Evaluating the face involves a thorough understanding of its structure, functionality, and various conditions that can affect its appearance and performance. This procedure requires knowledge of anatomy, neurological responses, and common signs associated with certain health issues. The process is essential for professionals aiming to assess overall health or diagnose specific conditions linked to the face.
Comprehending key techniques plays a crucial role in ensuring accuracy and clarity during an assessment. Recognizing subtle differences in symmetry, muscle movements, or skin conditions can provide important insights. By studying the range of possible signs, individuals are better equipped to detect any irregularities or underlying concerns.
In this guide, we will explore the most relevant inquiries and solutions related to the examination of the face. We will discuss common challenges faced during assessments, along with the best practices to ensure effective and reliable results. Whether for general health checkups or specialized diagnostics, this section provides valuable knowledge for both professionals and those seeking to understand the assessment process better.
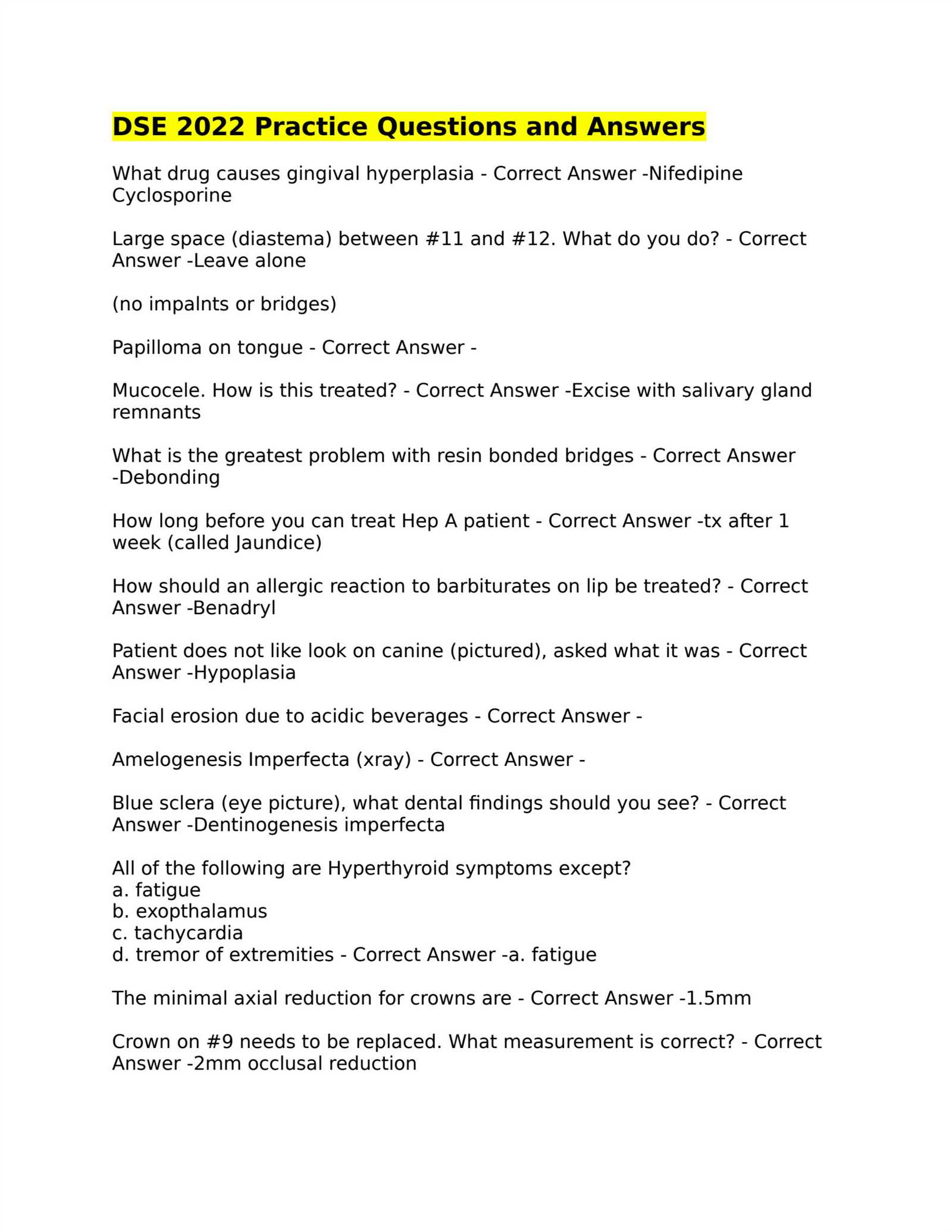
Facial Exam Questions and Answers
Understanding the process of evaluating the face requires familiarity with the key factors that contribute to a thorough assessment. Professionals must be able to identify signs, recognize variations in appearance, and understand the underlying causes of any abnormalities. By asking the right set of inquiries, one can gather crucial information that aids in proper diagnosis or treatment planning.
Common Issues to Explore
Inquiries often focus on symmetry, muscle activity, skin condition, and nerve function. For example, a typical concern is whether one side of the face behaves differently from the other, which can indicate neurological conditions or structural imbalances. Additionally, skin appearance can reveal a range of health conditions, from infections to chronic diseases.
Interpretation of Results
Once the relevant data is gathered, it is important to accurately interpret the results. Recognizing subtle shifts in expression, such as difficulty moving specific muscles or unusual skin texture, can be indicative of underlying problems. Understanding these signs is essential for determining the next steps in treatment or further testing.
Key Concepts in Facial Exams
To effectively assess the face, understanding its structure, function, and possible abnormalities is essential. This process requires a solid grasp of various aspects such as symmetry, muscle movement, skin texture, and nerve responses. A comprehensive understanding of these elements allows for accurate evaluations and helps in identifying potential issues.
One important aspect of the evaluation is the recognition of asymmetry. Differences in the appearance or movement of the left and right sides of the face can point to a variety of conditions. Another crucial factor is the assessment of muscle strength and function, as it can reveal underlying neurological concerns. Additionally, changes in the skin, such as discoloration, texture, or lesions, are often early indicators of both external and internal health issues.
These concepts form the foundation of any thorough assessment, allowing professionals to gather valuable insights that guide diagnosis and treatment decisions. Understanding these fundamental components ensures the identification of issues that may otherwise go unnoticed.
Common Questions in Facial Assessments
During a face evaluation, certain key topics frequently arise. These inquiries often center on identifying irregularities in appearance, muscle movement, and neurological function. Recognizing these concerns early on is crucial for accurate diagnosis and appropriate intervention.
A typical inquiry involves assessing symmetry–whether both sides of the face move equally or if one side exhibits weakness. Another common question relates to the functionality of facial muscles. For example, is there any difficulty in performing basic movements such as raising the eyebrows or smiling? Such issues can point to neurological disturbances or muscle-related conditions.
Skin appearance is also often a subject of focus. Questions may involve changes in texture, color, or the presence of unusual marks. These signs can reveal underlying health problems ranging from infections to chronic skin conditions.
Techniques for Accurate Facial Evaluation
Achieving a precise assessment of the face requires a combination of observation, palpation, and understanding the body’s natural responses. Various techniques help professionals identify issues with symmetry, movement, and skin health, providing valuable insights into a patient’s overall condition. By applying these methods, a comprehensive evaluation can be conducted, ensuring any abnormalities are recognized and addressed appropriately.
Observational Techniques
The first step in a thorough evaluation is careful observation. Evaluators should look for any signs of asymmetry, irregular muscle movements, or changes in skin texture. Subtle differences, such as a drooping eyelid or uneven smiles, may indicate nerve damage or muscle weakness. A well-trained eye can identify these discrepancies early on, prompting further investigation if necessary.
Palpation and Functional Tests
Another essential technique involves palpation, or the physical examination of muscles, skin, and bone structure. Gently pressing on different areas of the face can reveal tenderness or abnormal swelling that may be indicative of deeper health concerns. Additionally, functional tests, such as asking a person to smile or furrow their brow, help assess muscle strength and coordination, offering further clues about potential issues.
Preparing for a Facial Exam
Preparation for a thorough evaluation of the face involves several key steps that ensure the process is as accurate and effective as possible. Both the examiner and the individual undergoing the assessment should be well-prepared to make the most of the evaluation. By following a few simple guidelines, potential issues can be identified early and addressed promptly.
- Ensure comfort: Make sure the person being evaluated is relaxed and comfortable. Tension can affect muscle movement and skin response, leading to inaccurate results.
- Proper lighting: Good lighting is essential for detecting subtle signs and ensuring accurate observations. Bright, natural light is ideal for highlighting differences in symmetry or texture.
- Clear instructions: Clearly explain the procedure to the individual, ensuring they understand any movements or actions required during the assessment.
Additionally, the examiner should review the patient’s medical history, as any underlying conditions might influence the results. It’s also important to avoid any distractions during the assessment to ensure a focused and precise evaluation.
Understanding Facial Musculature and Function
The muscles of the face play a critical role in a variety of functions, from basic expressions to more complex actions such as speaking or chewing. A clear understanding of these muscles is essential for identifying any potential issues related to movement, coordination, or nerve function. Examining how these muscles interact and contribute to facial dynamics can provide valuable insights into a person’s overall health.
Key Muscles Involved in Movement
The face is home to several muscles that control movement in different areas, including the eyes, mouth, and forehead. These muscles work together to allow for a wide range of expressions and physical actions. Below is a table of some of the major muscles responsible for facial movement:
| Muscle | Function |
|---|---|
| Zygomaticus Major | Responsible for lifting the corners of the mouth, crucial for smiling. |
| Orbicularis Oculi | Controls the eyelids, enabling eye closure and squinting. |
| Frontalis | Raises the eyebrows and wrinkles the forehead. |
| Buccinator | Helps with chewing by compressing the cheeks. |
| Masseter | A major muscle for chewing, enabling jaw movement. |
Impact of Muscle Function on Health
Issues with the muscles of the face can be indicative of neurological disorders, injury, or other health conditions. For instance, weakness or paralysis in certain muscles may signal nerve damage or the onset of diseases like Bell’s palsy. Assessing the function of these muscles is therefore a crucial part of any thorough evaluation.
How to Interpret Facial Expressions
Understanding the subtle cues provided by the face is essential for interpreting a person’s emotional state, health status, or neurological function. The muscles and movements that create expressions are closely tied to underlying thoughts, feelings, and physical conditions. By recognizing these signals, a more accurate picture of an individual’s well-being can be obtained.
Facial expressions are powerful indicators of mood and reactions, often conveying more than words. By focusing on specific features, one can assess a wide range of emotions or detect potential health concerns.
Key Elements to Observe
- Eyes: The movement and openness of the eyes can signal emotions such as surprise, fear, or sadness. A lack of eye contact may also indicate discomfort or a neurological issue.
- Mouth: Smiling or frowning reflects happiness, sadness, or frustration. Uneven smiles or the inability to raise both corners of the mouth could point to muscle weakness.
- Eyebrows: Raised or furrowed brows indicate surprise, confusion, or anger. Difficulty moving the eyebrows can be a sign of nerve-related issues.
- Cheeks: The level of tension or relaxation in the cheeks can reveal tension or joy. Tightened cheeks may reflect stress or anxiety.
Common Expressions to Recognize
- Happiness: Characterized by a wide smile, squinting eyes, and raised eyebrows.
- Sadness: A downward curve of the mouth, drooping eyelids, and lack of eye brightness.
- Anger: Furrowed brows, tight lips, and glaring eyes.
- Surprise: Wide eyes, raised eyebrows, and an open mouth.
Recognizing these movements and their variations can provide key insights into a person’s emotional state and overall health. By honing the ability to interpret these expressions, professionals can gain a deeper understanding of their patients’ conditions or needs.
Facial Symmetry and Its Importance
Symmetry in the face is often considered a key indicator of health, development, and even attractiveness. The balance between the left and right sides of the face plays an essential role in various aspects of physical and emotional well-being. Any noticeable imbalance or asymmetry can provide valuable insights into underlying medical conditions or neurological issues.
When evaluating the face, it is important to assess the alignment of key features such as the eyes, eyebrows, nose, and mouth. Asymmetry can be a normal variation, but pronounced differences may indicate conditions that require attention.
Why Symmetry Matters
- Health Indicators: Imbalances in facial features may signal nerve damage, muscle weakness, or conditions like Bell’s palsy or stroke.
- Developmental Concerns: Significant asymmetry can be a sign of developmental abnormalities, such as congenital disorders or craniofacial syndromes.
- Psychological Implications: Disproportionate features can affect self-esteem and may contribute to social or emotional challenges.
How to Assess Symmetry
- Visual Inspection: Observe the alignment of facial features, looking for any obvious differences in size or shape between the left and right sides.
- Functional Tests: Ask the individual to perform facial movements, such as smiling or raising their eyebrows, to see if both sides of the face move evenly.
- Photographs: Taking photographs of the face from different angles can help highlight asymmetries that may not be visible during a direct observation.
Recognizing facial imbalance early allows for timely intervention and better outcomes. Understanding symmetry is crucial for identifying potential health concerns and enhancing overall well-being.
Assessing Skin Health During Exams
Evaluating the condition of the skin is a crucial part of understanding an individual’s overall health. The skin can reflect a wide range of internal conditions, from hydration levels to possible underlying diseases. A thorough assessment can help identify early signs of conditions such as infections, allergic reactions, or systemic disorders that might not be immediately visible elsewhere in the body.
When assessing skin health, it is important to focus on various aspects, including texture, color, and the presence of any unusual markings. Changes in the skin can often indicate a variety of health issues, making it essential to recognize these signs early for appropriate action.
- Texture: Skin that feels dry, rough, or scaly can indicate dehydration, nutrient deficiencies, or certain dermatological conditions.
- Color: Changes in color, such as redness, paleness, or a bluish tint, can be signs of circulatory issues, infection, or even liver problems.
- Presence of lesions: Bumps, rashes, or any unusual growths should be carefully examined for signs of skin cancer, infections, or allergic reactions.
A well-rounded approach to skin evaluation also includes assessing factors like elasticity and overall moisture levels, which can offer insight into age-related changes or health imbalances. Regular monitoring and careful examination can help in identifying potential concerns before they escalate.
Role of Facial Nerves in Evaluation
The nerves that control the muscles of the face play a pivotal role in both expression and function. These nerves are essential for various actions, such as smiling, blinking, and raising eyebrows. Assessing the condition and functionality of these nerves provides valuable insight into a person’s neurological health. Dysfunction in these nerves can indicate a range of conditions, from minor irritation to more serious neurological disorders.
By observing how well the facial muscles respond to different stimuli, clinicians can identify issues related to nerve damage, muscle weakness, or other medical conditions. Evaluating these functions is an important part of a comprehensive health assessment.
How Nerves Affect Facial Movements
- Muscle Coordination: Proper nerve function ensures coordinated movement of the muscles on both sides of the face. Asymmetry or weakness in these movements could indicate a nerve-related issue.
- Reflexes: Some facial nerve tests involve checking reflexes, such as the blink response. An impaired reflex may suggest nerve damage or neurological impairment.
- Facial Sensitivity: Nerves also provide sensory feedback from the skin. Reduced or altered sensation can indicate issues such as nerve compression or trauma.
Common Conditions Affecting Nerve Function
- Bell’s Palsy: A condition causing temporary weakness or paralysis on one side of the face, often due to nerve inflammation.
- Stroke: Nerve damage following a stroke may result in facial drooping or difficulty controlling facial muscles.
- Neuropathy: Damage to peripheral nerves can lead to loss of sensation, tingling, or weakness in the face.
By evaluating the facial nerve’s performance, healthcare providers can detect abnormalities early, allowing for timely intervention and treatment of underlying conditions.
Important Terminology in Facial Exams
In any assessment involving the face, certain terms are essential for accurate communication and understanding. These terms help describe the various features, conditions, and functions related to the face and its underlying structures. A clear understanding of these concepts is vital for both professionals and individuals undergoing evaluations.
Familiarity with the terminology used in these assessments ensures that healthcare providers can clearly communicate their observations and diagnosis. It also helps individuals undergoing evaluations to better understand the process and the results.
Key Terms to Know
- Asymmetry: The lack of balance between the left and right sides of the face, which can be a natural variation or indicate a health issue.
- Neurological Impairment: A condition where the nerves controlling facial muscles or sensory input are damaged, affecting movement or sensation.
- Muscle Tone: The normal tension in facial muscles, which is important for functions such as expressions and speech.
- Hypertension: High blood pressure, which can sometimes affect facial appearance or contribute to vascular changes.
- Dermatological Concerns: Issues related to the skin on the face, including rashes, scars, or lesions, which may require further medical attention.
Common Conditions
- Bell’s Palsy: A sudden weakness or paralysis of the facial muscles, often caused by nerve inflammation.
- Stroke: A sudden interruption of blood flow to the brain, which can affect the muscles on one side of the face.
- Rash: Redness or irritation on the skin, which may be indicative of an allergic reaction or other health conditions.
Knowing the key terms can enhance the clarity of the discussion, leading to a more efficient and accurate evaluation of the face’s condition and function.
Addressing Facial Pain in Exams
When discomfort occurs in the face, it’s essential to carefully assess the underlying causes. Various conditions can contribute to pain in this area, ranging from nerve irritation to muscle tension. Understanding the nature and location of the pain helps determine the most effective approach for relief. This section explores common causes of facial discomfort and the steps to take for accurate assessment and treatment.
Common Causes of Facial Discomfort
- Sinus Infections: Often accompanied by pressure and tenderness, these can lead to discomfort around the nose, cheeks, and forehead.
- Temporomandibular Joint Disorders: Pain can arise from problems with the jaw joint, affecting the lower face, particularly when chewing or speaking.
- Trigeminal Neuralgia: A condition involving sharp, shooting pain in the face, typically triggered by simple movements or light touch.
- Dental Issues: Infections or tooth problems may cause referred pain, which can radiate to the jaw or cheeks.
Methods of Evaluating Pain
- Detailed Symptom Assessment: Identifying the exact nature and location of the pain is the first step in narrowing down possible causes.
- Physical Examination: Gently palpating areas of discomfort can help determine if the pain is due to muscle strain, joint dysfunction, or nerve involvement.
- Medical History Review: A thorough patient history, including any previous injuries or dental issues, may provide clues to the source of the pain.
Accurate diagnosis and effective treatment require a methodical approach to pain evaluation. Addressing the root cause ensures appropriate management, helping patients find relief and preventing further complications.
Facial Exam in Neurological Assessments
When evaluating neurological function, the appearance and movement of the face play a crucial role in identifying potential disorders. Observing the symmetry and muscle function of the face can provide important insights into the health of the nervous system. Abnormalities in facial expressions or sensations may indicate underlying neurological conditions, making this part of the evaluation essential for accurate diagnosis and treatment.
Neurological assessments often begin with the observation of facial muscle movements, as they can reveal clues to various issues such as nerve damage, stroke, or other central nervous system abnormalities. Through a combination of visual inspection and targeted testing, healthcare professionals can assess how well the facial muscles respond to stimuli.
Common Neurological Tests for the Face
- Smile and Frown Tests: Asking the patient to smile or frown helps assess the integrity of the facial nerve and the muscles it controls.
- Eyebrow Raise Test: This test evaluates the upper part of the face and can indicate issues with the facial nerve or central nervous system.
- Light Touch and Pain Sensation: Testing sensitivity in various areas of the face can identify sensory nerve dysfunction or other neurological conditions.
Interpreting Abnormal Findings
- Asymmetry: Uneven facial movements can be a sign of stroke, Bell’s palsy, or other neurological conditions affecting the facial nerve.
- Weakness or Paralysis: Difficulty performing basic movements like smiling or closing the eyes may suggest a neurological issue affecting the motor function of the face.
- Sensory Loss: Numbness or altered sensations on one side of the face could indicate problems with the trigeminal nerve or other neurological disorders.
Incorporating a thorough facial examination into a neurological assessment is vital for identifying early signs of neurological diseases. By evaluating facial muscle function and sensation, healthcare providers can detect conditions like stroke, facial nerve palsy, or other nerve-related disorders in their early stages, allowing for timely intervention and management.
Common Mistakes During Facial Evaluation
When assessing the appearance and function of the face, several common errors can lead to inaccurate conclusions or missed diagnoses. These mistakes may stem from improper techniques, misinterpretation of signs, or failure to consider the full range of potential conditions. Recognizing and avoiding these pitfalls is crucial for ensuring a comprehensive and reliable evaluation.
Overlooking Subtle Symptoms
One of the most common mistakes is failing to detect subtle signs that could indicate underlying issues. For example, slight asymmetry or minor facial drooping may be easily overlooked, yet they could be early indicators of conditions such as stroke or Bell’s palsy. It’s essential to take a thorough approach and not dismiss small but significant differences in facial movement or sensation.
Relying Solely on Visual Inspection
While visual inspection is an important part of the evaluation process, it should not be the only method used. Relying only on what can be seen may lead to missed sensory or motor deficits. Testing facial movements, such as asking the patient to smile, frown, or raise their eyebrows, as well as assessing touch sensitivity, provides a more complete picture of neurological health. A comprehensive evaluation should combine observation with active testing.
Inaccurate conclusions can also arise from failure to assess the context in which the symptoms appear. For instance, facial asymmetry or weakness could be the result of non-neurological issues like muscle fatigue or psychological stress. It’s important to consider the broader clinical picture and patient history before reaching a diagnosis.
By avoiding these common mistakes, healthcare professionals can improve the accuracy of their evaluations, ensuring that any underlying conditions are identified and addressed promptly. A thorough and methodical approach is essential for achieving the best outcomes for patients.
Facial Exam in Pediatric Patients
When assessing the health and development of young patients, it is crucial to carefully observe various facial features and functions. This process requires a tailored approach, taking into consideration the unique anatomy, behavior, and responses of children. Identifying any abnormalities early on can significantly impact treatment and long-term health outcomes.
Consideration of Growth Patterns
In pediatric patients, it is important to understand that facial structures undergo significant changes as they grow. What might appear as an asymmetry or abnormality in an adult patient could be a normal part of a child’s development. Therefore, an examiner must have a solid understanding of typical growth patterns to avoid unnecessary concern over natural variations.
Engaging the Patient
Working with children requires not only technical knowledge but also the ability to make them feel comfortable during the evaluation. Young patients may not always cooperate, so it is essential to approach the assessment with patience. Techniques such as using toys or encouraging playful interaction can help engage the child and allow the examiner to accurately assess facial movements and reactions. This interaction is vital for a thorough evaluation, as children may not be able to verbalize discomfort or unusual sensations.
Additionally, caregivers often play a crucial role in providing information about the child’s history or any changes noticed in facial expressions, such as drooping, weakness, or other signs of concern. Gathering this information can be just as critical as the direct assessment.
By keeping these considerations in mind, healthcare providers can effectively assess pediatric patients and ensure any issues are addressed promptly, helping to support healthy development.
Post-Exam Recommendations for Patients
After undergoing a thorough assessment, patients often require guidance on how to manage their health and maintain optimal well-being. Providing clear and actionable recommendations is essential to help patients understand the next steps and promote recovery or preventive care. These instructions can range from lifestyle adjustments to follow-up procedures, depending on the findings and the patient’s condition.
General Care Guidelines
For patients who have undergone a comprehensive evaluation, general care recommendations typically focus on maintaining a healthy lifestyle. This includes advice on nutrition, hydration, and exercise. Ensuring that patients follow these guidelines can improve their overall health and prevent complications in the future.
Follow-up and Monitoring
In some cases, further monitoring or follow-up visits may be necessary to track the patient’s progress or to assess the effects of any treatment prescribed. It is important to schedule these appointments promptly and ensure that patients are aware of when they should return for reassessment.
| Recommendation | Details |
|---|---|
| Hydration | Drink plenty of water to maintain skin health and overall well-being. |
| Exercise | Engage in moderate physical activity to improve circulation and muscle tone. |
| Rest | Get adequate sleep to allow the body to heal and recover. |
| Follow-up visit | Schedule a follow-up appointment in 4-6 weeks to monitor progress. |
These recommendations are designed to enhance recovery and ensure that any underlying issues are addressed effectively. Patients should feel encouraged to reach out to their healthcare provider if they experience any changes in their condition or if they have concerns about their care plan.
Understanding Anatomy for Assessments
For any comprehensive evaluation, having a clear understanding of the underlying structure of the face is essential. The complex arrangement of muscles, nerves, bones, and skin contributes significantly to both functional and aesthetic aspects. Knowledge of this intricate structure helps in identifying abnormalities, assessing movement, and ensuring proper care during the evaluation process.
Knowing the key components and their roles aids in better decision-making and accurate interpretations. A detailed understanding allows for effective diagnosis, treatment planning, and patient communication, leading to improved outcomes in healthcare settings.
| Component | Description |
|---|---|
| Muscles | Responsible for facial expressions, movement, and other functional actions. |
| Nerves | Transmit sensory and motor information to control movement and sensation. |
| Bones | Provide structure and support for the face and help form the skeletal framework. |
| Skin | Acts as a protective barrier and plays a role in sensory functions. |
Understanding how these components interact provides a foundational basis for accurate assessments and effective treatment plans. It is crucial to consider how each element influences overall function and appearance when performing a thorough review of the face.