In the realm of healthcare, reflecting on fundamental beliefs and principles is essential for both personal and professional growth. This examination not only guides practitioners in their approach to patient care but also shapes their overall perspective on the responsibilities they carry. By exploring these core values, healthcare providers can enhance their understanding of human well-being and their role in promoting health.
Reflection and critical thinking play key roles in helping practitioners evaluate and refine their approach. These reflective processes encourage a deeper understanding of the ethical, social, and practical aspects of their work. Whether addressing challenges in patient interaction or navigating complex healthcare systems, a strong foundation of principles can make a significant difference.
Ultimately, this exploration is a continual journey, one that grows with experience and fosters a deeper connection between care providers and those they serve. As the field evolves, these guiding ideas remain a touchstone, ensuring that professionals stay focused on what truly matters in the practice of healthcare.
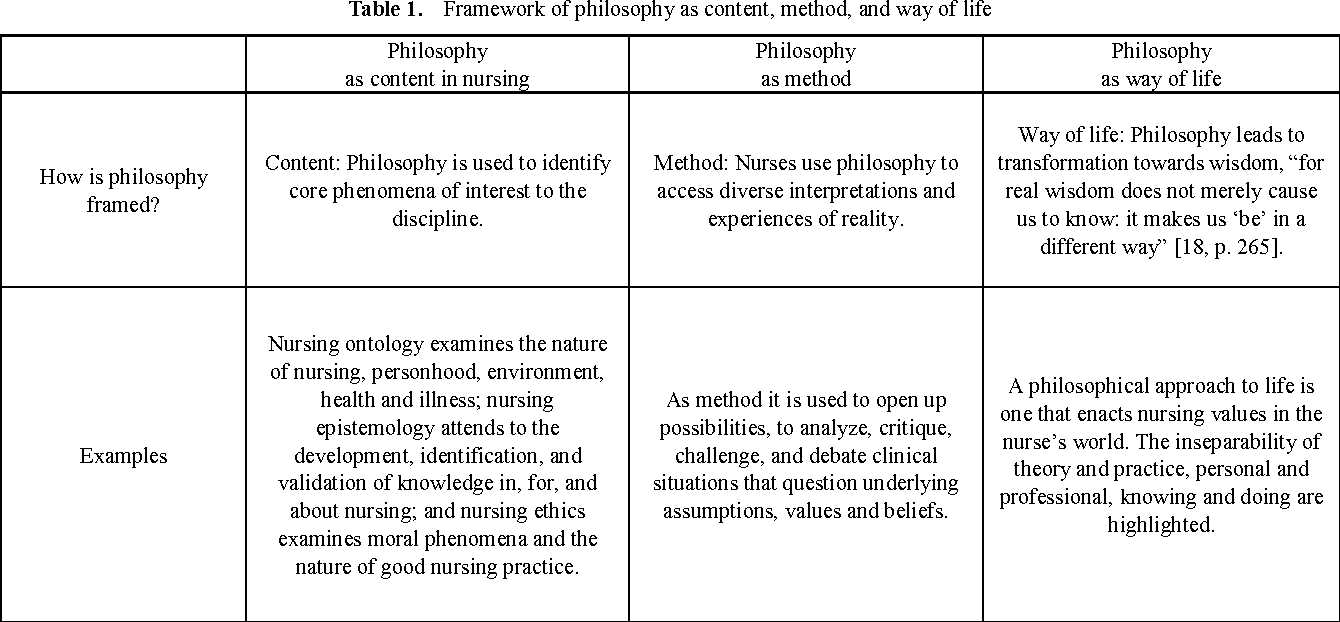
Exploring the Fundamentals of Nursing Philosophy
At the heart of every healthcare practice lies a set of foundational beliefs and values that guide how care is provided. These core principles form the basis for decisions, actions, and interactions with patients, ensuring that professionals approach their work with integrity, empathy, and a deep understanding of human well-being. By reflecting on these guiding concepts, practitioners can cultivate a mindset that prioritizes both the technical and compassionate aspects of their role.
These fundamental ideas are shaped by a variety of factors, including cultural influences, personal experiences, and the evolving demands of the healthcare system. They offer a framework for navigating complex ethical dilemmas, understanding patient needs, and promoting holistic care. Through ongoing education and self-reflection, healthcare providers refine their approach, adapting to the challenges of their practice while maintaining a commitment to high standards of care.
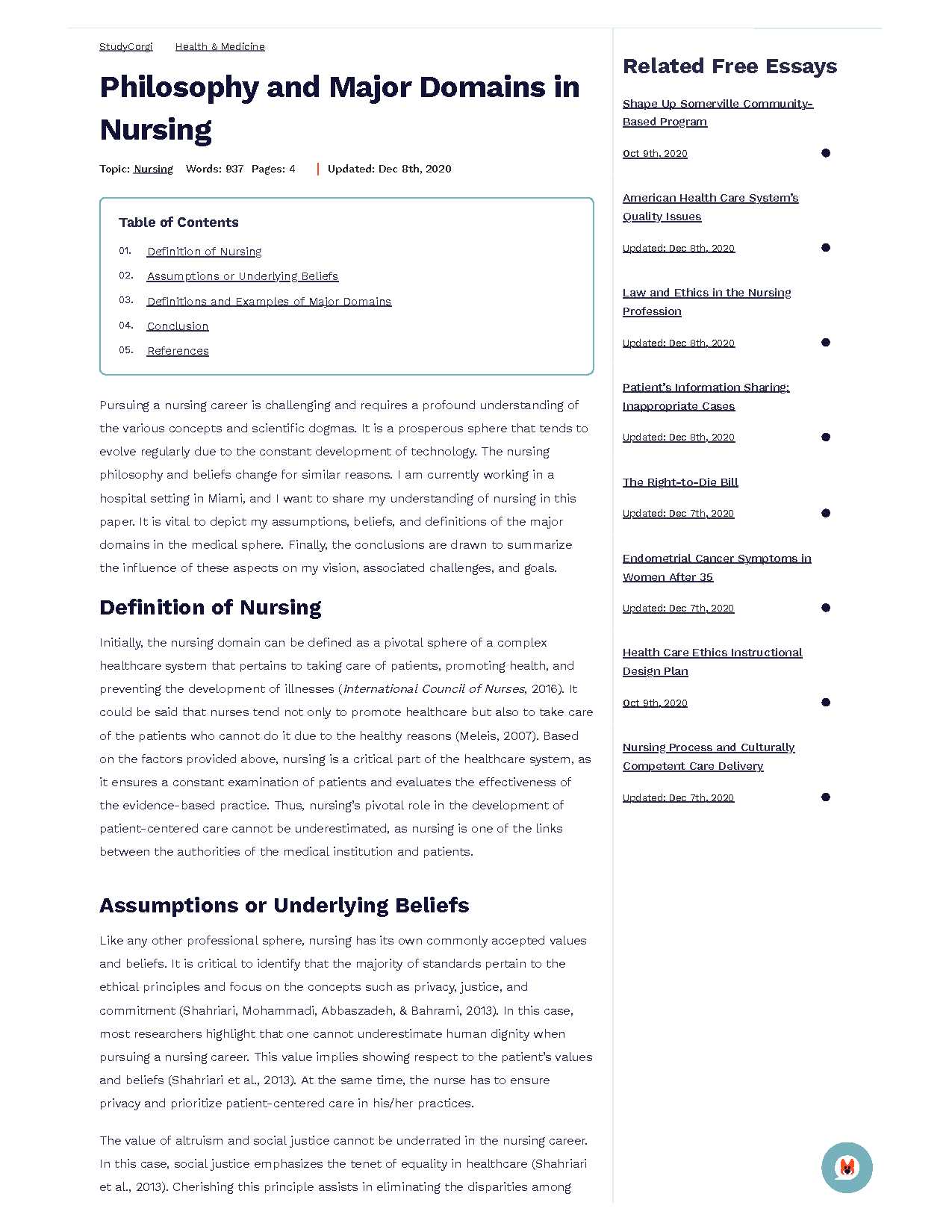
| Key Concept | Impact on Practice |
|---|---|
| Empathy | Improves patient communication and trust |
| Ethical Responsibility | Guides decisions related to patient rights and well-being |
| Holistic Care | Focuses on treating the whole person, not just the illness |
| Critical Thinking | Enhances problem-solving and decision-making in complex situations |
Defining Key Concepts in Nursing Philosophy

In any field of care, understanding the core ideas that shape practice is crucial for providing effective and compassionate support. These essential beliefs serve as the foundation for all actions and decisions, helping to guide professionals in their interactions with those they serve. By clearly defining and examining these guiding principles, individuals within the profession can develop a deeper understanding of their role and responsibilities.
Core Beliefs that Shape Practice
The central concepts that drive this field include a deep respect for human dignity, the recognition of individual needs, and the responsibility to provide care that supports both physical and emotional well-being. These values serve as the cornerstone for forming relationships with patients, establishing trust, and delivering care that is both ethical and effective.
Integrating Theory into Real-World Care
The integration of these fundamental ideas into everyday practice is essential for ensuring that care is provided in a holistic and compassionate manner. By consistently reflecting on and applying these core values, professionals are better equipped to address the complex challenges they face and contribute to the overall well-being of those in their care.
The Role of Ethics in Nursing Philosophy
Ethical principles are the cornerstone of any healthcare practice, shaping the way professionals approach their duties and interact with those in their care. These moral guidelines are critical for ensuring that care is provided in a manner that respects human dignity, prioritizes patient autonomy, and promotes well-being. The integration of ethical standards into daily practice helps professionals navigate difficult decisions and respond to the complexities of patient needs.
Guiding Decision-Making in Healthcare
Ethical considerations influence every aspect of healthcare, from the treatment options presented to patients to the way in which sensitive information is handled. Professionals are often faced with choices that require balancing the best interests of the patient, legal regulations, and the expectations of society. Clear ethical frameworks provide the necessary guidance to make these decisions with integrity and compassion.
Building Trust and Respect in Patient Care
Trust is essential in the healthcare environment, and ethical behavior plays a key role in fostering this trust. When patients believe that their care providers are acting with honesty, transparency, and a commitment to their well-being, they are more likely to engage in treatment and follow recommended care plans. Upholding ethical standards ensures that patient-provider relationships remain strong and effective.
Historical Development of Nursing Philosophy

The evolution of core beliefs and values within healthcare practice has been shaped by centuries of social, cultural, and scientific changes. From its early origins to its modern-day complexities, the development of ideas around patient care has been a reflection of shifting societal needs, advancements in medical knowledge, and the ongoing quest for ethical standards. Understanding this historical trajectory helps to appreciate how contemporary practices have emerged and how they continue to evolve.
The Early Foundations of Healthcare Practices
In ancient times, healthcare was often intertwined with spiritual beliefs and practices. Early caregivers were primarily guided by intuition and basic healing methods, with little distinction between medical and moral considerations. As societies advanced, there was a gradual shift toward more structured care, where the roles of caregivers became more defined, and attention to the well-being of individuals started to take a more systematic form.
Modern Shifts and the Institutionalization of Care
The modern era saw a significant shift, especially in the 19th and 20th centuries, as professional education, scientific advancements, and more formal ethical standards began to take hold. With the establishment of formal training programs and professional organizations, care practices became more standardized, and a deeper focus was placed on patient rights and holistic approaches to healing.
| Era | Key Developments |
|---|---|
| Ancient Civilizations | Healing combined with spiritual practices, care often informal |
| Middle Ages | Care provided mainly by religious institutions, limited medical knowledge |
| 19th Century | Introduction of formal education and training, emergence of ethical standards |
| 20th Century | Professionalization of care, scientific advancements, focus on patient rights |
Influential Theories in Nursing Philosophy
Theories play a crucial role in shaping the practices and values within the healthcare field, offering frameworks through which professionals can understand their roles and responsibilities. These theories provide guidance on how to approach patient care, how to make decisions, and how to balance technical skills with empathy and ethical considerations. Over time, several key theories have emerged, influencing the way healthcare is provided and advancing the profession’s approach to complex care scenarios.
Humanistic Theories and Patient-Centered Care
Humanistic theories emphasize the importance of empathy, respect, and the holistic approach to care. These theories prioritize the emotional and psychological needs of patients alongside their physical well-being, advocating for a personalized and compassionate approach. By focusing on the individual as a whole, these frameworks encourage caregivers to develop a deeper understanding of the patient’s unique experiences and needs.
Scientific and Systems-Based Approaches
In contrast to humanistic theories, scientific and systems-based theories offer a more structured and analytical perspective. These approaches focus on evidence-based practices, clinical protocols, and the integration of scientific knowledge into patient care. By organizing healthcare into defined systems, these theories help professionals streamline processes and enhance efficiency while maintaining high standards of care.
Application of Philosophy in Nursing Practice
The integration of core beliefs and guiding principles into everyday healthcare practice is essential for providing high-quality, compassionate care. These foundational concepts not only shape decision-making but also influence how professionals engage with patients, families, and colleagues. By applying these principles, practitioners are better equipped to address the complexities of care, balancing technical skills with empathy and ethical responsibility.
In practice, these ideas manifest in various ways, from establishing trust with patients to making ethically sound decisions in difficult situations. For example, a caregiver might draw on the value of patient autonomy when discussing treatment options, ensuring that the patient’s preferences are respected while also considering the best medical course of action. By continuously applying these concepts, healthcare providers can create environments where patients feel understood, respected, and supported in their journey to wellness.
The Relationship Between Nursing and Patient Care
The connection between healthcare providers and the individuals they care for is at the heart of effective treatment and recovery. This relationship goes beyond the technical aspects of medical care, encompassing emotional, psychological, and social support. A strong, compassionate connection helps to foster trust, improve communication, and ensure that patients feel valued and understood throughout their healing process.
Building Trust Through Communication
Clear and open communication is essential in establishing trust between caregivers and patients. By actively listening and responding with empathy, healthcare providers can create an environment where patients feel comfortable sharing their concerns, needs, and expectations. This trust strengthens the overall care process, ensuring that patients are more likely to follow treatment plans and make informed decisions about their health.
Holistic Care and Its Impact on Well-Being
Effective care is not just about addressing physical symptoms; it also involves considering the emotional and psychological needs of the patient. Holistic care takes into account the individual as a whole, recognizing that mental and emotional health are deeply interconnected with physical well-being. By understanding and addressing all aspects of a patient’s life, providers can enhance the healing process and improve overall outcomes.
Understanding Humanism in Nursing Philosophy
Humanism in healthcare is a perspective that emphasizes the value and dignity of every individual, focusing on the holistic care of patients. This approach highlights the importance of seeing each person as a unique being with distinct physical, emotional, and psychological needs. It encourages professionals to engage with patients not just as recipients of care but as individuals with personal experiences, beliefs, and values that influence their health and well-being.
At its core, humanism in healthcare is about fostering empathy, respect, and trust. By embracing this perspective, caregivers aim to establish meaningful connections with those they serve, creating environments where patients feel heard, understood, and cared for. This approach supports patient autonomy, encourages collaboration in decision-making, and ultimately promotes a more compassionate and patient-centered form of care.
Critical Thinking and Nursing Philosophy
Critical thinking is an essential skill in healthcare, allowing professionals to analyze situations, make informed decisions, and solve complex problems. In the context of patient care, it involves evaluating evidence, considering different perspectives, and applying knowledge in a way that promotes optimal outcomes. This skill helps professionals navigate challenges, particularly in situations where decisions may not be clear-cut or where multiple factors must be considered.
Key Components of Critical Thinking in Care
Effective critical thinking in healthcare requires several key elements:
- Analysis: Examining information thoroughly and identifying patterns or inconsistencies.
- Reflection: Assessing past experiences and considering how they inform future decisions.
- Evaluation: Weighing the potential outcomes of various actions and choosing the best course of action.
Applying Critical Thinking in Complex Scenarios
In complex healthcare situations, critical thinking enables professionals to:
- Identify the underlying issues or concerns affecting a patient’s health.
- Develop individualized care plans that consider both medical needs and personal circumstances.
- Make decisions that balance ethical considerations with clinical judgment.
By incorporating critical thinking into their practice, healthcare providers enhance the quality of care and contribute to better patient experiences and outcomes.
Philosophical Foundations for Nursing Education
The core principles that guide the education of healthcare professionals are rooted in fundamental beliefs about the nature of learning, teaching, and human development. These guiding ideas shape how educators design curricula, approach student engagement, and foster a deeper understanding of the complexities of patient care. By aligning educational strategies with these foundational concepts, institutions aim to produce skilled, compassionate professionals who are prepared to meet the challenges of an ever-evolving field.
At the heart of this educational approach is the belief that learning is a dynamic, interactive process that goes beyond the acquisition of technical knowledge. It is about cultivating critical thinking, ethical decision-making, and an understanding of the social, cultural, and emotional aspects of patient care. This perspective encourages educators to create an environment where students not only gain knowledge but also develop the personal qualities necessary to provide effective and compassionate care.
| Philosophical Concept | Implication for Education |
|---|---|
| Holistic Learning | Focus on developing the whole person, including emotional, social, and intellectual growth. |
| Constructivism | Encourage active learning through real-world experiences and reflection. |
| Humanism | Promote empathy, respect, and the development of personal values in care providers. |
| Critical Thinking | Develop the ability to assess situations, make informed decisions, and solve complex problems. |
The Impact of Nursing Philosophy on Policy
Core beliefs and guiding principles within the healthcare profession have a profound influence on the creation and implementation of policies. These foundational ideas shape how healthcare systems approach issues such as patient care, worker rights, and institutional practices. As professionals embrace values such as compassion, equity, and respect, these ideals often find their way into the policy-making process, ensuring that decisions align with the needs and dignity of both patients and providers.
When these guiding principles are incorporated into policy, they contribute to the development of frameworks that prioritize quality care, patient safety, and ethical standards. This alignment fosters environments where healthcare providers are empowered to deliver optimal care, while also ensuring that policies reflect the diverse needs of communities.
Key Areas Affected by Guiding Principles
- Patient Rights: Policies that prioritize respect, autonomy, and informed consent.
- Workplace Conditions: Guidelines that ensure safe and supportive work environments for caregivers.
- Resource Allocation: Decisions that reflect fairness and the equitable distribution of healthcare resources.
- Education and Training: Policies that emphasize ongoing learning and professional development for all healthcare workers.
Challenges and Opportunities in Policy Development
The integration of these core beliefs into policy is not without challenges. Balancing theoretical ideals with practical limitations can be difficult, especially when resources are scarce or when healthcare systems face significant pressures. However, the opportunity to influence policy through these values also presents a chance to create more compassionate, effective, and just healthcare environments.
Cultural Sensitivity in Nursing Philosophy

Cultural sensitivity is an essential aspect of healthcare that recognizes and respects the diverse backgrounds, values, and traditions of patients. By understanding and acknowledging cultural differences, healthcare professionals can provide more personalized and effective care. This approach emphasizes the importance of building trust, fostering open communication, and tailoring care to meet the unique needs of individuals from various cultural contexts.
Integrating cultural sensitivity into practice allows providers to offer care that not only addresses medical needs but also respects patients’ beliefs, preferences, and customs. This holistic approach helps improve patient satisfaction, compliance, and overall outcomes, while also promoting an inclusive and compassionate healthcare environment.
Key Components of Cultural Sensitivity in Care
- Respect for Beliefs: Understanding and accommodating patients’ religious, spiritual, and cultural beliefs in care decisions.
- Effective Communication: Using clear, culturally appropriate language and non-verbal cues to ensure understanding and comfort.
- Personalized Care: Adapting care plans to reflect the individual’s cultural preferences and values.
Benefits of Cultural Sensitivity in Healthcare
- Improved Patient Trust: Building stronger relationships through understanding and respect.
- Better Health Outcomes: Patients are more likely to follow treatment plans when their cultural needs are considered.
- Increased Patient Satisfaction: A culturally responsive environment fosters a positive experience for patients.
Philosophical Approaches to Nursing Leadership
Leadership within the healthcare field is deeply influenced by core beliefs and principles that shape decision-making, management, and the relationships between leaders and their teams. These guiding ideas provide a framework for leaders to navigate complex challenges, encourage collaboration, and inspire those they lead. Adopting different philosophical perspectives allows leaders to adjust their approach to best suit the needs of both their teams and patients, fostering an environment that prioritizes ethical care, innovation, and mutual respect.
By embracing various leadership models, healthcare leaders can cultivate a supportive, effective, and forward-thinking atmosphere that improves both staff satisfaction and patient outcomes. The right approach helps leaders remain adaptable and responsive to changes within the profession and to the diverse needs of individuals in their care.
Key Leadership Philosophies in Healthcare
- Transformational Leadership: Focuses on inspiring and motivating teams to achieve higher levels of performance and personal growth.
- Servant Leadership: Emphasizes prioritizing the needs of others, fostering a sense of trust, and supporting the development of team members.
- Ethical Leadership: Guides decision-making based on integrity, transparency, and fairness, ensuring that all actions align with moral and professional standards.
Impact of Leadership Approaches on Care Delivery
- Improved Team Collaboration: Leadership based on respect and empowerment enhances teamwork and cooperation.
- Enhanced Patient Outcomes: Ethical, compassionate leadership improves the quality of care provided.
- Increased Job Satisfaction: Supportive leadership boosts morale, leading to lower turnover rates and higher retention among healthcare staff.
Person-Centered Care and Nursing Philosophy
At the core of effective healthcare lies an approach that focuses on the individual, ensuring that their unique needs, preferences, and values are at the center of all care decisions. This method recognizes the importance of treating patients not as mere recipients of treatment but as active participants in their care journey. By prioritizing the whole person, healthcare professionals can provide more compassionate, tailored, and meaningful experiences, fostering stronger patient relationships and better overall outcomes.
Adopting a person-centered approach transforms the dynamic between caregivers and patients, shifting from a directive model to one that empowers individuals to be involved in their own health decisions. This shift encourages mutual respect, improves patient satisfaction, and promotes collaboration in achieving optimal health goals.
Principles of Person-Centered Care

- Respect for Individuality: Acknowledging and valuing each person’s unique cultural background, beliefs, and preferences.
- Collaboration in Care: Encouraging patients to take an active role in decisions about their health and well-being.
- Holistic Care: Considering all aspects of a person’s life–emotional, social, spiritual, and physical–when developing care plans.
Benefits of Person-Centered Care
- Enhanced Patient Satisfaction: When patients feel respected and heard, they are more likely to be satisfied with their care experience.
- Improved Health Outcomes: Engaging patients in decision-making and care leads to better compliance with treatment plans and overall well-being.
- Stronger Relationships: A focus on individual needs fosters trust and creates a supportive, collaborative healthcare environment.
Future Trends in Nursing Philosophy
The landscape of healthcare is constantly evolving, with new challenges and opportunities arising that shape how care is provided. As advancements in technology, research, and patient expectations continue to grow, the way healthcare professionals approach their practice is also changing. In the coming years, we can expect a greater emphasis on personalized care, technological integration, and holistic approaches that prioritize the well-being of the individual in all aspects of their health journey.
One of the most notable trends is the shift toward greater patient autonomy. As more people become informed and involved in their own care, healthcare providers will need to adapt by fostering more collaborative relationships with their patients. This transformation is likely to lead to the development of new models of care that are centered around individualized treatment plans, with a focus on the whole person rather than just their physical symptoms.
Another trend is the increasing use of artificial intelligence (AI) and data analytics to enhance decision-making and optimize care delivery. With the help of advanced technologies, healthcare providers will be able to analyze large sets of data to identify patterns, predict outcomes, and make more informed decisions. This will not only improve efficiency but also allow for more precise, evidence-based care.
Furthermore, the emphasis on interdisciplinary teamwork is expected to grow. As healthcare becomes more complex, collaboration between professionals from various fields will be essential to ensure comprehensive and well-rounded care. The ability to work as a cohesive team, drawing on the expertise of multiple disciplines, will be a critical component of future healthcare practices.
Challenges in Implementing Nursing Philosophy
While integrating fundamental principles into healthcare practice is essential, several barriers hinder the seamless adoption of these guiding ideas. From structural limitations within healthcare systems to individual resistance, these challenges can significantly impact how core values are incorporated into day-to-day activities. Overcoming these obstacles requires careful consideration, planning, and often a shift in both organizational culture and individual attitudes.
Organizational Barriers
One of the primary challenges in implementing these values is the existing structure within healthcare organizations. Many systems are designed around efficiency and productivity rather than providing holistic, patient-centered care. As a result, these practices may clash with approaches that prioritize individualized care and moral responsibilities toward patients. Some of the key organizational challenges include:
- Resource Constraints: Limited funding and staff shortages often restrict the ability to provide the ideal level of care, making it difficult to adhere to the values of compassionate and comprehensive care.
- Resistance to Change: Healthcare organizations may be reluctant to adopt new models or frameworks, especially if these require altering long-established procedures or workflows.
- Policy and Regulation Limitations: National or institutional policies might not fully support the integration of more personalized or value-driven approaches to patient care.
Individual and Cultural Challenges
In addition to organizational hurdles, individual practitioners and cultural factors also play a significant role in the difficulty of implementing these ideas effectively. Healthcare providers may struggle with conflicting demands, ethical dilemmas, or lack of training, which can impede the adoption of values-based care. These challenges include:
- Education and Training: Without proper training or understanding of these guiding principles, healthcare professionals may not feel equipped to apply them in their daily practice.
- Ethical Dilemmas: Healthcare providers may face moral conflicts when attempting to balance professional duties with patient autonomy or preferences, complicating the application of certain values in care.
- Cultural Resistance: In some cases, cultural attitudes towards certain approaches may prevent their acceptance, particularly in regions or institutions with deeply rooted traditions that differ from more progressive models.
Successfully overcoming these challenges requires commitment from all levels of the healthcare system, including leadership, policy-makers, and frontline staff, to create an environment that encourages the integration of these essential principles into everyday practice.