In the world of medical training, practical simulations offer invaluable insights into patient care, allowing students to refine their diagnostic skills. By engaging with virtual patients, learners face real-life scenarios that enhance their clinical reasoning and decision-making abilities. These exercises are designed to test knowledge while challenging healthcare professionals to respond effectively to complex cases.
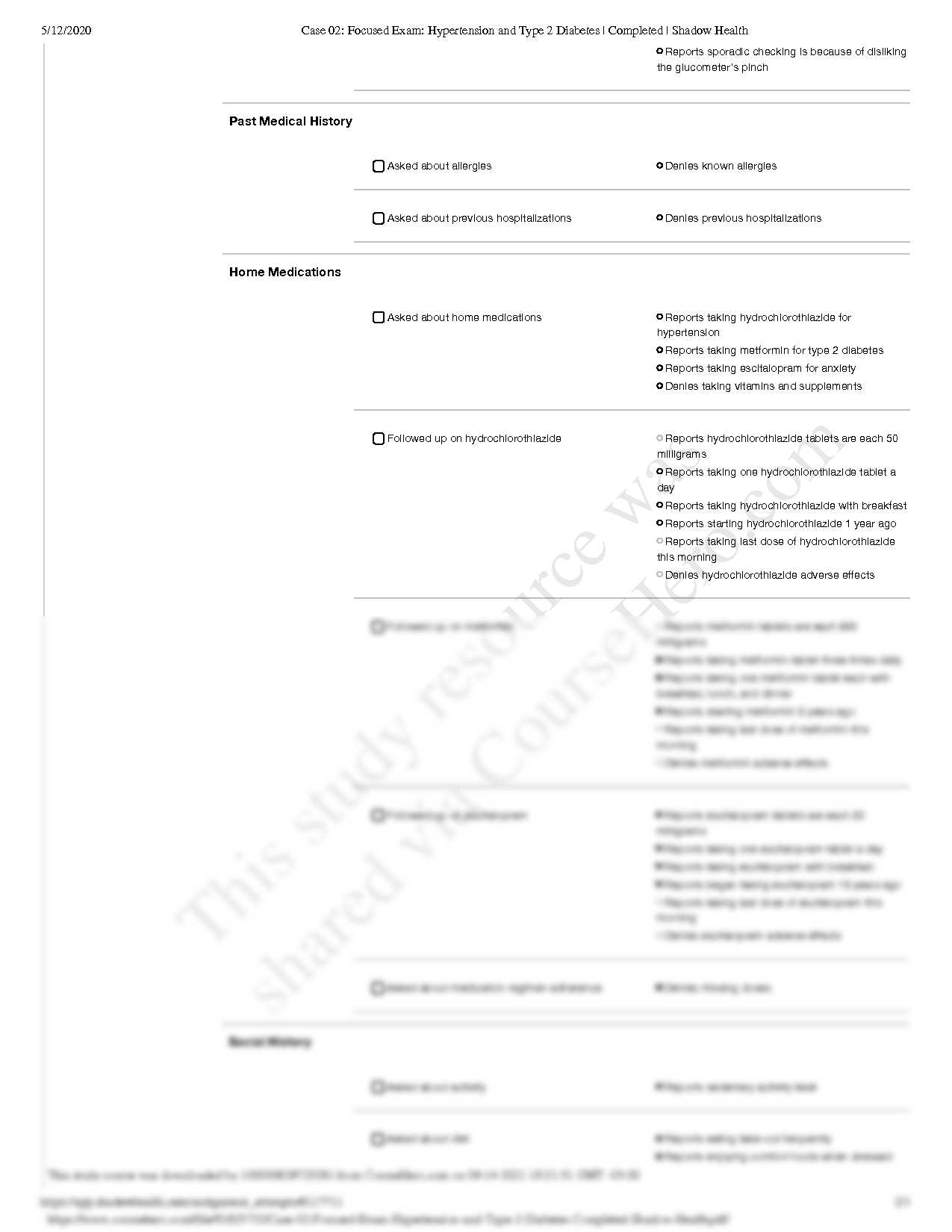
For those preparing for assessments that focus on long-term health issues, understanding the management of common chronic conditions is essential. The ability to identify key symptoms, evaluate risk factors, and propose appropriate treatment plans can make a significant difference in patient outcomes. Mastery of these areas not only helps students succeed in their assessments but also equips them with the necessary tools to provide high-quality care in clinical practice.
Practical experience is at the heart of developing a comprehensive understanding of chronic conditions, enabling students to interact with cases that require critical thinking. Through virtual simulations, learners are encouraged to apply their knowledge and problem-solving skills in real-time, ensuring they are well-prepared for future professional challenges.
Shadow Health Focused Exam Answers
When preparing for clinical simulations, mastering the key concepts of managing chronic conditions is essential. These assessments challenge students to apply their knowledge of patient care in realistic scenarios, ensuring that they can make informed decisions under pressure. Each case is crafted to test a range of competencies, from patient interaction to diagnosing and managing long-term illnesses.
Success in these simulations relies on understanding not only the theoretical aspects of patient care but also the practical application of medical guidelines. The ability to recognize symptoms, evaluate risk factors, and create personalized treatment plans are critical skills. These elements are central to achieving a high score and developing the confidence necessary to manage real-world patients effectively.
Students who approach these challenges with a structured, methodical approach will be better equipped to navigate complex cases. It’s important to focus on each patient’s unique needs, continually updating care plans based on evolving symptoms and feedback. This approach mirrors the demands of actual clinical practice, where adaptability and continuous learning are key to providing the best possible care.
Understanding Hypertension in Shadow Health
Chronic cardiovascular conditions are among the most common health challenges faced by patients, requiring healthcare providers to have a deep understanding of the underlying causes, symptoms, and management strategies. Effective care for individuals with elevated blood pressure involves not only identifying the key risk factors but also implementing appropriate interventions to prevent complications. This section explores the essential aspects of dealing with high blood pressure in clinical simulations, offering insights into best practices for patient assessment and management.
Recognizing Risk Factors
Identifying patients at risk for high blood pressure is the first step in providing effective care. Key factors such as age, lifestyle choices, and family history can increase the likelihood of developing this condition. By carefully evaluating these elements, healthcare providers can make informed decisions about further testing and treatment options. Regular monitoring of a patient’s blood pressure levels is crucial to track changes and adjust care plans as needed.
Effective Management Techniques
Managing high blood pressure involves a combination of lifestyle modifications, medications, and ongoing patient education. Encouraging healthier habits such as improved diet, regular exercise, and stress management can significantly impact blood pressure levels. In some cases, medications may be necessary to help control the condition and prevent long-term complications like heart disease or stroke. By taking a personalized approach, healthcare providers can help patients manage their condition and improve their overall well-being.
Key Symptoms of Type 2 Diabetes
Recognizing the early indicators of this chronic metabolic condition is crucial for effective intervention and management. The symptoms of this condition often develop gradually, which can make it challenging for patients to identify them without proper monitoring. Early detection is essential, as it allows for timely treatment and the prevention of complications associated with poor blood sugar regulation.
| Symptom | Description |
|---|---|
| Increased Thirst | Excessive thirst or dry mouth is a common symptom due to high blood sugar levels, leading to frequent urination and dehydration. |
| Frequent Urination | High blood glucose levels cause the kidneys to work harder to filter and absorb the excess sugar, resulting in more frequent urination. |
| Fatigue | Feeling unusually tired or weak is common, as the body’s cells are unable to effectively use glucose for energy. |
| Blurred Vision | High blood sugar can lead to fluid changes in the eyes, causing temporary blurred vision. |
| Slow Healing of Wounds | When blood sugar levels are consistently high, the body’s ability to heal and fight infections is impaired, leading to slower recovery. |
Awareness of these symptoms is vital, as timely action can help manage the condition effectively and prevent further complications. Regular screenings and patient education play a key role in early diagnosis and treatment. By understanding these warning signs, healthcare professionals can provide better care and improve patient outcomes.
Effective Management of Hypertension
Managing elevated blood pressure requires a comprehensive approach that addresses both lifestyle changes and, when necessary, medical intervention. Long-term control of this condition is crucial for preventing complications like heart disease, stroke, and kidney failure. The goal is to normalize blood pressure levels and reduce the strain on vital organs, which can be achieved through a combination of habits, treatments, and regular monitoring.
| Approach | Description |
|---|---|
| Dietary Adjustments | A low-sodium, heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins can help lower blood pressure. |
| Regular Exercise | Engaging in physical activity, such as brisk walking or swimming, for at least 30 minutes a day can significantly improve cardiovascular health. |
| Weight Management | Maintaining a healthy weight helps reduce the pressure on the heart and blood vessels, lowering the overall risk of complications. |
| Stress Reduction | Chronic stress can contribute to elevated blood pressure. Techniques such as meditation, yoga, or deep breathing exercises can help alleviate tension. |
| Medications | For patients unable to manage their condition through lifestyle changes alone, antihypertensive medications are prescribed to control blood pressure. |
By adopting these strategies, patients can successfully manage their condition and reduce the risk of long-term health complications. Regular check-ups with healthcare providers are essential to ensure that treatment plans are effective and adjusted as needed over time.
Common Challenges in Diabetes Care
Managing chronic metabolic conditions can be a complex task, especially when it comes to balancing daily treatment routines with long-term health goals. For patients dealing with blood sugar irregularities, maintaining stable glucose levels often requires constant attention, lifestyle adjustments, and monitoring. Healthcare providers face several challenges in offering comprehensive care that is both effective and sustainable for patients over time.
Patient Adherence to Treatment Plans
One of the most significant hurdles in managing chronic conditions is ensuring patient adherence to prescribed treatment regimens. This includes taking medications as directed, following dietary guidelines, and regularly monitoring blood glucose levels. Lack of motivation, misunderstanding of the condition, or challenges in daily routines can hinder a patient’s ability to consistently follow through with their care plan.
Managing Complications and Co-morbidities
Patients often experience a range of complications alongside their primary condition, including heart disease, kidney dysfunction, or nerve damage. These additional health issues can complicate the management process, as treatment needs to be tailored to address multiple conditions simultaneously. Careful coordination between healthcare providers is essential to avoid potential drug interactions and ensure the overall well-being of the patient.
By understanding these challenges, healthcare providers can offer more personalized care and better support patients in managing their conditions effectively. Communication, education, and continuous monitoring are key to overcoming these obstacles and improving long-term health outcomes.
Approaching the Shadow Health Exam
Preparing for virtual clinical assessments requires a strategic approach, where students need to effectively apply their medical knowledge in a simulated patient environment. Success in these simulations relies not only on theoretical understanding but also on the ability to make decisions quickly and accurately under pressure. With a clear strategy, students can navigate through complex scenarios while demonstrating their diagnostic and problem-solving skills.
| Preparation Strategy | Key Focus Areas |
|---|---|
| Review Patient History | Carefully analyze the patient’s background to understand potential risk factors and prior conditions. |
| Understand Symptoms | Identify key indicators that point to specific conditions, ensuring accurate diagnosis. |
| Formulate Treatment Plans | Develop a personalized care plan that includes interventions, lifestyle changes, and medication when necessary. |
| Prioritize Communication | Engage the patient with clear, empathetic communication to gather necessary information and provide reassurance. |
| Stay Calm Under Pressure | Manage time effectively and make decisions confidently, even when faced with challenging scenarios. |
By focusing on these key areas, students can ensure they approach these assessments with confidence and clarity. With each case requiring a different set of skills, thorough preparation is essential to demonstrating proficiency and securing a successful outcome in the virtual patient environment.
Assessing Blood Pressure in Patients
Accurately evaluating a patient’s blood pressure is essential in diagnosing and managing various health conditions. Proper assessment helps healthcare professionals understand the pressure exerted on the walls of the arteries during heartbeats and at rest. This simple yet critical measurement provides insight into cardiovascular health and can indicate the presence of potential complications. A thorough approach to this process ensures that patients receive the correct treatment and preventive care.
- Ensure the patient is seated comfortably and relaxed for at least five minutes before taking a measurement.
- Position the arm at heart level, with the cuff wrapped snugly around the upper arm, ensuring it is not too tight or loose.
- Use the appropriate cuff size for the patient’s arm to get an accurate reading.
- Inflate the cuff to the recommended pressure and gradually release it while listening for the systolic and diastolic pressures using a stethoscope.
- Repeat the measurement at least twice, if necessary, to confirm accuracy, particularly if the initial readings are high or inconsistent.
Proper technique and consistency are crucial when measuring blood pressure. Inaccurate readings can lead to incorrect diagnosis and improper treatment. Regular monitoring and an understanding of how to interpret results can greatly improve patient outcomes and guide medical decisions.
Identifying Risk Factors for Diabetes
Recognizing the key risk factors for chronic conditions related to poor blood sugar regulation is crucial for early intervention and prevention. A variety of factors can contribute to the development of these conditions, many of which are preventable or manageable with appropriate lifestyle changes. Identifying these risk factors allows healthcare professionals to assess a patient’s likelihood of developing complications and to provide targeted care strategies.
Genetic and Lifestyle Factors
Several genetic predispositions, combined with lifestyle choices, significantly influence the risk of developing blood sugar imbalances. Understanding these elements helps in designing personalized prevention plans.
- Family history of metabolic conditions or cardiovascular disease
- Being overweight or obese, particularly with excess abdominal fat
- Physical inactivity and a sedentary lifestyle
- Unhealthy eating habits, such as high consumption of sugary and processed foods
Health Conditions and Demographics

In addition to lifestyle factors, certain pre-existing health conditions and demographic traits can increase the risk of developing chronic metabolic disorders.
- Age, particularly over the age of 45
- High cholesterol or elevated triglyceride levels
- High blood pressure or other cardiovascular risk factors
- Gestational conditions such as high blood sugar during pregnancy
By recognizing these risk factors early, healthcare providers can implement effective prevention strategies to reduce the likelihood of developing chronic conditions. Education, lifestyle changes, and regular screenings are vital components of proactive care.
Improving Patient Communication Skills
Effective communication with patients is a fundamental aspect of providing quality care. It not only helps in gathering accurate information but also plays a crucial role in building trust and improving patient outcomes. Healthcare professionals must develop the ability to listen actively, convey complex information in simple terms, and create an empathetic environment that encourages patients to share their concerns and follow treatment plans.
| Key Skills | Impact on Care |
|---|---|
| Active Listening | Encourages patients to feel heard and understood, leading to better rapport and more accurate information sharing. |
| Clear Explanation | Ensures patients fully understand their condition, treatment options, and the importance of following medical advice. |
| Empathy and Support | Creates a supportive environment, helping patients feel more comfortable in discussing sensitive issues and adhering to their care plan. |
| Non-Verbal Communication | Improves patient comfort and trust through appropriate body language and facial expressions. |
By improving these communication skills, healthcare providers can ensure that patients are more engaged in their care, leading to better compliance and healthier outcomes. Establishing open lines of communication is crucial in managing chronic conditions and preventing complications. It is important for practitioners to regularly assess and refine their communication techniques to foster a positive and effective patient-provider relationship.
Critical Thinking in Diabetes Management
Effective management of metabolic conditions requires a structured approach that incorporates critical thinking at every stage. Healthcare professionals must carefully assess patient data, interpret symptoms, and make informed decisions about treatment plans. By applying logical reasoning and evidence-based practices, practitioners can develop tailored interventions that improve patient outcomes and reduce the risk of complications.
- Analyze patient history to identify potential risk factors and previous medical conditions.
- Evaluate current symptoms and determine whether they align with common patterns of the condition.
- Consider the impact of lifestyle factors such as diet, exercise, and stress on the patient’s overall health.
- Incorporate the latest clinical guidelines and research to inform treatment decisions.
- Regularly reassess treatment plans based on patient feedback and ongoing monitoring results.
By cultivating critical thinking skills, healthcare providers are better equipped to make decisions that are in the best interest of their patients. This approach fosters comprehensive care that addresses not just the immediate concerns, but also long-term health goals, leading to more effective management of the condition.
Interpreting Lab Results in Shadow Health

Accurate interpretation of laboratory results is crucial for making informed decisions about patient care. Lab tests provide valuable insights into the patient’s condition, helping healthcare providers identify potential risks, diagnose issues, and track the effectiveness of treatment plans. A clear understanding of the results allows for timely interventions and tailored care strategies to improve patient outcomes.
Key Factors to Consider
When interpreting lab results, several factors must be taken into account to ensure accurate conclusions. The following elements are vital for making proper assessments:
- Patient history and current symptoms: Understand how lab results correlate with the patient’s overall health and current complaints.
- Test accuracy and conditions: Ensure that the tests were conducted under proper conditions and that the results are reliable.
- Normal reference ranges: Familiarize yourself with the standard reference ranges for each test to recognize abnormalities.
- Multiple test results: Assess multiple lab results together to form a comprehensive picture of the patient’s health.
Common Lab Results in Patient Management
Some lab results provide essential information that directly influences treatment decisions. Healthcare providers must know how to interpret these tests to create effective care plans.
- Blood Glucose Levels: Elevated glucose levels may indicate poor regulation, necessitating lifestyle changes or medication adjustments.
- Cholesterol and Lipid Profiles: Abnormal lipid levels can increase the risk of cardiovascular complications, affecting treatment choices.
- Kidney Function Tests: These tests help identify complications such as kidney damage, which can affect overall treatment strategy.
- Blood Pressure Readings: Consistent elevated levels can signal the need for more intensive management to prevent other health issues.
Interpreting lab results requires both technical knowledge and clinical experience. By carefully evaluating the data, healthcare professionals can enhance patient care, reduce risks, and achieve better health outcomes. Regular training and practice are essential to stay up-to-date with evolving testing methods and interpretation techniques.
Understanding the Role of Medications
Medications play a crucial part in managing chronic conditions and preventing complications. By targeting specific pathways in the body, they can help control symptoms, stabilize vital functions, and reduce the risk of long-term health issues. It’s essential for healthcare providers to understand the different classes of drugs, their mechanisms, and how they interact with other treatments to offer the best care possible for patients.
Types of Medications Commonly Used
Several categories of drugs are commonly prescribed to manage chronic illnesses. Each class targets different aspects of the condition, and it’s important to tailor the treatment to the individual’s needs.
- Insulin: Helps regulate blood sugar levels in individuals who have difficulty producing or utilizing insulin effectively.
- Beta-blockers: Often used to lower blood pressure and reduce the strain on the heart.
- ACE Inhibitors: Help relax blood vessels, which can lower blood pressure and protect kidney function.
- Statins: Used to lower cholesterol levels and reduce the risk of cardiovascular complications.
- Diuretics: Help reduce excess fluid in the body, often used to manage blood pressure and swelling.
Monitoring and Adjusting Medication
While medications are essential for managing chronic conditions, it’s equally important to regularly monitor their effectiveness and make adjustments as needed. Factors such as changes in a patient’s lifestyle, progression of the condition, or new research findings may necessitate altering the medication regimen.
- Regular check-ups: Ensure that the patient’s condition is being managed effectively, and adjust dosages or medications as necessary.
- Patient feedback: Consider any side effects or challenges the patient may be experiencing with their medication.
- Lab results: Monitor lab tests to assess the effectiveness and safety of the medications being prescribed.
Proper medication management can significantly improve quality of life and prevent serious complications. By understanding the role of each drug, healthcare providers can ensure that patients receive the most appropriate treatment for their condition.
Creating Care Plans for Hypertension
Developing an effective care plan is essential for managing chronic conditions that impact cardiovascular health. A well-structured care plan helps healthcare providers monitor symptoms, reduce risks, and improve overall patient well-being. The process involves assessing individual needs, setting achievable goals, and outlining interventions to address both the medical and lifestyle factors that contribute to the condition.
Key Components of a Care Plan
A comprehensive care plan typically includes several key elements aimed at controlling and improving the patient’s health. These components address various aspects of the condition and ensure a holistic approach to treatment.
- Assessment: Start by evaluating the patient’s current health status, including their medical history, risk factors, and any existing complications.
- Goals: Define clear, measurable objectives, such as reducing blood pressure, improving medication adherence, or promoting heart health.
- Interventions: Choose appropriate treatments and interventions, such as medications, lifestyle modifications (diet, exercise), and patient education.
- Follow-up: Establish a schedule for regular check-ups and monitoring to ensure progress and make necessary adjustments to the plan.
Patient Involvement in the Care Plan
Effective care plans are collaborative efforts that involve the patient in their own health management. Encouraging patients to actively participate in their care increases the likelihood of successful outcomes. Key areas of patient involvement include:
- Education: Providing information on how the condition impacts their health and the importance of adhering to the prescribed treatment regimen.
- Self-monitoring: Teaching patients how to monitor their vital signs, such as blood pressure, and track any symptoms that may arise.
- Behavioral changes: Supporting patients in making necessary lifestyle changes, such as increasing physical activity and improving dietary habits.
By creating a tailored care plan that addresses both medical and personal factors, healthcare providers can help individuals better manage their health, reduce complications, and enhance their overall quality of life.
How to Handle Complications in Diabetes
Managing chronic conditions often involves not only treating the core symptoms but also addressing any secondary issues that may arise over time. Complications can occur due to prolonged uncontrolled levels, affecting various organs and systems. Promptly identifying and treating these issues is crucial to prevent further damage and improve quality of life.
Common Complications and Their Management
While complications can vary depending on the individual, there are several common issues that many people face. Addressing these concerns proactively is key to effective long-term management.
- Cardiovascular Problems: Individuals with chronic conditions may be at higher risk for heart disease. Regular monitoring of cholesterol, blood pressure, and heart health is essential, along with medication and lifestyle changes such as improved diet and physical activity.
- Nerve Damage: Neuropathy can occur, causing pain, numbness, or tingling, particularly in the feet and hands. Managing blood sugar levels, regular foot care, and specific treatments for nerve pain can help alleviate symptoms.
- Kidney Issues: Kidney function may deteriorate over time. Early detection through routine tests for protein in the urine and regular kidney function assessments can help slow progression. Adequate hydration, controlled blood pressure, and medication can support kidney health.
- Vision Impairment: Eye problems such as retinopathy may develop. Regular eye exams, controlling blood sugar levels, and managing blood pressure can help reduce the risk of severe vision loss.
- Wound Healing Problems: Wounds may take longer to heal. Ensuring good blood circulation, proper wound care, and monitoring for signs of infection can aid in faster recovery and prevent further complications.
Preventative Measures
Preventing complications is a vital part of managing chronic conditions. Taking steps to minimize risk factors and adhere to prescribed care plans can help reduce the chances of complications arising.
- Regular Monitoring: Frequent check-ups and testing for glucose levels, kidney function, and cholesterol are essential to stay ahead of potential issues.
- Lifestyle Adjustments: Healthy eating, regular physical activity, maintaining a healthy weight, and managing stress can significantly lower the risk of complications.
- Medication Adherence: Consistently following prescribed treatments is critical to keeping the condition in check and avoiding complications.
By staying vigilant and taking a comprehensive approach to care, individuals can manage the risks associated with their condition and prevent long-term damage. Collaborating with healthcare providers and making necessary lifestyle changes are integral to ensuring optimal outcomes.
Guidelines for Diet and Lifestyle Changes
Making sustainable changes to daily habits is essential for managing chronic conditions effectively. Modifying diet, exercise routines, and other aspects of life can significantly improve overall health, control symptoms, and prevent complications. A balanced approach that incorporates healthier food choices, regular physical activity, and mental well-being strategies can help in achieving long-term success.
Dietary Recommendations
One of the most important aspects of managing a chronic condition is ensuring proper nutrition. A well-rounded, nutrient-dense diet helps maintain stable blood levels and supports overall bodily functions. Here are some key guidelines:
- Focus on Whole Grains: Include foods like brown rice, whole wheat, oats, and quinoa. These provide fiber and can help regulate blood sugar levels.
- Eat Plenty of Vegetables: Aim for a variety of colorful vegetables. They are high in vitamins, minerals, and antioxidants that can support overall health.
- Limit Processed Foods: Reduce the intake of sugary snacks, refined carbohydrates, and processed meats. These can cause spikes in blood sugar and worsen overall health.
- Incorporate Lean Proteins: Opt for sources such as fish, chicken, beans, or tofu. These proteins help maintain muscle mass without increasing unhealthy fats.
- Healthy Fats: Include healthy fats from sources like avocados, olive oil, nuts, and seeds. These fats support heart health and overall well-being.
- Watch Portion Sizes: Eating in moderation is crucial. Overeating, even healthy foods, can lead to weight gain and blood sugar instability.
Exercise and Physical Activity

Regular physical activity plays a crucial role in managing chronic conditions. Exercise can help control blood sugar levels, reduce stress, improve cardiovascular health, and promote overall fitness. Here are some tips for incorporating exercise into your routine:
- Consistency is Key: Aim for at least 30 minutes of moderate exercise most days of the week. Activities like walking, swimming, or cycling are great options.
- Strength Training: In addition to aerobic exercise, include strength training to build muscle mass and enhance metabolism. Bodyweight exercises, resistance bands, or weight lifting can be effective.
- Flexibility and Balance: Incorporate stretching and balance exercises to improve flexibility, reduce stress, and lower the risk of falls.
- Stay Active Throughout the Day: Find ways to stay moving, such as taking the stairs instead of the elevator or walking around during breaks. Small changes can add up.
Mental Health and Stress Management
Managing stress and maintaining mental well-being are just as important as physical health. Chronic stress can worsen symptoms and impact overall quality of life. Here are some practices to consider:
- Mindfulness Practices: Engage in mindfulness techniq
Utilizing Resources for Comprehensive Patient Assessments
To perform thorough evaluations and improve clinical decision-making, utilizing available resources effectively is essential. These tools provide valuable insights, ensuring that practitioners are well-prepared to assess, diagnose, and manage patient conditions. A wide range of materials, including online platforms, textbooks, and professional guidelines, can support both learning and practical application in medical settings.
Online Platforms and Interactive Simulations

Interactive tools and simulations are incredibly helpful for refining clinical skills. They offer a hands-on approach to learning, allowing practitioners to apply theoretical knowledge in a controlled, risk-free environment. By engaging with virtual patient scenarios, users can practice making real-time decisions and observe outcomes based on their actions.
- Virtual Case Studies: These allow for the exploration of various patient conditions, providing scenarios to assess and diagnose based on symptoms, history, and lab results.
- Clinical Decision Support Tools: These resources guide healthcare professionals through diagnostic processes, offering evidence-based recommendations and reminders to ensure accuracy in patient care.
- Simulation Platforms: Simulated patient interactions provide opportunities for practicing communication, assessment, and diagnostic skills in a virtual setting, helping refine approach and technique.
Textbooks, Research Articles, and Professional Guidelines
In addition to digital tools, traditional resources such as textbooks, peer-reviewed research, and established clinical guidelines remain indispensable for comprehensive knowledge and evidence-based practices. These materials ensure that the care provided aligns with the latest scientific research and professional standards.
- Medical Textbooks: Standard reference books provide in-depth knowledge of various conditions, treatment options, and case studies to guide practice.
- Peer-Reviewed Journals: Staying up-to-date with the latest research articles helps keep practice evidence-based, ensuring the application of the most current medical findings.
- Clinical Protocols and Guidelines: These resources provide structured, standardized approaches to diagnosing and managing a wide array of conditions, ensuring consistency and high-quality care.
By integrating these tools into daily practice, healthcare professionals can enhance their diagnostic capabilities, improve patient outcomes, and gain confidence in their clinical decision-making skills.
Developing Confidence in Exam Responses
Building self-assurance when responding to assessments is crucial for effective learning and performance. Confidence stems from a strong foundation of knowledge, experience, and preparation. By adopting strategic methods, individuals can improve their ability to answer questions with clarity, precision, and confidence, leading to better outcomes in evaluations.
Thorough Preparation and Practice
The first step in enhancing confidence is consistent preparation. Regularly reviewing course materials, textbooks, and relevant guidelines ensures a deep understanding of the topics at hand. Practice plays a key role in reinforcing this knowledge. By engaging in mock scenarios, quizzes, and self-assessments, individuals can familiarize themselves with the types of questions they may encounter, as well as refine their responses.
- Mock Quizzes: Taking practice tests under timed conditions helps simulate real assessment environments, aiding in better time management and response accuracy.
- Case Studies: Analyzing case studies and discussing them with peers or mentors enhances critical thinking and decision-making abilities.
- Reviewing Feedback: Reflecting on past evaluations and incorporating constructive feedback allows for continuous improvement and knowledge refinement.
Effective Answer Structuring
How answers are structured plays a significant role in conveying knowledge clearly and confidently. A well-organized response demonstrates a logical thought process and ensures that important points are not overlooked. It is important to break down answers into manageable sections, focusing on key concepts and supporting them with relevant details.
- Introduction: Start with a clear, concise statement addressing the core of the question.
- Main Body: Provide detailed explanations, using examples and evidence to support your points.
- Conclusion: Summarize the key points, reinforcing your main argument or solution.
By integrating these strategies, individuals can boost their self-assurance, enhance their performance in evaluations, and achieve success in their academic and professional journeys.
Tips for Success in Clinical Simulations
Clinical simulations provide an opportunity to apply theoretical knowledge in a controlled, real-world environment, helping students and professionals refine their skills. Success in these simulated settings hinges on preparation, clear communication, and critical thinking. By following practical strategies, individuals can navigate simulations confidently and achieve positive outcomes.
Preparation is Key
Thorough preparation is crucial to performing well in clinical simulations. Familiarizing yourself with the case details, patient background, and expected outcomes allows you to approach the scenario with a clear mind. Review any relevant protocols or guidelines before the simulation to ensure you can apply them accurately in practice.
- Study the Scenario: Understand the key components of the case, including patient history, symptoms, and potential diagnoses.
- Know Your Tools: Be comfortable with the medical equipment and technology you’ll be using during the simulation.
- Practice Key Skills: Regularly practice hands-on skills, such as taking vital signs or administering medications, to build proficiency.
Effective Communication and Teamwork
Clear communication is vital during clinical simulations, as it ensures that all team members are aligned and able to make informed decisions. Whether you’re leading the simulation or participating as part of a team, sharing information effectively is essential. Be open to receiving feedback, ask questions when needed, and ensure that instructions are understood by everyone involved.
- Active Listening: Pay attention to the information shared by the patient or team members, as it may influence your decisions.
- Ask Clarifying Questions: Don’t hesitate to ask questions if you’re unsure about certain aspects of the case.
- Use Clear Terminology: Communicate your thoughts and actions using precise, professional language to avoid misunderstandings.
By mastering these strategies, individuals can enhance their performance in clinical simulations, build confidence in their abilities, and improve their overall clinical competence.