|
| Informed Consent | The patient is fully informed about the risks, benefits, and alternatives of a procedure or treatment before agreeing to it. |
| Implied Consent | Consent that is assumed based on the patient’s actions, such as agreeing to a physical examination. |
| Expressed Consent | Consent that is given explicitly, either verbally or in writing, for a specific procedure or treatment. |
| Emergency Consent | Consent obtained in urgent situations where the patient is unable to provide consent and immediate action is required to preserve life. |
Ensuring that patients understand the information provided to them, and that consent is obtained in a clear and uncoerced manner, is essential for both legal and moral reasons. In cases where consent cannot be obtained directly from the patient, healthcare providers must look to legally recognized substitutes, such as a family member or legal guardian, to ensure that the patient’s best interests are preserved.
Legal Frameworks for Medical Professionals
Healthcare providers operate within a structured set of regulations that guide their professional conduct and ensure patient safety. These frameworks are designed to establish clear boundaries and provide guidance on acceptable practices. Adhering to these guidelines is essential for practitioners, as non-compliance can lead to significant legal consequences and undermine trust in the healthcare system.
Core Regulations for Healthcare Providers
Various principles and rules govern the conduct of healthcare professionals. These regulations focus on ensuring the safety and well-being of patients while maintaining high standards of care. Some key areas include:
- Standard of Care: The level of care expected from a reasonable healthcare provider in a similar situation.
- Licensing and Certification: Requirements that ensure healthcare professionals have the necessary education and training to practice safely.
- Patient Rights: Laws that protect the autonomy, privacy, and dignity of patients.
- Informed Consent: Legal requirements ensuring that patients understand the risks, benefits, and alternatives of medical procedures.
Compliance with Healthcare Regulations
Healthcare professionals must also comply with a variety of organizational and governmental regulations that address safety, ethical treatment, and accountability. These rules cover a broad range of topics, from handling confidential patient information to ensuring equitable access to care. Practitioners are required to:
- Understand local, national, and international standards that apply to their specific field of practice.
- Follow guidelines established by professional associations and regulatory bodies.
- Participate in ongoing education to stay up-to-date with evolving standards and best practices.
By adhering to these established frameworks, healthcare providers can mitigate legal risks and ensure that their practice is aligned with professional expectations, protecting both their patients and themselves.
Legal Frameworks for Medical Professionals
Healthcare providers operate within a structured set of regulations that guide their professional conduct and ensure patient safety. These frameworks are designed to establish clear boundaries and provide guidance on acceptable practices. Adhering to these guidelines is essential for practitioners, as non-compliance can lead to significant legal consequences and undermine trust in the healthcare system.
Core Regulations for Healthcare Providers
Various principles and rules govern the conduct of healthcare professionals. These regulations focus on ensuring the safety and well-being of patients while maintaining high standards of care. Some key areas include:
- Standard of Care: The level of care expected from a reasonable healthcare provider in a similar situation.
- Licensing and Certification: Requirements that ensure healthcare professionals have the necessary education and training to practice safely.
- Patient Rights: Laws that protect the autonomy, privacy, and dignity of patients.
- Informed Consent: Legal requirements ensuring that patients understand the risks, benefits, and alternatives of medical procedures.
Compliance with Healthcare Regulations
Healthcare professionals must also comply with a variety of organizational and governmental regulations that address safety, ethical treatment, and accountability. These rules cover a broad range of topics, from handling confidential patient information to ensuring equitable access to care. Practitioners are required to:
- Understand local, national, and international standards that apply to their specific field of practice.
- Follow guidelines established by professional associations and regulatory bodies.
- Participate in ongoing education to stay up-to-date with evolving standards and best practices.
By adhering to these established frameworks, healthcare providers can mitigate legal risks and ensure that their practice is aligned with professional expectations, protecting both their patients and themselves.
Malpractice and Legal Liabilities
Healthcare professionals are entrusted with the well-being of their patients, but errors or negligence can lead to legal consequences and claims of professional misconduct. These situations often result in legal liabilities, where the provider may be held responsible for harm caused by a breach in the standard of care. Understanding the concept of malpractice and the legal responsibilities that come with professional practice is crucial for mitigating risks and maintaining ethical standards.
Malpractice refers to instances where a healthcare provider fails to meet the accepted standards of care, leading to harm or injury to the patient. This can include a variety of actions, such as misdiagnosis, surgical errors, or failure to obtain informed consent. The key elements in a malpractice claim typically include proof of duty, breach of duty, causation, and damages.
Legal liabilities for healthcare providers can arise from several scenarios:
- Negligence: Failure to act with reasonable care, resulting in patient harm. This can include mistakes in diagnosis, treatment, or medication administration.
- Failure to Inform: Not providing patients with the necessary information regarding treatment risks and alternatives, leading to issues of informed consent.
- Vicarious Liability: Legal responsibility of employers for the actions of their employees, meaning a healthcare institution can be held accountable for the actions of its staff.
To avoid legal consequences, healthcare professionals must adhere to established standards of care, practice within their scope of competence, and ensure that they obtain proper informed consent. Additionally, professional liability insurance can offer protection against potential malpractice claims, providing financial support in the event of a lawsuit.
Healthcare Regulations and Compliance
The healthcare sector operates under a comprehensive framework of rules and standards that ensure patient safety, quality of care, and fairness in treatment. Compliance with these regulations is essential for maintaining the integrity of healthcare institutions and professionals. These regulations not only safeguard patients but also ensure that providers meet legal, ethical, and professional obligations, preventing misuse and promoting transparency in healthcare practices.
Key Regulatory Bodies and Their Roles
Various organizations and governmental agencies set guidelines to regulate healthcare practices and ensure they meet established standards. These bodies oversee compliance and monitor healthcare delivery across different settings:
- Government Health Agencies: These agencies enforce national and regional policies, such as the Centers for Disease Control and Prevention (CDC) or the Food and Drug Administration (FDA), ensuring public safety and monitoring healthcare products and services.
- Professional Associations: Organizations like the American Medical Association (AMA) set professional standards, codes of conduct, and best practices for healthcare providers, ensuring ethical behavior and patient-centered care.
- Accrediting Bodies: Institutions such as The Joint Commission accredit healthcare facilities, ensuring they meet rigorous standards for quality care and operational effectiveness.
Compliance Requirements for Healthcare Providers
Healthcare providers must adhere to various regulations that govern their practice. These compliance standards cover a wide range of topics, from patient rights to workplace safety, and ensure that patients receive the highest standard of care:
- Privacy Protection: Regulations like the Health Insurance Portability and Accountability Act (HIPAA) mandate strict guidelines to protect patient data and ensure confidentiality.
- Patient Safety: Healthcare organizations must comply with safety standards that prevent harm and improve outcomes for patients, including protocols for infection control, medication safety, and risk management.
- Licensing and Certification: Healthcare professionals are required to maintain valid licenses and certifications to practice, ensuring that they have the necessary training and expertise to provide care.
By adhering to these regulations, healthcare providers help to maintain a trustworthy and transparent system where patients can feel confident in the care they receive. Compliance not only helps avoid legal repercussions but also fosters a culture of safety and ethical responsibility in healthcare settings.
Role of Ethics Committees in Healthcare
In healthcare settings, difficult decisions often arise that require careful consideration of both moral principles and practical implications. Ethics committees play a crucial role in guiding healthcare providers through these complex situations. These committees are designed to offer advice, promote ethical decision-making, and ensure that patient care aligns with established moral standards. By evaluating cases from multiple perspectives, they help to resolve conflicts and support healthcare professionals in making informed, responsible choices.
Functions and Responsibilities of Ethics Committees
Ethics committees are instrumental in addressing a wide range of issues within healthcare institutions. Their primary responsibilities include:
- Advising on Complex Cases: Ethics committees offer guidance on cases where there is a moral or ethical dilemma, such as end-of-life decisions, organ transplantation, or conflicts of interest.
- Policy Development: They contribute to the creation of policies that reflect ethical principles and legal standards, ensuring the organization operates with integrity and responsibility.
- Supporting Healthcare Providers: These committees provide support to doctors, nurses, and other healthcare professionals in making decisions that align with both patient welfare and ethical standards.
Composition of Ethics Committees
The effectiveness of ethics committees relies on their diverse composition, ensuring that various perspectives are taken into account when evaluating complex issues:
| Role | Responsibilities |
|---|---|
| Healthcare Professionals | Provide expertise in clinical care and treatment protocols, offering insight into medical options and risks. |
| Ethicists | Guide discussions with a deep understanding of moral principles, helping to navigate difficult decisions. |
| Legal Experts | Ensure that recommendations align with legal regulations, protecting the institution and professionals from liability. |
| Community Representatives | Provide input on public perceptions and cultural considerations, ensuring that decisions reflect the values of the broader community. |
By incorporating diverse viewpoints, ethics committees ensure that healthcare practices are both compassionate and responsible, allowing for well-rounded decision-making that respects the dignity of patients and aligns with professional standards.
Legal Aspects of End-of-Life Care
End-of-life care involves complex decisions regarding the treatment and comfort of patients approaching the final stages of life. Legal considerations play a critical role in ensuring that patients’ rights are respected while healthcare providers navigate these sensitive circumstances. Legal frameworks guide decision-making processes, helping to balance the patient’s autonomy with the need for compassionate care, while protecting both the healthcare professionals and institutions from potential liabilities.
Several key issues arise in end-of-life scenarios, including decisions about withholding or withdrawing life-sustaining treatment, managing patient consent, and addressing concerns related to the patient’s wishes. Legal documents, such as advance directives or living wills, play an essential role in ensuring that the patient’s preferences are followed even when they are unable to communicate their desires directly.
In addition to respecting the wishes of the patient, healthcare providers must adhere to local and national regulations that govern end-of-life care. These regulations provide clear guidance on matters such as:
- Informed Consent: Patients should be fully informed about their treatment options and any risks associated with life-sustaining interventions. Consent must be obtained for any procedure or treatment that may impact the patient’s quality of life or outcome.
- Advance Directives: These legal documents outline a patient’s preferences regarding life-sustaining treatment, should they become incapacitated or unable to make decisions.
- Physician-Assisted Dying: In some jurisdictions, laws govern the practice of physician-assisted death, where patients can request medical assistance in ending their own life, often under strict conditions.
Ultimately, the legal landscape of end-of-life care aims to ensure that healthcare providers uphold the dignity and rights of patients, while minimizing the potential for legal disputes. The intersection of patient autonomy, ethical considerations, and legal requirements continues to shape the way end-of-life care is approached worldwide.
Informed Consent and Ethical Considerations
Obtaining approval from a patient before any procedure or intervention is a cornerstone of respecting their autonomy. It involves providing comprehensive information so the individual can make a knowledgeable decision regarding their healthcare. This process goes beyond mere paperwork, ensuring that patients are aware of the potential outcomes and have the freedom to make choices aligned with their values and preferences.
Key Elements of Informed Consent
For consent to be valid, it must meet certain criteria, ensuring the patient understands and voluntarily agrees to the proposed action:
- Comprehension: Clear communication is vital, ensuring the patient understands the details of the procedure, including risks, benefits, and alternatives.
- Autonomy: Consent must be given freely, without external pressure, allowing the individual to make their own decisions without coercion.
- Capacity: The patient must have the mental ability to understand the provided information and make an informed choice. If necessary, a guardian or legal representative may step in to help.
Ethical Dilemmas in Consent
While informed consent is fundamental, healthcare providers often face ethical challenges, especially in complex or urgent situations. Some common dilemmas include:
- Vulnerable Patients: Individuals who are unable to fully comprehend the information–such as minors, those with cognitive impairments, or non-native speakers–may require extra support to ensure they understand the details of the decision.
- Emergency Circumstances: In situations where immediate action is required and the patient cannot provide consent, decisions may need to be made in their best interest, creating a conflict between ethical obligations and urgent care.
- Complex Decisions: When treatment involves experimental procedures or carries substantial risks, it can be difficult for patients to grasp the full extent of what they are agreeing to, requiring a more nuanced explanation and careful guidance from healthcare professionals.
Informed consent is an ongoing process, not just a one-time formality. It ensures that patients are not only aware of what is happening to them but are also empowered to make decisions about their own care, reinforcing the ethical responsibility of providers to respect the rights and dignity of every individual.
Medical Decision-Making and Autonomy
In healthcare, the right of individuals to make decisions about their own treatment is fundamental. Autonomy allows patients to choose or refuse interventions based on their own values, beliefs, and preferences. This principle not only empowers individuals but also ensures that they are central to the decision-making process, enhancing the respect for their dignity and personal rights.
Healthcare professionals are tasked with providing the necessary information to help patients understand their options, risks, and benefits, enabling informed decisions. However, challenges arise when patients face complex choices, and their understanding or decision-making ability may be compromised. In such cases, careful consideration must be given to both the ethical implications and the legal frameworks surrounding autonomy.
Key Aspects of Autonomy in Decision-Making
- Informed Choice: To make autonomous decisions, patients must be given clear, accurate, and comprehensive information about their condition and treatment options.
- Voluntary Consent: Autonomy is only valid when decisions are made freely, without pressure or coercion from external parties.
- Capacity to Decide: The ability to understand the situation and make decisions is central to autonomy. In cases of diminished capacity, such as minors or individuals with cognitive impairments, alternative decision-makers may be appointed.
Challenges to Autonomy
- Informed Consent in Crisis Situations: In urgent medical scenarios where time is critical, the ability to gain full consent may be compromised, raising ethical dilemmas about respecting autonomy versus the need for immediate intervention.
- Influence of Family or Culture: Sometimes, family members or cultural values may exert significant influence on a patient’s choices. Striking a balance between respecting autonomy and considering these external factors can be a delicate matter.
- Understanding Complex Medical Information: Some treatments, especially experimental ones, may involve complex risks and benefits. Patients may struggle to fully understand these details, complicating their ability to make truly informed decisions.
Ultimately, decision-making in healthcare is a shared responsibility between patients and providers. Ensuring that autonomy is respected requires a commitment to communication, understanding, and ethical considerations at every stage of care.
Impact of Medical Law on Patient Care
Regulations that govern healthcare practices play a critical role in shaping the quality of care patients receive. These frameworks are designed to ensure that healthcare providers operate within defined boundaries, protecting both patients and practitioners. While these rules can enhance patient safety and trust, they can also introduce complexities in the decision-making process, as medical professionals must navigate legal requirements while delivering compassionate care.
The implementation of guidelines influences everything from patient privacy to the consent process, often requiring healthcare professionals to balance legal obligations with ethical considerations. These frameworks ensure that care is provided in accordance with established standards, promoting fairness and accountability within the healthcare system.
Ensuring Patient Rights and Safety
- Patient Confidentiality: Legal structures help safeguard patient information, ensuring that personal data is kept secure and only shared with authorized individuals.
- Consent Process: Legal standards demand that patients are fully informed about their treatment options and agree voluntarily, thus respecting their autonomy.
- Access to Care: Healthcare regulations also protect the rights of patients to access necessary services, ensuring equality and fairness in treatment.
Challenges and Ethical Dilemmas
- Conflicting Priorities: At times, healthcare providers may face situations where legal requirements conflict with the best interests of the patient, leading to difficult decisions.
- Resource Allocation: Regulations on how resources are distributed can sometimes limit access to treatment, raising questions about fairness and justice in care delivery.
Ultimately, the impact of regulatory frameworks on patient care lies in finding a balance between ensuring legal compliance and providing compassionate, personalized treatment. By protecting patient rights and promoting accountability, these structures contribute significantly to the overall quality and trust in healthcare systems.
Legal Challenges in Medical Research
In the field of scientific discovery and healthcare innovation, researchers often face complex legal considerations that can influence the direction and scope of their work. These challenges arise from the need to protect participants’ rights while ensuring that studies are conducted responsibly and with due diligence. As advancements in treatment and technology continue, the regulatory landscape for research becomes increasingly intricate, requiring careful navigation to avoid potential legal pitfalls.
Compliance with guidelines and regulations is essential to ensure that research is not only effective but also ethically sound. Legal challenges may involve issues such as patient consent, intellectual property rights, data privacy, and the use of experimental treatments. These factors must be carefully balanced to maintain public trust and avoid legal repercussions.
Informed Consent and Participant Protection
- Voluntary Participation: Legal requirements dictate that participants must be fully informed about the research process, potential risks, and benefits before agreeing to take part.
- Protection of Vulnerable Populations: Special legal protections are in place for certain groups, such as minors, pregnant women, or those with impaired capacity, ensuring their safety in research settings.
- Ongoing Monitoring: Legal frameworks demand that research activities are regularly reviewed for compliance, with any adverse events or risks being promptly addressed.
Intellectual Property and Data Security
- Ownership of Discoveries: Researchers must navigate intellectual property laws to determine the ownership rights of inventions or discoveries made during the course of their studies.
- Confidentiality of Data: Legal mandates require that personal data obtained from research participants be kept confidential, with strict penalties for breaches.
As research continues to evolve, legal challenges in this area are likely to grow in complexity. However, by adhering to established protocols and understanding the legal environment, researchers can contribute to scientific progress while safeguarding public trust and individual rights.
Ethical Considerations in Medical Education
In the training of future healthcare professionals, numerous moral dilemmas must be addressed to ensure that students develop both the technical expertise and the compassionate approach necessary for patient care. These considerations range from the treatment of patients during clinical training to the principles guiding interactions between students and instructors. The goal is to create an environment that fosters not only competence but also integrity, respect, and responsibility.
The development of students in healthcare education is not just about acquiring knowledge; it also involves instilling the values that will guide their professional behavior. The ethical challenges faced in educational settings can have lasting impacts on the future practices of healthcare workers. It is essential to balance rigorous training with a commitment to upholding ethical standards throughout the educational process.
Respect for Patient Autonomy and Confidentiality
- Informed Consent: During clinical training, students must be taught the importance of obtaining clear and voluntary consent from patients before involving them in any procedures or research.
- Privacy Protection: Maintaining patient confidentiality is a fundamental principle that students must understand and adhere to, both in the classroom and clinical settings.
Professionalism in the Learning Environment
- Honesty and Integrity: Students must be encouraged to demonstrate honesty in their interactions with patients, peers, and instructors, particularly when acknowledging limitations or mistakes.
- Respect for Diversity: Healthcare education programs should emphasize the importance of treating all individuals with respect, regardless of their background, race, gender, or other characteristics.
- Fairness in Evaluation: Ethical evaluation practices ensure that students are assessed on their abilities and not influenced by bias, providing a level playing field for all.
By addressing these ethical concerns, educational institutions can help prepare students to navigate the complex moral landscapes they will encounter in their careers, ultimately fostering a healthcare workforce committed to providing compassionate and ethical care.
Preparing for the Medical Law Exam
Successfully navigating the challenging assessments in the field of healthcare regulations requires a focused approach and thorough understanding of core principles. Preparation involves mastering key concepts, familiarizing oneself with practical scenarios, and understanding the legal frameworks that shape healthcare practice. It is essential to approach this process with a clear strategy, balancing theoretical knowledge with real-world applications.
One of the most effective ways to prepare is by reviewing case studies and practicing the application of regulations to various healthcare situations. Additionally, familiarizing yourself with the terminology and recognizing the implications of specific rules on patient care and provider responsibility can significantly enhance your ability to answer questions accurately and thoughtfully.
Key Topics to Focus On
- Rights and Responsibilities: Understand the legal rights of patients, healthcare providers’ responsibilities, and the role of consent in clinical settings.
- Patient Protection: Focus on privacy laws, confidentiality, and the regulations governing the handling of patient information.
- Clinical Accountability: Review standards for patient care and the potential legal consequences for failing to meet established practices.
Study Tips and Resources
| Study Method | Purpose |
|---|---|
| Practice Exams | Simulate the assessment environment and test your knowledge under time constraints. |
| Case Studies | Enhance your ability to apply legal principles to real-world situations. |
| Group Discussions | Engage with peers to discuss complex topics and different perspectives on legal challenges in healthcare. |
Thorough preparation not only helps you perform well on the assessment but also ensures that you are equipped to handle complex legal situations in your professional practice. With a solid understanding of the material and effective study habits, success in this area is well within reach.