In the field of healthcare, precise categorization plays a vital role in ensuring effective communication, billing, and patient care. Professionals in this area must navigate a complex system of codes that represent a variety of procedures, diagnoses, and services. This process requires a thorough understanding and careful attention to detail to avoid errors and discrepancies.
Over time, certain challenges have emerged that complicate the accuracy and consistency of this classification system. Whether it’s dealing with complex medical terminology, ensuring compliance with evolving regulations, or understanding the nuances of different systems, mastering this field demands continuous learning and practice. In this section, we will address common concerns and provide clarity on key concepts to help individuals enhance their expertise in this essential domain.
Medical Classification Insights and Solutions
Accurate classification is an integral part of healthcare operations. Professionals in this field must ensure that every service, diagnosis, and procedure is represented by a corresponding code. Errors in this process can lead to financial discrepancies, incorrect patient information, and delayed treatments. This section delves into common concerns, offering clarity and practical guidance on how to effectively manage the challenges that arise in this essential domain.
Common Challenges in Classification Systems
As the healthcare environment evolves, so does the complexity of categorization. Some of the most frequent issues include understanding the ever-changing regulations, dealing with intricate terminology, and ensuring proper alignment with insurance providers. Coders often face the task of interpreting ambiguous or incomplete documentation, which can further complicate the process. Maintaining consistency across various platforms and ensuring compliance with standards adds another layer of difficulty.
Practical Tips for Effective Classification
One of the most important steps to improving accuracy is ongoing education. Staying up-to-date with the latest guidelines and best practices can help professionals avoid common mistakes. Additionally, leveraging technology such as software tools designed for classification can streamline workflows, reduce human error, and increase efficiency. A thorough understanding of the nuances of each system is crucial for success, especially when working with complex patient data.
What is Healthcare Classification
In the healthcare industry, each service, procedure, and diagnosis is assigned a unique identifier. This process ensures accurate communication between medical professionals, insurance companies, and patients. By translating complex medical terminology into standardized codes, the system allows for streamlined record-keeping, billing, and reimbursement procedures. Understanding this practice is crucial for anyone involved in managing healthcare data and ensuring its proper use in administrative functions.
The Importance of Accurate Classification
Precision in assigning the right code is essential for the smooth operation of healthcare facilities. Incorrect codes can lead to payment delays, disputes with insurers, or misinterpretation of patient information. Professionals in this field must possess in-depth knowledge of both the systems used and the medical concepts they represent. Consistency and accuracy are key to maintaining the integrity of the healthcare process.
Different Types of Healthcare Codes
There are several types of codes used within the healthcare industry, each serving a specific purpose. Diagnostic codes represent the diseases or conditions a patient is diagnosed with, while procedure codes correspond to the treatments or services provided. Additionally, administrative codes are used for billing and claims processing. Familiarity with these different types is essential for anyone working with healthcare records.
Importance of Accurate Healthcare Classification
In any healthcare system, the precise assignment of identifiers to diagnoses, procedures, and services is crucial for smooth operations. The accuracy of these classifications impacts not only billing and reimbursement processes but also the quality of patient care. A small mistake in assigning the wrong code can result in delayed treatments, incorrect medical records, or even financial loss. For healthcare providers, this accuracy is an essential part of maintaining trust and compliance with regulations.
Impact on Financial Reimbursement
Accurate classification directly influences the reimbursement process between healthcare providers and insurers. If codes are misapplied, it can lead to denied claims or delayed payments. This disruption can have a significant financial impact on healthcare facilities, particularly smaller practices or hospitals that depend on timely payments for their operations. Ensuring that codes are correctly assigned helps prevent these issues, streamlining the revenue cycle.
Ensuring Patient Safety and Care Quality
Correct classification is also vital for patient safety. Accurate data ensures that healthcare providers have the most up-to-date and complete information when making clinical decisions. Misclassifications can result in inappropriate treatments or missed diagnoses, putting patients at risk. By maintaining precision in categorization, healthcare professionals can deliver better care, reducing errors and improving outcomes for patients.
Common Healthcare Classification Challenges

In the field of healthcare, professionals face several obstacles when assigning the correct identifiers to services, procedures, and diagnoses. These challenges can arise from a variety of factors, including ambiguous documentation, evolving guidelines, and complex medical terminology. Ensuring accuracy while adhering to regulatory requirements is a constant concern for individuals working with healthcare records. Understanding these challenges is crucial for improving efficiency and minimizing errors in this essential process.
Ambiguous or Incomplete Documentation
One of the most common challenges faced by healthcare professionals is dealing with vague or incomplete patient records. When documentation is unclear, it can lead to confusion regarding the proper classification of a diagnosis or procedure. This may result in incorrect coding, which can affect patient care, insurance claims, and overall operational efficiency. It’s essential for healthcare providers to ensure that their documentation is comprehensive and unambiguous to avoid these issues.
Frequent Updates to Guidelines
Healthcare classification systems are subject to frequent updates and revisions, which can create confusion for professionals who must stay current with new rules and regulations. These changes may involve modifications to the codes themselves or shifts in the way they are applied. Keeping up with these updates is vital to prevent errors and ensure compliance with industry standards. Continuous education and training are necessary to stay on top of these evolving requirements.
| Challenge | Impact | Solution |
|---|---|---|
| Ambiguous Documentation | Leads to misclassification, payment delays, and patient care errors | Ensure complete, clear, and consistent documentation from providers |
| Frequent Updates to Guidelines | Increases the risk of errors and non-compliance | Regular training and access to updated resources |
| Complex Terminology | Misunderstanding terms can result in incorrect codes | Use specialized training and reference tools |
Difference Between ICD and CPT Codes
In healthcare classification, there are various systems used to categorize procedures, diagnoses, and services. Two of the most widely used types of identifiers are the ICD and CPT systems. While both serve critical roles in the healthcare industry, they differ in purpose and application. Understanding the distinctions between these two coding systems is essential for accurate record-keeping, billing, and claims processing.
ICD Codes: Purpose and Usage
ICD codes, or International Classification of Diseases, are primarily used to describe diseases, injuries, and other health conditions. These codes are utilized to document the patient’s diagnoses and conditions, which are necessary for proper treatment and insurance purposes. Each diagnosis is assigned a unique alphanumeric code that represents a specific condition. These codes are regularly updated to reflect emerging medical knowledge and are widely adopted globally for health statistics and reporting.
CPT Codes: Purpose and Usage
CPT codes, or Current Procedural Terminology, are used to describe medical, surgical, and diagnostic services provided to patients. Unlike ICD codes, which focus on conditions, CPT codes categorize actions performed by healthcare providers, such as tests, surgeries, or treatments. These codes are essential for billing purposes, as they define the services delivered and determine reimbursement rates. CPT codes are maintained by the American Medical Association and updated annually to accommodate new procedures and technologies.
| Code Type | Purpose | Usage |
|---|---|---|
| ICD | Identifies diseases, conditions, and injuries | Used for documenting diagnoses and health statistics |
| CPT | Describes medical procedures and services | Used for billing and documenting treatments and surgeries |
How to Get Certified in Healthcare Classification
Obtaining certification in the field of healthcare classification can significantly enhance career prospects and establish credibility. This process involves a combination of education, practical experience, and successful completion of an examination. Certification not only demonstrates proficiency in the field but also opens up a wide range of employment opportunities in healthcare organizations, insurance companies, and other related sectors.
Steps to Achieving Certification
The path to certification involves several key steps that can vary depending on the certifying body and specialization. Below is an outline of the general process:
- Education: Complete a training program that covers the essential concepts and practices of healthcare classification. Many accredited institutions offer courses that prepare candidates for certification exams.
- Gain Experience: Obtain hands-on experience through internships, entry-level jobs, or volunteer opportunities. This practical exposure helps reinforce theoretical knowledge.
- Choose a Certification Exam: Select the appropriate certification based on your career goals. Popular certifications include those offered by the American Health Information Management Association (AHIMA) or the American Academy of Professional Coders (AAPC).
- Prepare for the Exam: Study relevant materials, take practice tests, and review guidelines. Many resources, including textbooks and online courses, are available to help with preparation.
- Pass the Exam: Successfully complete the certification exam to demonstrate your knowledge and competency in the field.
Types of Certifications Available
- Certified Professional Coder (CPC): Offered by AAPC, this certification is widely recognized and focuses on procedural coding.
- Certified Coding Specialist (CCS): Provided by AHIMA, this certification is ideal for individuals who wish to specialize in inpatient or outpatient coding.
- Certified Inpatient Coder (CIC): Also from AAPC, this certification focuses on coding for inpatient settings.
- Certified Outpatient Coder (COC): AAPC offers this certification for those working in outpatient facilities.
Top Healthcare Classification Resources and Tools
For professionals working in the field of healthcare classification, having access to the right resources and tools is essential for accuracy and efficiency. These resources provide comprehensive information on guidelines, codes, and industry standards, enabling individuals to stay updated and perform their tasks effectively. Below are some of the most valuable tools and references for anyone looking to enhance their expertise in this area.
Essential Reference Materials
Utilizing the following resources will help you stay informed about the latest updates, best practices, and accurate classification methods:
- ICD-10-CM/PCS Official Guidelines: The official guidelines published by the CDC provide detailed instructions on how to properly assign diagnostic and procedural codes.
- CPT Codebook: The CPT codebook, published by the American Medical Association, offers a comprehensive list of procedural codes used in healthcare. It is an essential tool for billing and reporting.
- ICD-10 Code Lookup Tools: Many online platforms provide search functions for quickly finding the correct ICD-10 codes based on symptoms, diagnoses, or procedures.
- HCPCS Level II Codebook: Used for identifying services and supplies not included in the CPT codebook, the HCPCS Level II codebook is essential for outpatient billing and Medicare services.
Online Tools and Software
In addition to printed resources, several software solutions and online tools can assist with classification tasks. These tools often feature features like code search, automated classification, and reporting functionalities:
- 3M CodeFinder: This powerful tool helps coders quickly locate the appropriate codes and stay updated on the latest coding rules.
- Optum360 EncoderPro: EncoderPro offers an easy-to-use interface for searching and selecting accurate codes, with updates reflecting the latest industry standards.
- AAPC Code Search Tool: The American Academy of Professional Coders offers an online code search platform for members, making it simple to find precise codes and guidelines.
- TruCode Encoder: TruCode provides coding professionals with a user-friendly, real-time encoding solution that helps to ensure accuracy in medical documentation.
Understanding Healthcare Classification Guidelines
Accurate classification of health conditions and procedures relies on following established rules and standards. These guidelines ensure consistency, prevent errors, and maintain compliance with healthcare regulations. By adhering to these protocols, professionals can assign the correct codes, streamline billing, and support better patient outcomes. It’s crucial for individuals working with health records to be familiar with these guidelines to ensure precision and avoid costly mistakes.
Key Aspects of Classification Guidelines
Guidelines provide detailed instructions on how to assign codes for various medical conditions, treatments, and services. Understanding these rules is fundamental for ensuring that the right identifier is used for every case. Some key elements include:
- Code Specificity: The guidelines often specify the level of detail required for each diagnosis or procedure, ensuring that coders select the most accurate and appropriate code.
- Sequencing Rules: Proper sequencing of codes is critical, as certain diagnoses must be recorded before others to reflect the correct clinical picture.
- Exclusion and Inclusion Notes: Certain codes may have exclusions or inclusions, indicating when specific codes should or should not be used together.
- Use of Modifiers: Modifiers are used to indicate a variation in a procedure or diagnosis, which may impact treatment or reimbursement.
Updating Classification Guidelines
Classification rules are not static and are frequently updated to reflect advancements in medical knowledge, changes in treatment methods, and regulatory shifts. Staying up to date with the latest revisions is critical for healthcare professionals to remain compliant and efficient in their work. Regular training, resources from certifying organizations, and access to updated coding systems are all necessary tools for keeping knowledge current.
How to Handle Coding Errors
Errors in classification can lead to incorrect billing, delayed claims, and even compliance issues. It’s important to identify, correct, and prevent these mistakes to ensure accuracy and maintain the integrity of healthcare records. Handling errors promptly and efficiently is crucial for both operational efficiency and legal compliance.
Steps to Address Errors
When an error is detected, it’s important to follow a structured process for correction. Below are the recommended steps to handle coding mistakes effectively:
| Step | Action |
|---|---|
| 1. Identification | Recognize the error through routine checks or during an audit. It could involve mismatched codes, missing modifiers, or incorrect sequencing. |
| 2. Documentation | Ensure all details of the mistake are documented, including the affected codes and the reason for the error. This helps maintain transparency and assists with future corrections. |
| 3. Correction | Amend the incorrect codes and submit the revised claim. This may involve resubmitting the claim to insurance providers or updating patient records. |
| 4. Follow-up | Monitor the revised claims or patient records to ensure the issue is resolved and no further issues arise. |
| 5. Prevention | Implement measures such as additional training, automated checks, or enhanced review processes to reduce the likelihood of future mistakes. |
Common Causes of Errors
Understanding the common reasons behind errors can help in avoiding them in the future. Some frequent causes include:
- Incomplete or outdated reference materials
- Misinterpretation of clinical notes or physician documentation
- Improper training or lack of familiarity with guidelines
- Rushed or inadequate review processes
By taking a proactive approach to identifying, correcting, and preventing errors, healthcare professionals can improve accuracy and ensure smoother operations across the board.
Healthcare Classification and Insurance Claims
Accurate classification plays a vital role in the submission of insurance claims. Correctly identifying conditions, procedures, and services ensures that the proper reimbursements are processed without delays or errors. Insurers rely heavily on well-defined classification to determine coverage, reimbursement rates, and the appropriateness of the submitted treatments. A misunderstanding or mistake in this process can lead to claim rejections, delays, and even legal complications.
Impact on Claim Reimbursement
Insurance companies use the classifications submitted with claims to assess the medical necessity, appropriateness, and cost of the treatments provided. Accurate coding is essential for timely reimbursement. Misclassifications can lead to the following issues:
- Delayed Payments: Incorrect classifications may cause insurance companies to request additional documentation or clarify coding, resulting in delayed reimbursements.
- Claim Denials: Some insurers might outright deny a claim if the submitted codes do not align with their guidelines or expectations.
- Underpayments or Overpayments: Incorrectly selected codes can either reduce the amount reimbursed or cause overpayments, leading to potential audits and penalties.
Best Practices for Submission
To avoid issues with insurance claims, healthcare professionals should adhere to the following best practices:
- Ensure Code Accuracy: Always verify that the codes used accurately represent the diagnosis or procedure performed. Double-check the most up-to-date coding manuals or software.
- Understand Insurance Requirements: Familiarize yourself with the specific coding and documentation guidelines of different insurance providers.
- Utilize Electronic Systems: Automated coding systems help streamline the submission process and reduce human error.
- Stay Informed: Regular training and education on the latest classification updates, payer policies, and regulatory changes will ensure continued accuracy.
By maintaining a strong understanding of both healthcare classification and insurance requirements, providers can improve the efficiency of claims processing and ensure accurate reimbursements.
What is a Coding Audit
A review process to examine the accuracy of assigned classifications plays a crucial role in ensuring that healthcare records and claims are properly documented and compliant with regulatory standards. This evaluation helps identify potential errors, inconsistencies, or gaps that could affect reimbursement or lead to non-compliance. The audit process is integral for maintaining the integrity of the healthcare documentation system and preventing financial losses.
Purpose of a Coding Audit
Audits are conducted to ensure that the assigned codes accurately reflect the diagnoses, treatments, and services provided. The main objectives of this process include:
- Identifying Errors: Detecting mistakes in code selection, sequencing, or the use of modifiers to avoid incorrect billing and reimbursements.
- Improving Accuracy: Ensuring that all records are properly classified, which leads to accurate billing and fewer claims rejections.
- Compliance Assurance: Verifying that the classifications align with regulatory standards, payer guidelines, and internal protocols.
- Reducing Financial Risk: Minimizing the risk of audits, fines, or penalties due to incorrect classifications or fraudulent submissions.
Steps in Conducting a Coding Audit
Performing an audit requires a methodical approach to reviewing records and classifications. Common steps include:
- Selection of Sample Cases: A random or targeted selection of claims or patient records is made for review.
- Review of Documentation: The healthcare records, including physician notes and test results, are analyzed for accuracy and completeness.
- Verification of Code Assignment: The chosen codes are compared against the documentation to confirm that they align with the diagnoses and procedures described.
- Reporting Findings: The results of the audit, including any discrepancies or issues identified, are compiled into a detailed report.
- Corrective Actions: Based on the audit results, adjustments are made to the coding practices to address errors or improve accuracy.
Regular audits help maintain high standards in healthcare classification, leading to better financial outcomes, improved accuracy, and enhanced compliance.
How to Choose the Right Classification Specialization
Selecting the appropriate area of focus in the field of healthcare classification is a significant decision for professionals looking to build their careers. Different specialties require unique sets of skills and knowledge. Understanding the scope of each specialty can help individuals make an informed choice that aligns with their interests, strengths, and career goals.
Factors to Consider When Choosing a Specialization
When deciding on a specific area of expertise, consider the following key factors:
- Interest and Passion: Choose a field that sparks your interest, as this will motivate you to stay engaged and continue learning in the long term.
- Job Market Demand: Evaluate the demand for specific specialties in your area. Some fields may have more job opportunities due to industry needs.
- Skill Set: Different specialties require different skills, such as knowledge of particular procedures or systems. Choose one that aligns with your strengths.
- Salary Potential: Some classifications, such as inpatient or outpatient coding, may offer higher pay rates depending on the complexity and responsibilities of the role.
- Work Environment: Certain specialties may involve more direct interaction with healthcare providers or patients, while others may be more office-based or administrative in nature.
Popular Specializations to Explore
There are several key areas within healthcare classification that professionals can pursue, including:
- Inpatient Classification: Focuses on coding for patients admitted to a hospital for an extended period.
- Outpatient Classification: Deals with services provided to patients who are not admitted to a hospital but require treatments or procedures.
- Emergency Department Classification: Specializes in coding for emergency room visits and related treatments.
- Physician’s Office Classification: Involves coding for services provided in a doctor’s office, such as consultations or minor procedures.
- Pathology Classification: Focuses on coding for laboratory services and pathology reports.
By evaluating your personal preferences, skills, and the market demand, you can select the right area to specialize in, leading to a fulfilling and successful career in the field.
Classification for Hospitals vs Clinics
The process of assigning codes to healthcare services differs significantly between large hospitals and smaller outpatient clinics. While both settings involve the documentation and classification of patient care, the complexity, types of services, and coding requirements can vary greatly. Understanding the distinctions between these environments is crucial for professionals in this field.
Key Differences Between Hospitals and Clinics
Several factors contribute to the differences in classification practices for hospitals and clinics:
- Service Complexity: Hospitals typically offer a wider range of complex services, including emergency care, surgeries, and long-term treatments, which require more detailed coding.
- Patient Length of Stay: In hospitals, patients are often admitted for extended periods, which means coding for multiple procedures and diagnoses over a longer time span. In contrast, clinic visits are usually short-term, involving a single consultation or procedure.
- Volume of Cases: Hospitals often handle a higher volume of cases, leading to an increased number of codes assigned. Clinics, on the other hand, see fewer patients and have a lower volume of claims to process.
- Insurance and Billing: Hospitals often deal with more complex billing and insurance claims due to the diversity of services provided. Clinics may focus on simpler, outpatient claims that are more straightforward.
Specific Considerations for Each Setting
In both environments, professionals need to be familiar with the specific needs and regulations:
- Hospitals: Requires in-depth knowledge of inpatient coding, ICD codes for diseases, and procedures related to surgeries, diagnostics, and prolonged care.
- Clinics: Primarily involves outpatient coding for simpler diagnoses, minor procedures, and routine consultations. Familiarity with office visit codes and preventative care services is key.
In summary, although both hospitals and clinics require accurate classification practices, the differences in patient care complexity, service types, and volume highlight the need for specialized knowledge in each setting.
Impact of Technology on Healthcare Classification
Advancements in technology have revolutionized many industries, and the healthcare sector is no exception. The methods used to assign codes for medical procedures, diagnoses, and patient care have seen significant changes thanks to innovations in software, automation, and data management. These developments have both streamlined the process and introduced new challenges for professionals in the field.
With the introduction of electronic health records (EHR) and automated systems, coding accuracy has improved, but so has the complexity of managing vast amounts of data. The integration of artificial intelligence (AI) and machine learning tools is enhancing the speed and efficiency of coding, yet it also requires that healthcare professionals stay updated with new technologies and training.
Benefits of Technological Advancements
- Increased Efficiency: Automation tools reduce the time needed for manual data entry, making the entire process faster and reducing the risk of human error.
- Improved Accuracy: Advanced systems can quickly cross-reference codes with patient data, improving the overall accuracy of classifications and billing.
- Better Integration: Technology allows for seamless integration of patient information across different departments, improving communication and reducing duplication of services.
- Enhanced Training Tools: Interactive software and AI-based training programs offer healthcare professionals an efficient way to stay updated with coding rules and regulations.
Challenges Presented by Technology
However, with the benefits come several challenges that need to be addressed:
- Data Security: As more healthcare providers rely on digital systems, there is an increased risk of data breaches and cyberattacks, necessitating stringent security protocols.
- Training Requirements: The introduction of new tools requires coders to undergo continuous training to remain proficient with the latest technologies and coding standards.
- System Failures: Relying on technology means that system outages or technical glitches can disrupt the coding process, potentially delaying billing and claims submissions.
Overall, technology has greatly improved the efficiency and accuracy of healthcare classification systems. However, it requires constant updates and proper implementation to fully realize its potential and avoid unintended disruptions in the coding process.
| Technology Impact | Benefit | Challenge |
|---|---|---|
| Automation | Faster processing times | Need for ongoing training |
| Artificial Intelligence | Improved accuracy of codes | Complex system integration |
| Electronic Health Records (EHR) | Seamless data sharing | Data privacy concerns |
Best Practices for Healthcare Classification Professionals
For individuals working with healthcare classification, following industry best practices is essential to ensure accuracy, efficiency, and compliance with regulatory standards. Implementing the right strategies helps to minimize errors, enhance productivity, and contribute to a smooth workflow. These practices guide professionals in maintaining high-quality work while staying updated with the ever-evolving healthcare landscape.
One key practice is the consistent use of official coding manuals and guidelines. These resources help ensure that each procedure or diagnosis is assigned the correct code, reducing the chance of inaccuracies. It’s also crucial to review the latest updates regularly to stay informed of changes in the coding systems.
Tips for Healthcare Classification Professionals
- Double-check everything: Always verify the details of each patient’s records and ensure the correct codes are applied to avoid discrepancies.
- Stay updated: Regularly attend training sessions, workshops, or webinars to stay current with changes in codes and rules.
- Organize your workspace: A clean and organized workspace helps improve focus and reduces the likelihood of overlooking important information.
- Use technology to your advantage: Leverage automated systems and tools to streamline tasks and increase accuracy. Ensure proper system backups to avoid data loss.
- Collaborate with other professionals: Foster communication with healthcare providers to clarify any ambiguous cases, ensuring accuracy in coding and billing processes.
Common Mistakes to Avoid
- Misunderstanding the codes: Ensure you understand the context of the procedure or diagnosis before assigning a code to avoid misclassification.
- Ignoring updates: Outdated codes or missed revisions can lead to compliance issues, so always check for updates in relevant manuals or systems.
- Skipping audits: Regular internal audits can help identify and correct errors before they become significant problems.
By adopting these best practices, healthcare classification professionals can maintain high standards of accuracy and efficiency, contributing to the overall effectiveness of the healthcare system.
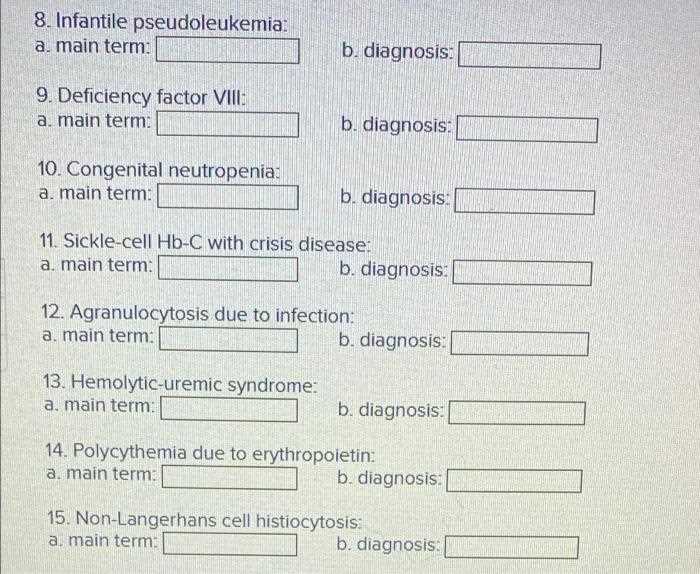
Challenges in Pediatric Coding
When it comes to classifying healthcare procedures for children, there are a variety of unique obstacles that professionals face. These challenges stem from the complexity of pediatric care, which often involves specialized diagnoses and treatments that differ from those in adult healthcare. The variability in age, development, and medical conditions in children adds layers of complexity when assigning appropriate classification codes.
One major issue is the age-related variation in diagnoses. As children grow, their healthcare needs evolve, leading to codes that may differ significantly depending on the patient’s age group. This makes it essential for professionals to be extremely precise in identifying the correct codes for conditions that may manifest differently in infants, toddlers, or adolescents.
Common Obstacles in Pediatric Classification
- Age-specific diagnosis codes: Accurate classification requires a deep understanding of how diseases and conditions present in different age groups, which may vary from one stage of childhood to another.
- Complex medical conditions: Pediatric patients often have complex, multisystem conditions that require nuanced coding, making it challenging to select the correct codes for both rare and common conditions.
- Frequent updates: Pediatric codes often change more frequently due to new research, therapies, and evolving standards, making it essential to stay up to date with the latest revisions.
Solutions to Overcome Challenges

- Continuous training: It is vital to participate in ongoing educational opportunities to stay informed about the latest pediatric healthcare guidelines and classifications.
- Collaboration with healthcare providers: Regular communication with pediatricians and specialists can help clarify complex cases and ensure the accurate use of codes.
- Utilizing advanced tools: Implementing software designed to handle pediatric cases can streamline the process, improving efficiency and reducing human error.
Addressing these challenges is critical for ensuring accurate classification in pediatric care, which, in turn, ensures proper treatment and appropriate reimbursement for services provided to young patients.
How to Stay Updated on Coding Changes
As the healthcare field evolves, so too do the rules and guidelines for classifying medical procedures and diagnoses. Staying informed about these changes is crucial for professionals to ensure accuracy and compliance in their work. Failure to do so may result in coding errors, leading to delays, denied claims, and even legal issues. It is essential to adopt strategies that keep you up to date with the latest revisions and developments in classification systems.
Key Strategies for Staying Informed
- Subscribe to Industry Newsletters: Many organizations offer newsletters and updates on changes in healthcare classification systems. These resources provide timely information on new guidelines, codes, and best practices.
- Join Professional Associations: Becoming a member of industry associations such as the American Health Information Management Association (AHIMA) or the American Academy of Professional Coders (AAPC) provides access to webinars, workshops, and publications that highlight code changes.
- Regularly Review Official Guidelines: Ensure that you frequently consult official documents, such as updates from the Centers for Medicare & Medicaid Services (CMS) or the World Health Organization (WHO), to stay aligned with industry standards.
Leverage Technology for Continuous Learning
- Use Specialized Software: Many software tools are designed to integrate the latest changes into their databases. These platforms help automate the process of updating codes and guidelines, making it easier for professionals to stay current.
- Participate in Webinars and Online Courses: Numerous online resources offer virtual learning opportunities. These platforms are often updated with the latest changes, providing professionals with direct access to expert advice and analysis.
- Follow Social Media and Forums: Many industry experts and organizations actively share insights on social media platforms. Engaging in online communities allows professionals to interact with peers and experts, sharing tips and staying informed about the latest trends.
By utilizing these strategies, professionals can stay on top of frequent changes in classification standards, ensuring they provide the best possible service while maintaining compliance with evolving regulations.
Future of Medical Coding Careers
The landscape of healthcare administration is continuously shifting, with emerging technologies, regulations, and industry trends playing a major role in shaping the future. Professionals in the field of procedure and diagnosis classification are essential to maintaining the integrity of medical records and ensuring proper reimbursement. As the healthcare sector evolves, so does the demand for skilled individuals capable of adapting to new challenges and advancing their expertise in this critical area.
Growth Opportunities in a Changing Landscape
With the rise of electronic health records (EHR) and health information technology, the need for precise and up-to-date classification systems has grown exponentially. As healthcare systems around the world increasingly rely on automation and data-driven decisions, there will be a continued demand for professionals who can bridge the gap between technology and patient care. This will result in an expansion of job opportunities and specializations within the field.
- Specialized Roles: The future may see an increased focus on niche areas, such as pediatric, orthopedic, or mental health classification. Professionals with expertise in these specific fields will be in high demand to ensure accuracy and compliance.
- Technology Integration: As AI and machine learning continue to transform the healthcare industry, coding professionals will likely need to work alongside advanced technologies to ensure the accuracy of data and support decision-making processes.
- Remote Work Flexibility: The rise of telehealth and remote patient monitoring will lead to more remote opportunities for those working in classification, providing greater flexibility and access to professionals across different regions.
Adapting to Industry Innovations
In addition to expanding specialization areas, the field will also require ongoing professional development and adaptation to technological advancements. Certification programs, workshops, and specialized training will play a key role in preparing individuals for the future. Professionals will need to stay updated with the latest guidelines, changes in regulations, and best practices to stay competitive in a rapidly evolving environment.
- Continual Learning: As coding standards and healthcare policies continue to evolve, staying ahead of these changes will be crucial for long-term career success.
- Data Analytics Expertise: Understanding data analysis and reporting tools will become increasingly important, as healthcare organizations use this data to optimize patient care and improve financial outcomes.
The future of this profession promises a wealth of opportunities, with continued technological advancements and increasing demand for skilled professionals. Embracing change, learning new skills, and specializing in emerging areas will ensure success in the evolving landscape of healthcare administration.