Mastering gastrointestinal topics is essential for anyone pursuing a career in healthcare, especially when preparing for certification exams. The gastrointestinal system plays a critical role in overall patient care, and understanding its complexities can significantly enhance your clinical judgment and decision-making skills.
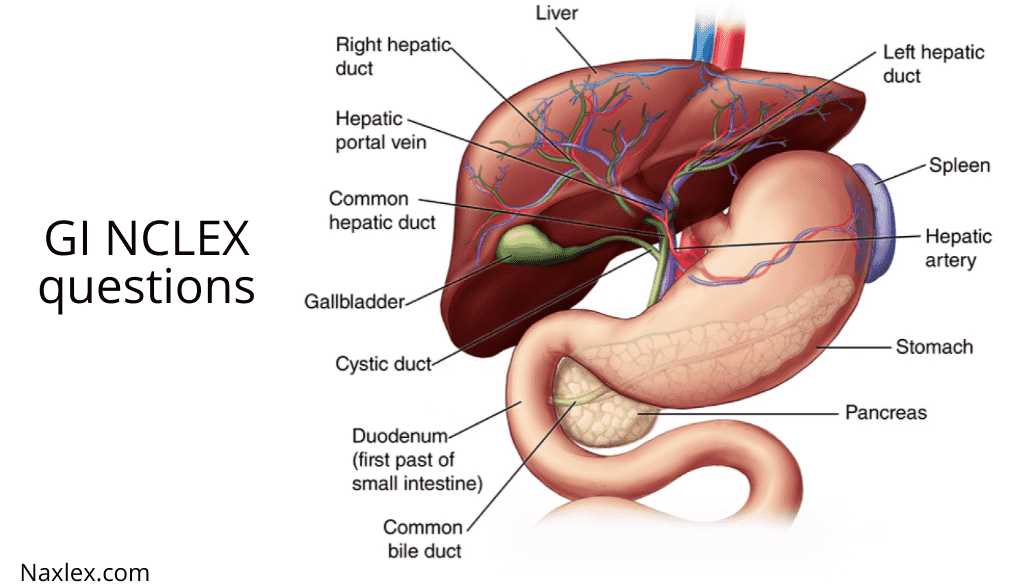
Focus on core principles that govern gastrointestinal health and common disorders. A solid foundation in anatomy, physiology, and pathophysiology is crucial for tackling exam scenarios related to the digestive system. By strengthening your grasp on these concepts, you will be well-prepared for practical applications in real-world settings.
Effective preparation involves not only memorizing facts but also understanding how to apply knowledge in various clinical situations. This approach will help you better navigate the different challenges you may face during your exam, as well as in patient care. Staying informed about the latest treatment protocols and diagnostic techniques is key to excelling in both the written and practical assessments.
Gi NCLEX Questions and Answers
Preparing for an exam focused on gastrointestinal topics requires a thorough understanding of both the theoretical and practical aspects of digestive health. Being able to identify key concepts and apply them in different clinical situations is essential. In this section, we will explore various challenges commonly faced during such assessments and offer insights into how best to approach them.
Key Areas to Focus On
Successful preparation revolves around mastering several core areas. These topics are frequently tested and serve as a foundation for understanding more complex scenarios:
- Understanding gastrointestinal anatomy and function
- Recognizing common disorders such as ulcers, GERD, and IBS
- Interpreting diagnostic tests and lab results
- Pharmacological treatments for digestive conditions
- Patient education on managing gastrointestinal health
Common Clinical Scenarios
Many exam scenarios present real-world situations that test your ability to make informed decisions based on clinical evidence. Here are examples of situations you may encounter:
- Managing a patient with severe abdominal pain and suspected appendicitis
- Assisting a patient who has recently undergone gastrointestinal surgery
- Evaluating a patient with chronic gastrointestinal symptoms
By practicing these types of cases, you will gain confidence in your decision-making abilities and improve your readiness for the exam. Each scenario tests your understanding of pathophysiology, patient care, and critical thinking under pressure.
Understanding the GI System for NCLEX
Grasping the fundamentals of the gastrointestinal system is essential for success in any healthcare examination. This system is responsible for the digestion, absorption, and processing of nutrients, and understanding its complex functions will significantly aid in managing related clinical scenarios. A clear comprehension of the GI system not only enhances your theoretical knowledge but also prepares you for practical application in patient care.
To fully understand the gastrointestinal system, it’s crucial to break it down into its key components. These include the digestive organs, enzymes, and processes that work together to ensure nutrient absorption and waste elimination. Below is a table that outlines the major parts of the system and their functions:
| Organ | Function |
|---|---|
| Mouth | Begins the digestive process by breaking down food with saliva and chewing. |
| Esophagus | Transports food from the mouth to the stomach via peristalsis. |
| Stomach | Secretes acid and enzymes to break down food and absorb some nutrients. |
| Small Intestine | Absorbs most of the nutrients from digested food into the bloodstream. |
| Large Intestine | Absorbs water and salts, forming waste to be eliminated. |
By studying each of these components in detail, you will gain a better understanding of how the system functions as a whole. This knowledge is essential for identifying issues, diagnosing conditions, and providing appropriate treatments in clinical practice. Furthermore, it will strengthen your ability to interpret related scenarios during any exam, enhancing both your theoretical knowledge and practical skills.
Common GI Disorders in NCLEX Exams
Gastrointestinal disorders are frequently tested in clinical exams due to their wide-ranging impact on patient health. These conditions can affect various parts of the digestive system, each presenting unique challenges in diagnosis and treatment. Understanding the common disorders and their symptoms will help you identify key issues during the assessment process and offer effective solutions in clinical practice.
Common Gastrointestinal Conditions
Some gastrointestinal disorders are commonly encountered in exams and are essential to understand for proper patient care. These conditions vary in severity and require different approaches for management:
- Gastroesophageal Reflux Disease (GERD): A chronic condition where stomach acid or bile irritates the food pipe lining, leading to symptoms like heartburn and regurgitation.
- Peptic Ulcer Disease: Open sores that develop on the inner lining of the stomach or small intestine, often due to bacterial infections or prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs).
- Irritable Bowel Syndrome (IBS): A functional GI disorder characterized by abdominal pain, bloating, and changes in bowel movements.
- Crohn’s Disease: An inflammatory bowel disease that causes inflammation in parts of the digestive tract, leading to symptoms such as diarrhea, abdominal cramps, and weight loss.
Managing GI Disorders in Clinical Practice
Effective management of gastrointestinal disorders often requires a combination of pharmacological and non-pharmacological approaches. Treatment strategies may include medications to reduce acid production, antibiotics for infections, or dietary adjustments to relieve symptoms. Understanding these treatment protocols and how to apply them in different clinical scenarios is crucial for providing optimal care.
Key Concepts in GI Physiology
The gastrointestinal system is responsible for several critical processes that ensure proper nutrient absorption and waste elimination. Understanding the fundamental principles of GI physiology helps in diagnosing and treating various digestive disorders. By familiarizing yourself with the system’s functions, you will be better equipped to approach clinical situations and provide effective care.
The following key concepts are essential for grasping the underlying mechanisms of the GI system:
- Digestive Enzyme Function: Enzymes play a vital role in breaking down food into absorbable nutrients. Amylase, lipase, and protease are some of the primary enzymes involved in the breakdown of carbohydrates, fats, and proteins, respectively.
- Motility and Peristalsis: The coordinated muscle contractions known as peristalsis move food along the digestive tract. This process is crucial for the proper functioning of the esophagus, stomach, and intestines.
- Absorption in the Small Intestine: The majority of nutrient absorption occurs in the small intestine, where villi and microvilli increase the surface area to maximize nutrient uptake.
- Acid-Base Balance: The GI system plays a role in regulating the body’s pH. The secretion of stomach acid helps digest food but must be balanced to prevent conditions like acid reflux or ulcers.
Understanding these physiological processes is fundamental for recognizing abnormalities that may arise during clinical examinations. A solid grasp of GI physiology allows healthcare providers to assess symptoms, perform appropriate tests, and select the most effective treatment options.
Preparing for GI-Related NCLEX Questions
Proper preparation for gastrointestinal topics is essential for success in any healthcare certification exam. A strong understanding of the digestive system, common disorders, diagnostic procedures, and treatment protocols is crucial. By focusing on key concepts and honing critical thinking skills, you can effectively tackle challenges related to GI health in an exam setting.
Here are some strategies to help you prepare for GI-related scenarios:
- Review Anatomy and Physiology: Ensure you have a solid grasp of the structure and functions of the GI system, including the digestive organs, enzymes, and absorption processes.
- Focus on Common Disorders: Study frequently tested conditions such as GERD, peptic ulcers, Crohn’s disease, and irritable bowel syndrome. Understand their pathophysiology, symptoms, and treatment options.
- Practice Clinical Scenarios: Engage in practice questions and case studies that involve GI-related symptoms and treatment protocols. This helps you apply theoretical knowledge to real-world situations.
- Master Diagnostic Procedures: Familiarize yourself with various diagnostic tests, including endoscopy, imaging, and lab work, as they are crucial in diagnosing GI disorders.
By focusing on these key areas, you will develop the expertise needed to approach GI-related cases with confidence. Consistent practice and review will strengthen your ability to quickly identify the correct course of action in both written and practical assessments.
Top Tips for GI Exam Success
Achieving success in any exam focused on gastrointestinal topics requires a combination of in-depth knowledge, practical skills, and efficient exam strategies. By understanding the critical concepts, practicing problem-solving techniques, and maintaining a structured study plan, you can improve your chances of excelling in the exam. Here are some proven tips to help you succeed.
Effective Study Techniques
Mastering the essential material is the first step in your preparation. Here are some key study strategies:
- Break Down Complex Topics: Tackle complicated subjects, like digestive disorders and treatment protocols, by breaking them into smaller, manageable sections. Focus on understanding the core principles first.
- Create a Study Schedule: Develop a study plan that allocates time for each topic based on its importance. Consistent daily review is more effective than cramming before the exam.
- Use Visual Aids: Diagrams, charts, and tables can help reinforce complex physiological processes, making them easier to remember and understand.
Practice with Real-Life Scenarios
One of the best ways to prepare is to simulate real-life situations that may arise in the exam. This not only helps in applying theoretical knowledge but also builds confidence:
- Work Through Case Studies: Engage with clinical scenarios that mimic exam-style questions. This helps you apply what you’ve learned and develop decision-making skills.
- Review Past Assessments: Analyze previous exams or practice tests to understand question formats, identify recurring themes, and familiarize yourself with the structure of questions.
- Test Your Knowledge: Regularly quiz yourself to gauge your understanding of key topics, and focus on areas where you feel less confident.
By applying these tips, you will be well-prepared to confidently tackle GI-related questions, making your exam experience smoother and more successful.
Approach to Gastrointestinal Assessment
Conducting a thorough assessment of the gastrointestinal system is essential for identifying any underlying issues that may affect a patient’s health. A systematic approach ensures that all relevant factors are considered, allowing for accurate diagnosis and effective treatment. The goal is to evaluate both subjective symptoms and objective findings to form a complete picture of the patient’s GI health.
The assessment begins with taking a comprehensive history, focusing on symptoms such as pain, bloating, changes in bowel habits, and weight loss. It is important to inquire about any previous GI conditions, family history, and lifestyle factors such as diet and alcohol consumption.
Next, a physical examination is conducted, which involves inspecting, palpating, percussing, and auscultating the abdomen. This helps to identify signs of inflammation, distention, or abnormal sounds that could indicate a problem with the digestive tract.
In some cases, further diagnostic testing may be necessary, such as blood work, stool samples, imaging studies, or endoscopy, to gather additional information and confirm a diagnosis. Each step in the assessment process is critical for ensuring that no aspect of the patient’s condition is overlooked.
Understanding Gastrointestinal Pharmacology
Pharmacology plays a crucial role in managing gastrointestinal disorders, as medications help alleviate symptoms, promote healing, and manage underlying conditions. Understanding the mechanisms, indications, and side effects of various drugs used to treat GI conditions is essential for effective patient care. The right medications can significantly improve patient outcomes, while improper use can lead to complications.
Common Classes of GI Medications
There are several categories of medications used to treat gastrointestinal issues, each targeting different aspects of digestion and absorption:
- Antacids: These neutralize stomach acid and provide quick relief from heartburn and acid reflux.
- Proton Pump Inhibitors (PPIs): PPIs reduce the production of stomach acid, helping to treat ulcers, GERD, and other acid-related disorders.
- H2 Receptor Antagonists: These block histamine receptors, reducing stomach acid secretion and offering relief from conditions like GERD and ulcers.
- Laxatives: Used to treat constipation, laxatives can either soften stool or stimulate bowel movements.
- Antidiarrheals: These medications, like loperamide, help slow down intestinal motility and reduce diarrhea.
Important Considerations in GI Pharmacology
While medications can be highly effective, their proper use requires careful consideration of the patient’s medical history, potential drug interactions, and any underlying conditions. It’s crucial to:
- Monitor for Side Effects: All GI medications come with potential side effects, such as nausea, headache, or dizziness. Regular monitoring helps prevent complications.
- Consider Drug Interactions: Many GI drugs can interact with other medications, potentially affecting their efficacy or leading to adverse effects. Careful evaluation is essential.
- Personalize Treatment: Treatment should be tailored to the individual, considering the severity of the condition, any co-existing disorders, and the patient’s response to medication.
By understanding gastrointestinal pharmacology, healthcare providers can more effectively manage patients’ conditions and improve long-term health outcomes.
Dietary Considerations for GI Conditions
Diet plays a pivotal role in managing gastrointestinal disorders. A well-balanced diet tailored to an individual’s condition can help alleviate symptoms, promote healing, and prevent complications. Understanding which foods to include or avoid is essential for optimizing digestive health and improving overall well-being.
For individuals with gastrointestinal issues, it’s important to focus on foods that are gentle on the digestive system while ensuring adequate nutrition. The goal is to reduce irritation, support proper digestion, and manage symptoms such as bloating, discomfort, or diarrhea.
Specific dietary changes are often recommended depending on the condition. For example, a high-fiber diet may benefit those with constipation, while low-fat or low-acid foods might be better suited for individuals with GERD or peptic ulcers.
Here are some general dietary guidelines for common GI conditions:
- For Irritable Bowel Syndrome (IBS): A balanced diet low in FODMAPs may help reduce bloating and discomfort. Small, frequent meals can also prevent digestive overload.
- For Gastroesophageal Reflux Disease (GERD): Avoid acidic foods like citrus, tomatoes, and spicy dishes. Opt for lean proteins, non-citrus fruits, and vegetables that don’t trigger reflux.
- For Inflammatory Bowel Disease (IBD): A low-residue diet may be recommended during flare-ups to reduce irritation. Foods that are easy to digest, such as cooked vegetables and lean meats, are often preferred.
- For Celiac Disease: Strictly avoid gluten-containing foods, such as wheat, barley, and rye. Incorporating gluten-free grains like rice and quinoa is essential for managing symptoms.
By tailoring dietary choices to the specific needs of the gastrointestinal system, patients can enhance their treatment plan, minimize discomfort, and maintain a better quality of life.
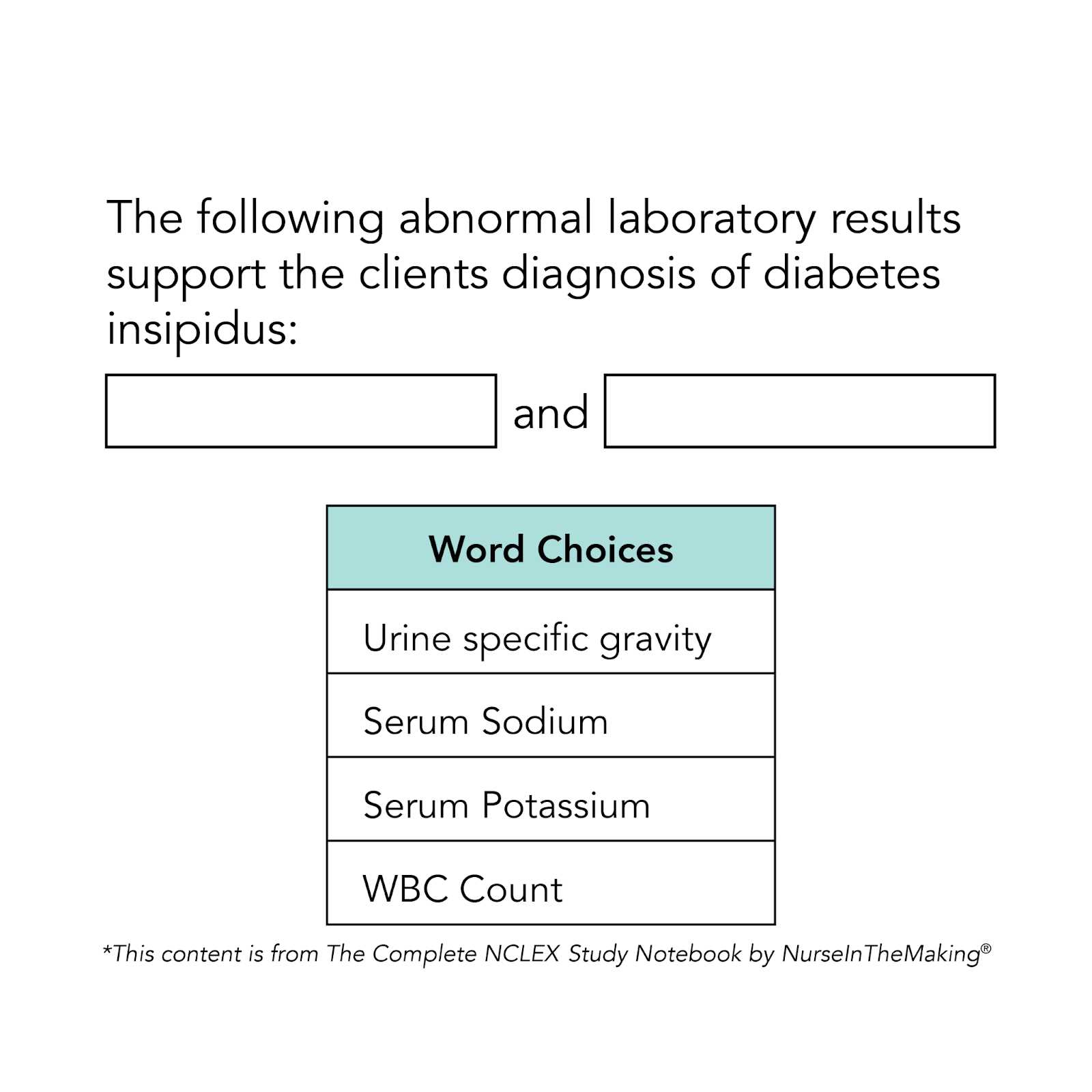
Interpreting Lab Results in GI Nursing
Interpreting laboratory results is an essential skill in gastrointestinal nursing, as these tests provide valuable insights into a patient’s digestive health. Understanding the significance of blood tests, stool samples, and imaging results allows healthcare professionals to make informed decisions about diagnosis and treatment. Lab results help identify abnormalities, track the progress of a condition, and determine the effectiveness of interventions.
Laboratory tests commonly used in the management of gastrointestinal conditions include liver function tests, electrolyte panels, complete blood counts, and stool cultures. Each test offers specific information that can guide clinical decisions and shape patient care plans.
For instance, elevated liver enzymes may indicate liver dysfunction or damage, while abnormal electrolyte levels could suggest dehydration or malabsorption. A low hemoglobin level might signal gastrointestinal bleeding or anemia, and stool samples can detect infections, parasites, or the presence of blood.
Below are some common lab tests and their implications in GI nursing:
- Liver Function Tests: Assess the health of the liver and its ability to process toxins and produce essential proteins. Abnormal results may indicate liver disease, such as cirrhosis or hepatitis.
- Complete Blood Count (CBC): Helps identify anemia, infection, or bleeding disorders, all of which may be related to GI conditions such as ulcers, Crohn’s disease, or colorectal cancer.
- Electrolyte Panel: Measures levels of sodium, potassium, chloride, and bicarbonate. Imbalances may occur due to vomiting, diarrhea, or malabsorption, affecting fluid and electrolyte balance.
- Stool Culture: Detects pathogens, such as bacteria, viruses, or parasites, which could be responsible for gastrointestinal infections or diarrhea.
By understanding the implications of lab results, nurses can better assess the severity of a patient’s condition, monitor progress, and collaborate with the healthcare team to provide optimal care.
GI Emergencies and NCLEX Question Types
Gastrointestinal emergencies require swift assessment, diagnosis, and intervention to prevent complications and improve patient outcomes. These critical conditions often involve severe symptoms, including intense pain, bleeding, or sudden changes in bowel movements, all of which demand immediate attention from healthcare providers. Recognizing the signs and symptoms of these emergencies, as well as knowing the appropriate actions to take, is essential for effective management.
In clinical settings, healthcare providers are expected to be prepared for a wide range of GI emergencies. These include conditions like acute pancreatitis, perforated ulcers, bowel obstructions, and gastrointestinal bleeding. Understanding the pathophysiology of these conditions and the best approach to patient care can significantly affect recovery rates and prevent long-term damage.
Common GI Emergencies
- Perforated Ulcer: A rupture in the stomach or duodenal lining can lead to peritonitis, a life-threatening infection that requires immediate surgical intervention.
- Acute Pancreatitis: Inflammation of the pancreas caused by factors such as gallstones or excessive alcohol use, often presenting with severe abdominal pain.
- Gastrointestinal Bleeding: This can be caused by conditions like peptic ulcers, varices, or diverticulosis, and may present with hematemesis or melena.
- Intestinal Obstruction: A blockage in the small or large intestine that can cause severe pain, vomiting, and bloating, requiring prompt treatment to avoid ischemia.
Understanding Question Types in GI Emergencies
When preparing for exams or clinical assessments, it’s important to understand the different types of questions that may be asked regarding GI emergencies. These questions often assess the ability to recognize symptoms, prioritize interventions, and apply critical thinking to real-life situations. Understanding the key concepts behind these questions will better equip you to succeed in both practical and theoretical settings.
| Question Type | Description |
|---|---|
| Priority Setting | Focuses on identifying the most urgent intervention or action based on patient symptoms or clinical presentation. |
| Situational Analysis | Assesses the ability to analyze a patient’s condition and determine the appropriate diagnostic and therapeutic interventions. |
| Pathophysiology-Based | These questions require understanding the underlying mechanisms of GI emergencies and the rationale behind treatment choices. |
| Interdisciplinary Collaboration | Evaluates the ability to recognize the role of the healthcare team in managing a patient’s condition and ensuring effective care. |
By mastering the content and understanding the types of questions related to GI emergencies, healthcare professionals can improve their clinical decision-making skills, provide better patient care, and succeed in assessments and examinations.
Patient Education for GI Disorders
Effective patient education is a critical aspect of managing gastrointestinal conditions. Educating patients about their condition, treatment options, and lifestyle modifications can significantly improve outcomes and quality of life. Patients who understand their disease are more likely to adhere to treatment plans, make necessary dietary and lifestyle changes, and recognize warning signs of complications, ultimately leading to better health management.
In the context of gastrointestinal disorders, education should focus on providing clear, concise information that empowers patients to take an active role in their care. It involves explaining the nature of the condition, how it affects the digestive system, and the importance of following prescribed therapies and recommended lifestyle changes. Additionally, addressing emotional and psychological aspects, such as coping with chronic symptoms or managing stress, can further enhance patient engagement in their recovery process.
Key Areas of Education
- Dietary Modifications: Patients with gastrointestinal disorders often benefit from specific dietary adjustments. Educating them on avoiding trigger foods, understanding food labels, and following recommended nutrition plans is vital to managing symptoms.
- Medications and Therapies: It is essential to explain the purpose of prescribed medications, potential side effects, and the importance of adhering to the treatment regimen. Patients should also be informed about non-pharmacological therapies, such as stress management techniques or physical therapy for certain conditions.
- Symptom Monitoring: Teaching patients how to track their symptoms, such as pain, bloating, or changes in bowel habits, helps in recognizing exacerbations early and seeking timely care.
- Preventive Measures: Patients should be educated on the role of preventive care, such as routine screenings, vaccinations, and regular check-ups to reduce the risk of complications or progression of their condition.
Promoting Adherence to Treatment Plans

Ensuring that patients follow their treatment regimens can be challenging, but providing education in a supportive and non-judgmental manner helps build trust and encourages compliance. Providing visual aids, such as brochures or diagrams, and addressing any concerns or misconceptions can further facilitate understanding. Additionally, involving family members or caregivers in the education process can enhance support systems and increase the likelihood of successful outcomes.
By focusing on comprehensive education, healthcare providers can empower patients to manage their condition effectively, reduce hospital readmissions, and improve their overall well-being.
Fluid and Electrolyte Balance in GI Care
Maintaining a stable balance of fluids and electrolytes is vital for the proper functioning of the body, particularly in patients with gastrointestinal issues. The digestive system is responsible for absorbing both nutrients and water, but disturbances caused by conditions like vomiting, diarrhea, or malabsorption can quickly lead to imbalances. These disruptions not only affect hydration status but can also impact the body’s ability to perform essential processes such as nerve transmission and muscle contraction. Effective management of these imbalances is crucial to support recovery and prevent complications.
In clinical practice, healthcare providers must regularly monitor the intake and output of fluids, assess vital signs, and perform lab tests to detect early signs of dehydration or electrolyte disturbances. By addressing imbalances promptly, it is possible to minimize the risk of further complications. Treatment strategies often involve replenishing lost fluids, restoring electrolyte levels, and ensuring that the gastrointestinal system is functioning properly.
Key Causes of Fluid and Electrolyte Imbalances
- Vomiting: Excessive vomiting leads to the loss of both fluids and electrolytes, particularly sodium and potassium, which are essential for normal cell function.
- Diarrhea: Prolonged diarrhea can cause rapid dehydration and significant electrolyte depletion, especially in cases of gastrointestinal infections or chronic conditions.
- Malabsorption Syndromes: Conditions like celiac disease or Crohn’s disease can prevent proper absorption of fluids and essential nutrients, contributing to fluid imbalances.
- Gastrointestinal Surgeries: Surgeries that involve the stomach or intestines may interfere with normal fluid absorption, leading to dehydration or imbalances that require careful management.
Management Approaches to Correct Imbalances
- Oral Rehydration Therapy: Replenishing lost fluids through oral rehydration solutions (ORS) can effectively replace lost fluids and electrolytes, especially in cases of mild to moderate dehydration.
- Intravenous Fluid Administration: When oral intake is insufficient or not possible, intravenous fluids, such as saline or lactated Ringer’s, are used to quickly restore hydration levels and stabilize the patient.
- Electrolyte Supplementation: In cases where patients are severely depleted, electrolyte replacement, including potassium, sodium, or magnesium, may be needed to restore balance.
- Continuous Monitoring: Regular monitoring of urine output and lab results is essential to evaluate the effectiveness of interventions and detect any ongoing imbalances.
With timely intervention and appropriate care, managing fluid and electrolyte imbalances can greatly improve outcomes for patients dealing with gastrointestinal disorders.
Postoperative Care for GI Surgery
After gastrointestinal surgery, proper postoperative care is essential to promote healing and prevent complications. Patients who undergo surgical procedures involving the digestive system require careful monitoring to ensure that their recovery progresses smoothly. The immediate postoperative period focuses on addressing pain management, fluid balance, and preventing infection, while longer-term care includes supporting the restoration of normal gastrointestinal function and nutrition. A comprehensive care plan tailored to the patient’s specific needs is key to a successful recovery.
During the recovery phase, healthcare providers need to assess a variety of factors including vital signs, wound healing, and the patient’s ability to tolerate oral intake. Early detection of complications, such as infections, bleeding, or gastrointestinal dysfunction, can significantly improve outcomes. Nurses play a pivotal role in educating patients about their recovery process, providing emotional support, and ensuring that appropriate interventions are taken as needed.
Key Aspects of Postoperative Care
- Pain Management: Effective control of postoperative pain is crucial for patient comfort and recovery. Medications such as opioids, along with non-pharmacological methods like relaxation techniques, are commonly used.
- Monitoring Vital Signs: Close observation of blood pressure, heart rate, and respiratory rate helps detect signs of complications such as bleeding or infection.
- Fluid and Electrolyte Balance: Maintaining proper hydration and electrolyte levels is essential, particularly in patients who have undergone extensive surgeries involving fluid loss or disruption of normal gastrointestinal function.
- Wound Care: Proper care of surgical incisions is critical to prevent infections. Regular inspection and cleaning of the wound site, along with timely dressing changes, are necessary.
- Early Mobilization: Encouraging early movement and ambulation can help prevent complications such as deep vein thrombosis (DVT) and promote overall circulation.
Dietary Considerations in Postoperative Care
- Initial Fasting: After surgery, patients are often kept on an NPO (nothing by mouth) status until bowel sounds return and gastrointestinal function resumes.
- Gradual Introduction of Fluids: Once patients are ready to begin eating again, clear liquids are typically introduced first, followed by soft foods and a regular diet as tolerated.
- Monitor for Complications: Diet progression should be closely monitored for signs of nausea, vomiting, or discomfort, which may indicate issues with digestion or absorption.
Effective postoperative management in GI surgery is vital to minimize risks and ensure a smooth recovery. By monitoring vital signs, managing pain, preventing infections, and providing appropriate nutrition, healthcare providers can help ensure that patients return to their normal activities as soon as possible.
Common Medications for GI Disorders
In the management of gastrointestinal disorders, medications play a crucial role in alleviating symptoms, improving digestion, and preventing complications. These conditions can vary widely, from acid reflux and ulcers to chronic inflammatory diseases and motility disorders. The selection of the right medication depends on the underlying cause, severity, and type of gastrointestinal issue. Healthcare providers must carefully assess each patient’s condition to prescribe appropriate treatments that can provide relief and promote healing.
Common treatments for GI disorders include antacids, proton pump inhibitors (PPIs), and anti-inflammatory medications, among others. Each category targets specific symptoms or conditions, and understanding their mechanisms is essential for effective treatment. In some cases, medications may be used in combination to manage more complex GI issues.
Antacids and Proton Pump Inhibitors
- Antacids: These over-the-counter medications neutralize stomach acid, providing quick relief for conditions like heartburn and acid reflux. Common examples include calcium carbonate and magnesium hydroxide.
- Proton Pump Inhibitors (PPIs): PPIs reduce the production of stomach acid, offering long-term relief for conditions like gastroesophageal reflux disease (GERD) and peptic ulcers. Medications such as omeprazole and lansoprazole are frequently prescribed.
Anti-inflammatory and Immunosuppressive Agents
- Corticosteroids: Used in the treatment of inflammatory bowel diseases (IBD) such as Crohn’s disease and ulcerative colitis, corticosteroids help to reduce inflammation and control flare-ups. Prednisone is a commonly prescribed corticosteroid.
- Immunomodulators: These medications, such as azathioprine and methotrexate, suppress the immune response and help manage autoimmune-related GI disorders.
In addition to these, other medications may be used to manage symptoms of GI disorders, such as anti-diarrheal agents, laxatives, and prokinetic drugs. Understanding the specific function and potential side effects of each medication is key to achieving optimal outcomes for patients.
Clinical Scenarios for GI Nursing Practice
In gastrointestinal nursing, professionals frequently encounter a wide range of clinical situations that require quick thinking and skilled intervention. These scenarios can involve patients experiencing acute conditions, such as abdominal pain, vomiting, or dehydration, as well as chronic issues like inflammatory bowel disease or gastrointestinal cancers. Nurses must be able to assess symptoms, implement interventions, and collaborate with other healthcare providers to ensure comprehensive care for individuals with digestive system disorders.
Clinical situations often require a mix of patient education, symptom management, and monitoring for complications. The nursing approach can vary significantly based on the severity of the condition, the patient’s medical history, and the overall treatment plan. Below are some common scenarios in gastrointestinal nursing practice and the considerations involved in their management.
Acute Gastroenteritis Management
Acute gastroenteritis is a common condition that can lead to dehydration and electrolyte imbalances. Nurses must assess the patient’s fluid status, administer intravenous fluids as needed, and monitor for signs of worsening dehydration. Providing education on hygiene practices, diet modifications, and the importance of hydration are essential components of care. Nurses must also stay alert for potential complications, such as sepsis or prolonged diarrhea, which may require additional intervention.
Chronic Inflammatory Bowel Disease (IBD) Care
For patients with conditions like Crohn’s disease or ulcerative colitis, ongoing management is essential. Nurses need to be aware of medication regimens, potential side effects, and the signs of flare-ups. Nutrition plays a key role in managing IBD, and patients may need guidance on modifying their diet to reduce symptoms. Regular monitoring for complications, such as bowel perforation or infection, is also important. Providing emotional support to patients dealing with a chronic condition is a crucial aspect of the nursing role.
Postoperative Care Following GI Surgery
After a gastrointestinal surgery, such as a colectomy or gastric bypass, the focus of nursing care shifts to monitoring for complications like infection, bleeding, or bowel obstructions. Nurses must assess the surgical site, manage pain, and support the patient’s mobility. Early nutrition support, including the introduction of clear liquids and progress to solid foods, is part of recovery. Educating patients about lifestyle changes and dietary adjustments following surgery is also essential for long-term success.
In all of these clinical situations, nurses must be prepared to use critical thinking, assess for potential complications, and provide holistic care. By staying updated on the latest protocols and maintaining strong communication with the healthcare team, nurses can help ensure positive outcomes for patients dealing with gastrointestinal issues.