
Accurate documentation plays a critical role in the healthcare process, ensuring that patient information is properly recorded and easily accessible for medical professionals. Proper documentation not only improves communication between providers but also helps track patient progress over time. In medical settings, one effective method of recording patient information is through a structured format that covers various aspects of a patient’s health history, physical findings, and future care plans.
Within this structure, specific sections are dedicated to capturing different types of data, including the patient’s reported symptoms, observed physical signs, clinical assessments, and recommended actions. This method of documentation is essential for maintaining a comprehensive patient record, enhancing both the quality of care provided and the continuity of treatment. In this article, we will explore the key components of this type of clinical record, highlighting best practices for creating accurate and useful entries that support effective patient management.
Understanding the Health Assessment Documentation
In clinical practice, accurate and organized patient records are vital for providing high-quality care. This documentation method is designed to systematically capture key aspects of a patient’s health, including subjective complaints, objective findings, clinical evaluations, and treatment plans. By maintaining a structured approach, healthcare providers can ensure that all relevant information is readily available and can be easily referenced during follow-up appointments or in emergencies.
The method emphasizes clear and concise documentation that aids in understanding a patient’s health status over time. Each section serves a specific purpose, helping medical professionals assess a patient’s condition, identify potential issues, and formulate a personalized care plan. This approach not only supports effective communication but also contributes to improved health outcomes by enabling better tracking and continuity of care.
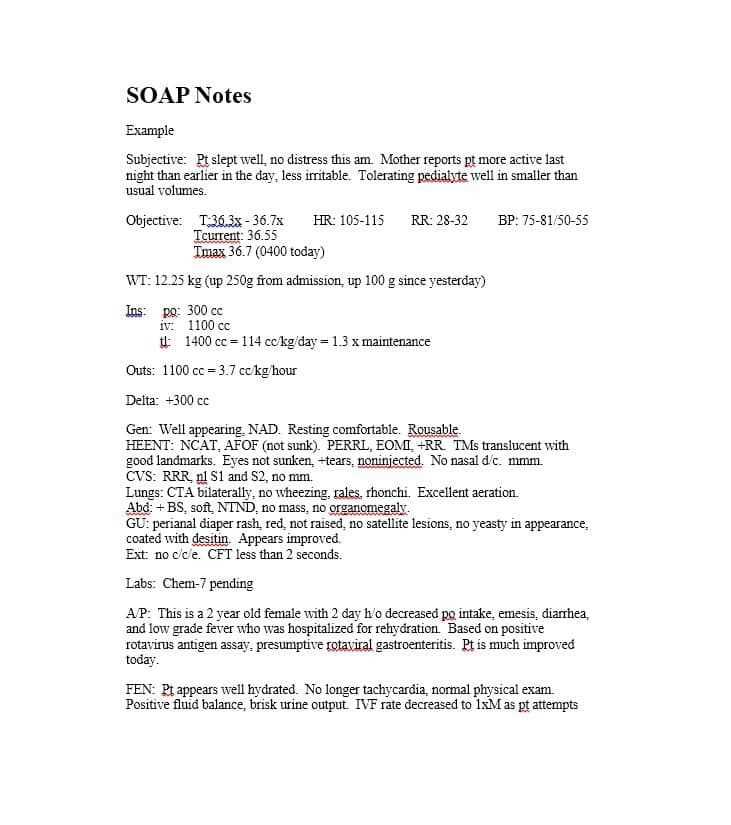
What is a SOAP Note
This documentation format is widely used by healthcare providers to record important details about a patient’s health status during medical consultations. It is a structured approach that helps capture the patient’s reported symptoms, physical findings, diagnosis, and care plan in a concise manner. By following a specific framework, this method ensures that key information is not overlooked and that all necessary elements of patient care are addressed.
The structure of this system is divided into four key sections:
- Subjective: This section includes the patient’s personal account of their symptoms, medical history, and any concerns they wish to express.
- Objective: Here, the healthcare provider records their observations, physical examination results, and diagnostic findings.
- Assessment: Based on the subjective and objective information, the clinician forms a clinical judgment, identifying potential health issues or confirming a diagnosis.
- Plan: This section outlines the recommended course of action, including treatment options, follow-up appointments, or further diagnostic tests.
Using this method ensures that all relevant information is documented in an organized way, which not only facilitates efficient patient care but also provides a clear reference for future consultations.
Key Components of the SOAP Note
This method of documentation is structured into distinct sections, each serving a specific purpose in capturing important patient information. These components allow healthcare providers to gather comprehensive data, assess patient conditions, and develop a clear plan for care. The structure ensures consistency in documenting critical aspects of a patient’s health, facilitating communication and continuity in treatment.
The four primary sections of this framework are as follows:
- Subjective: This section records the patient’s own account of their symptoms, concerns, and medical history. It may include information about pain levels, lifestyle factors, or recent changes in health.
- Objective: Here, the healthcare provider documents measurable data collected through physical examination, lab results, vital signs, and imaging studies. This section provides concrete evidence to support the clinical assessment.
- Assessment: Based on the information gathered, the clinician forms a diagnosis or identifies potential health issues. This section reflects the provider’s clinical judgment, often noting the severity or progression of the patient’s condition.
- Plan: The plan outlines the next steps in managing the patient’s health, which may include prescriptions, further testing, referrals, lifestyle recommendations, or follow-up visits.
Each section plays a crucial role in ensuring that the patient’s health is thoroughly documented and that an effective, individualized care plan is developed.
Subjective Section: Patient History

The subjective section of a patient record is focused on gathering the individual’s personal account of their health. This section is essential for understanding the patient’s symptoms, concerns, and medical background, providing a foundation for further clinical evaluation. It is the first step in building a comprehensive picture of the patient’s overall health status, enabling healthcare providers to tailor their assessments and decisions accordingly.
Types of Information Collected
In this section, the following key elements are typically documented:
| Category | Description |
|---|---|
| Chief Complaint | The primary reason the patient is seeking care, usually described in their own words. |
| Medical History | Details about past illnesses, surgeries, chronic conditions, and any ongoing treatments. |
| Family History | Relevant hereditary factors, including conditions that may run in the patient’s family. |
| Social History | Information about lifestyle, including smoking, alcohol use, exercise, diet, and occupational factors. |
| Review of Systems | A comprehensive overview of other body systems, looking for symptoms that the patient may not have mentioned yet. |
Importance of Accuracy in Patient History
Collecting accurate and thorough information in the subjective section is critical for establishing a proper diagnosis. The details provided by the patient can often guide further testing or influence the approach to treatment. It is important for healthcare providers to listen carefully, ask follow-up questions, and ensure that all relevant factors are documented clearly and comprehensively.
Objective Data Collection in SOAP Notes
The objective section of a patient record focuses on factual, measurable information collected through direct observation, examination, and diagnostic tests. This section provides concrete data that complements the patient’s subjective report, allowing healthcare providers to assess the situation with greater clarity and precision. It includes vital signs, physical findings, lab results, imaging, and other relevant tests that contribute to an objective understanding of the patient’s condition.
Key elements typically documented in this section include:
- Vital Signs: These include blood pressure, heart rate, temperature, respiratory rate, and oxygen saturation levels.
- Physical Examination: A detailed assessment of the patient’s body, which may involve inspections, palpations, auscultation, and percussion.
- Laboratory Results: Test results such as blood work, urine analysis, or cultures that provide insight into the patient’s internal health.
- Diagnostic Imaging: Information from imaging tests like X-rays, MRIs, or ultrasounds, which help identify physical abnormalities or confirm diagnoses.
By collecting objective data, healthcare providers can document findings that are not influenced by patient perception or subjectivity. This data is crucial for forming a clinical assessment and guiding the development of an appropriate care plan. Accurate documentation of objective information ensures that decisions are based on reliable evidence and enhances the quality of care provided.
Assessment in a Health Evaluation
The assessment section of a patient’s record plays a pivotal role in synthesizing the information gathered from both the patient’s report and the objective data collected during the visit. It reflects the clinician’s professional judgment based on all available facts, aiming to determine the patient’s overall health status, identify any concerns, and outline the next steps in care. This section is crucial for guiding treatment decisions and providing a clear direction for ongoing management.
Clinical Evaluation and Diagnosis
In this stage, the healthcare provider reviews all the subjective and objective data to identify any health conditions or risks. This may involve confirming a diagnosis, noting the severity or progression of existing conditions, or identifying areas that require further investigation. The assessment is not limited to just identifying problems; it also includes evaluating the patient’s risk factors, overall well-being, and the effectiveness of any ongoing treatments.
Formulating a Treatment Strategy
Based on the clinical evaluation, the provider can begin to formulate a tailored treatment plan. This may involve recommending lifestyle changes, initiating therapies or medications, or scheduling follow-up appointments to monitor progress. The assessment also helps in determining whether additional tests are needed to refine the diagnosis or assess other aspects of the patient’s health.
Creating a Plan for Patient Care
After assessing a patient’s health status, the next critical step is to develop a comprehensive care plan tailored to their needs. This plan outlines the actions that will be taken to address identified health issues, prevent future complications, and enhance overall well-being. A well-structured care plan not only guides treatment but also provides clear instructions for follow-up, monitoring, and adjustments as needed.
The care plan typically includes a combination of immediate interventions, long-term strategies, and preventative measures. It may involve prescribing medications, recommending lifestyle changes, scheduling additional tests, or referring the patient to specialists. The plan should also consider the patient’s preferences, health goals, and any potential barriers to following the prescribed recommendations.
Effective care planning fosters collaboration between the patient and healthcare provider, ensuring that both parties are aligned on treatment goals and expectations. By prioritizing individualized care, healthcare professionals can improve patient outcomes and enhance the overall quality of care provided.
SOAP Note Best Practices for Documentation
Accurate and efficient documentation is essential in healthcare, ensuring that patient information is clearly recorded and easily accessible. By adhering to best practices for documentation, healthcare providers can maintain high-quality records, enhance communication among professionals, and support better patient outcomes. Proper documentation also plays a critical role in legal protection and regulatory compliance.
Here are several best practices to follow when documenting patient information:
- Be Clear and Concise: Ensure that each section is well-organized and that all information is relevant to the patient’s condition. Avoid unnecessary details or jargon that may confuse future readers.
- Use Objective Language: Stick to measurable, factual information, especially in the objective section. Avoid subjective or biased terms that could be misinterpreted.
- Follow a Standardized Format: Consistency is key to ensuring that records are easy to follow. Use a clear, uniform structure for each section to facilitate quick access to important details.
- Document in Real Time: Record patient information as soon as possible after the consultation. This reduces the risk of errors and omissions.
- Include Relevant Details: Ensure that all pertinent findings are included in the documentation, from medical history to current symptoms and any diagnostic results.
- Protect Patient Privacy: Always follow confidentiality guidelines when documenting sensitive information. Adhere to legal and ethical standards for patient privacy.
By following these practices, healthcare providers can ensure that their documentation supports the delivery of effective care, fosters better collaboration, and meets all professional standards.
Common Challenges in Health Assessments
Healthcare providers often face a range of challenges when conducting routine health evaluations. These challenges can stem from various factors, such as patient anxiety, incomplete medical histories, or difficulty in communication. Addressing these issues is vital for ensuring that the assessment is thorough, accurate, and effective in identifying potential health risks or concerns.
Some of the most common challenges include:
- Patient Reluctance: Many patients may feel uncomfortable discussing sensitive health topics, leading to incomplete or inaccurate information. This can be particularly problematic when addressing personal or reproductive health matters.
- Language Barriers: Communication difficulties can arise if the patient and healthcare provider do not speak the same language or if there is a lack of understanding of medical terminology, making it harder to gather accurate information.
- Inconsistent Medical Histories: Patients may not always recall or disclose important details about their past health conditions, which can lead to gaps in understanding the full scope of their medical background.
- Time Constraints: Healthcare providers may have limited time to conduct a comprehensive evaluation, potentially leading to rushed appointments and missed symptoms or concerns.
- Fear of Judgment: Patients may avoid seeking care or be hesitant to share details due to fear of judgment or embarrassment, particularly when discussing lifestyle choices or sexual health.
- Lack of Follow-Up: Without proper follow-up, important findings from the assessment may not be adequately addressed, leading to missed opportunities for early intervention or treatment.
Overcoming these challenges requires patience, clear communication, and a compassionate approach. By fostering a comfortable environment and being proactive in addressing these barriers, healthcare providers can improve the quality of the evaluation and ensure more accurate diagnoses and better patient outcomes.
Tips for Accurate SOAP Note Writing
Clear and precise documentation is crucial for providing high-quality patient care. Well-written clinical records help ensure that important details are captured, facilitating better decision-making and effective communication among healthcare professionals. To achieve accuracy and clarity, it is essential to follow best practices when documenting patient information.
Here are some key tips to improve the quality and accuracy of clinical documentation:
- Be Specific and Detailed: Ensure that all findings, whether subjective or objective, are recorded with sufficient detail. Avoid vague descriptions and provide precise measurements or observations whenever possible.
- Use Standardized Terminology: Use consistent and widely accepted medical terminology to avoid confusion. This ensures that all members of the healthcare team can interpret the documentation accurately.
- Avoid Ambiguity: Keep language simple and direct. Avoid using terms that could be interpreted in multiple ways or that are not clinically relevant to the patient’s condition.
- Record Information in Real-Time: Document patient information as soon as possible during or after the consultation to reduce the chances of forgetting important details and to maintain accuracy.
- Focus on Objectivity: Stick to the facts, especially when documenting clinical findings. Avoid personal opinions or assumptions, and ensure that any subjective information is clearly attributed to the patient’s report.
- Review and Edit: Always double-check your documentation for completeness and clarity before finalizing it. Look for any missed details, grammatical errors, or inconsistencies that could impact the quality of the record.
- Be Concise: While it’s important to be thorough, it’s also crucial to avoid unnecessary repetition. Keep sentences focused on the most relevant details to maintain readability and efficiency.
By following these tips, healthcare providers can ensure that their documentation is accurate, efficient, and contributes to improved patient care. Well-organized and precise records enhance the overall quality of healthcare delivery and support better clinical outcomes.
Importance of Patient Privacy and Consent
In healthcare, maintaining patient privacy and obtaining proper consent are fundamental principles that protect both the patient and healthcare provider. These practices ensure that sensitive personal and medical information is kept secure and that patients are fully informed and comfortable with the care they receive. Adhering to privacy laws and ethical guidelines is crucial for building trust and fostering a positive relationship between healthcare professionals and patients.
Patient privacy refers to safeguarding their medical and personal information, while consent involves ensuring that patients are aware of and agree to the treatments or procedures being performed. Both of these aspects are essential for providing ethical, legal, and respectful care.
Here are key reasons why privacy and consent are critical in healthcare:
- Trust Building: When patients feel that their information is protected and that their participation is voluntary, they are more likely to share important details that can improve their care.
- Legal Compliance: Healthcare providers must follow laws and regulations such as HIPAA (Health Insurance Portability and Accountability Act) to avoid legal consequences and maintain professional standards.
- Respect for Autonomy: Obtaining informed consent allows patients to make decisions about their healthcare, respecting their right to autonomy and involvement in their treatment choices.
- Protecting Sensitive Information: Maintaining confidentiality ensures that private data, such as medical history and personal circumstances, is not disclosed without permission, preventing harm or discrimination.
- Minimizing Risks: Proper consent helps to clarify the risks and benefits of any proposed treatments, allowing patients to make well-informed decisions and reducing the likelihood of misunderstandings or disputes.
- Professional Integrity: Following privacy and consent protocols reinforces the ethical standards of the healthcare profession, fostering a reputation of professionalism and reliability.
Ensuring patient privacy and obtaining informed consent are not just legal requirements–they are essential to providing high-quality, compassionate, and patient-centered care. These practices help protect the rights of individuals while supporting the effective delivery of healthcare services.
How to Include Preventative Care in SOAP Notes
Incorporating preventative care into clinical documentation is an essential part of promoting overall health and wellness. Preventative measures aim to reduce the risk of developing chronic conditions and improve long-term health outcomes. By effectively recording these practices, healthcare providers can ensure that patients receive the guidance they need to maintain and improve their health.
When documenting care plans, it’s crucial to include specific recommendations for preventive screenings, lifestyle modifications, immunizations, and education on health risks. The key is to make the information clear, actionable, and relevant to each individual patient’s needs.
Identifying Key Preventative Measures
Preventative care should be tailored to the patient’s age, gender, medical history, and current health status. The following are common preventative interventions that can be included in documentation:
- Screenings: Include any recommended screenings based on the patient’s age and health status, such as mammograms, cholesterol checks, and colonoscopies.
- Immunizations: Document any vaccines that are due or recommended, such as flu shots, HPV vaccines, or other age-appropriate immunizations.
- Lifestyle Changes: Provide guidance on healthy habits such as smoking cessation, exercise, and diet changes to reduce the risk of chronic diseases.
- Patient Education: Offer educational materials or resources to inform patients about the importance of preventative care and healthy living practices.
Documenting Preventative Measures in SOAP Format
When including preventative care in clinical records, the following approach can be used:
- Subjective: Include any relevant patient-reported concerns or questions regarding preventative measures. For example, if the patient asks about the need for a flu vaccine or a screening test.
- Objective: Document any physical exam findings related to the need for preventative interventions, such as weight, blood pressure, or lab results that indicate risk factors.
- Assessment: Note the patient’s overall health status and identify any potential risk factors that require preventative care, such as a family history of certain conditions.
- Plan: Clearly outline the recommended preventative care measures, such as scheduling screenings, administering vaccines, or providing lifestyle change recommendations.
By documenting preventative care thoroughly and consistently, healthcare providers help ensure that patients are proactive in maintaining their health, which can lead to early detection of health issues and a better quality of life.
SOAP Notes for Routine Health Screenings
Routine health screenings are essential tools for identifying potential health issues early and preventing serious conditions from developing. Including these screenings in patient records helps ensure that individuals receive the appropriate tests and follow-up care. Proper documentation of these screenings provides a clear history for healthcare providers, helping them track patients’ health over time and make informed decisions about their care.
When documenting routine screenings, it’s important to include details such as the type of screening, the patient’s risk factors, the results, and any follow-up actions or recommendations. This helps ensure that all necessary screenings are completed and any abnormal results are addressed promptly.
Here’s how to effectively document routine screenings in a clinical record:
- Subjective: Note any relevant patient-reported concerns, including family history or symptoms that may indicate the need for specific screenings. For example, if a patient expresses concern about a family history of cancer or heart disease, this may warrant related tests.
- Objective: Document physical examination findings, such as vital signs or other measurable factors, that may indicate the need for a screening. For instance, high blood pressure readings may lead to a recommendation for cardiovascular screenings.
- Assessment: Based on the patient’s history and exam findings, assess the patient’s risk and determine the appropriate screenings. This may involve evaluating age, gender, family history, lifestyle factors, and previous health screenings.
- Plan: List the recommended screenings, including any relevant tests (e.g., mammograms, cholesterol checks, colonoscopies). If any screenings are overdue or need to be rescheduled, ensure that these actions are clearly outlined for follow-up.
Effective documentation of routine health screenings ensures that patients receive the best possible care and helps healthcare providers stay on top of preventive measures. Accurate records help providers track progress, identify trends, and make well-informed decisions regarding future care.
Enhancing Patient Communication Through SOAP Notes
Clear and effective communication between healthcare providers and patients is crucial for delivering quality care. Well-documented patient records play a key role in bridging any gaps in understanding, providing a structured way for providers to relay important information about a patient’s condition, treatment plans, and follow-up steps. By capturing both subjective experiences and objective findings, healthcare professionals can ensure that patients are well-informed and engaged in their care journey.
One of the main benefits of structured documentation is that it allows for better continuity of care, especially when multiple providers are involved. SOAP notes, when properly used, can serve as a valuable tool for conveying important clinical details in a format that is easy for all team members to read and understand. This not only helps improve internal communication but also enhances interactions with patients, ensuring that they are aware of their current health status and any necessary next steps.
To enhance communication, it’s essential to focus on certain aspects during documentation:
| Section | Communication Enhancement |
|---|---|
| Subjective | Capture patient concerns, complaints, and history accurately to establish trust and ensure that the patient feels heard. This creates a foundation for addressing their specific needs. |
| Objective | Document measurable data like vital signs or lab results to provide concrete evidence of the patient’s condition. This can help patients understand their health status and follow through with recommendations. |
| Assessment | Clearly explain the healthcare provider’s clinical evaluation, which not only informs the patient about their condition but also helps them understand the rationale behind suggested treatments. |
| Plan | Outline clear, actionable steps that the patient needs to take. This provides a roadmap for what to expect next and sets expectations for follow-up, empowering patients to take control of their health. |
When SOAP notes are written with the goal of improving patient communication, they not only serve as a record of care but also as an essential tool for enhancing patient understanding and involvement. This fosters a collaborative relationship where patients are actively engaged in their treatment decisions, ultimately leading to better health outcomes.
Using SOAP Notes for Follow-up Visits
Follow-up visits are an essential part of patient care, offering an opportunity to assess progress, adjust treatment plans, and address any new concerns that may arise. Detailed and structured documentation is crucial during these visits, ensuring that all relevant information is captured and clearly communicated to both the patient and the healthcare team. A well-organized record can guide future decisions and help maintain continuity of care, particularly when patients are seeing multiple providers or specialists.
For follow-up visits, structured documentation serves multiple purposes. It not only provides a clear record of the patient’s status, but also allows healthcare providers to evaluate the effectiveness of previous interventions and make any necessary adjustments to the treatment plan. This approach fosters a continuous loop of care that is both responsive and personalized to the patient’s needs.
Key Elements to Include in Follow-up SOAP Documentation
During follow-up visits, the SOAP format remains a useful framework for organizing information. Each section can be tailored to track changes in the patient’s condition, adherence to previous recommendations, and any new symptoms or concerns.
| Section | Focus for Follow-up |
|---|---|
| Subjective | Capture the patient’s perspective on their progress since the last visit, including feedback on symptoms, medication side effects, and any lifestyle changes. This helps gauge whether the treatment plan is working as intended. |
| Objective | Record measurable data from physical exams, lab results, or imaging studies. This is important to document the patient’s objective health status and track improvements or any emerging issues. |
| Assessment | Offer a clinical evaluation based on the updated information from the subjective and objective sections. Assess whether the original diagnosis or treatment plan needs modification based on the patient’s progress. |
| Plan | Outline the next steps in the patient’s care, including follow-up appointments, new treatments, or changes to medications. Ensure the plan aligns with the patient’s current needs and goals for continued improvement. |
Tracking Progress Over Time
By consistently using a structured approach for follow-up visits, healthcare providers can effectively track patient progress over time. SOAP documentation serves as an ongoing record of each visit’s outcomes, helping identify patterns and long-term health trends. This continuity is critical for making well-informed decisions and improving patient care.
Improving Quality of Care with SOAP Documentation
Clear and organized patient records play a fundamental role in enhancing the quality of care provided. Accurate documentation ensures that all healthcare providers involved in a patient’s care are aligned, facilitating informed decision-making and continuity in treatment. By using a standardized format to record patient encounters, healthcare professionals can address concerns more effectively, ensure timely interventions, and improve overall patient outcomes.
Structured documentation allows for better tracking of a patient’s progress over time, enabling providers to assess whether current treatments are effective or if adjustments are needed. Furthermore, comprehensive records reduce the risk of medical errors, as all relevant details are captured in a systematic and easy-to-reference manner. This approach fosters a collaborative environment where patient care is optimized and well-coordinated.
Improved Patient Engagement
When healthcare providers maintain thorough and accessible documentation, patients are more likely to feel heard and understood. The clear communication of a patient’s health status and treatment plan ensures they remain actively involved in their care, leading to higher satisfaction and better adherence to prescribed therapies. By reviewing previous visit documentation, patients can track their own progress, which can increase motivation and foster trust in their healthcare team.
Enhanced Coordination Among Providers
With a standardized method for documenting patient visits, various healthcare providers can easily share information, leading to improved collaboration. Whether a patient is seeing multiple specialists or transitioning between different levels of care, detailed and accurate records ensure that each provider is aware of the patient’s current condition and care plan. This coordinated approach minimizes the risk of duplicating tests, conflicting treatments, or overlooked issues, all of which can impact patient safety and quality of care.
Efficiency and Continuity in Care
Effective documentation supports efficiency by making it easier for providers to quickly assess the patient’s health status and treatment history. This streamlining of information saves time, reduces redundancies, and helps healthcare teams prioritize patient needs. Additionally, when consistent documentation is used, there is a clear record of decisions made, tests ordered, and treatments provided, which ensures a smooth transition between visits and follow-up care, contributing to better long-term outcomes.