In emergency situations, quick and accurate decision-making is crucial to saving lives, especially when dealing with children. This section will help you prepare for the certification required to respond effectively to pediatric emergencies. It covers essential topics, from basic life-saving techniques to advanced medical interventions, ensuring you understand the concepts needed to perform well in real-world scenarios.
Through an exploration of key principles, this guide provides the necessary knowledge to approach various medical situations involving children. Understanding the protocols, methods, and actions that should be taken in critical moments will improve your ability to provide timely and effective care. Whether you are aiming to pass your certification or enhance your skills, this content is designed to support your learning journey.
Pediatric Life Support Evaluation Preparation
Preparing for a pediatric emergency care assessment involves understanding core concepts, techniques, and scenarios that are critical in providing effective medical interventions to children. A thorough review of key material, from managing cardiac arrests to addressing respiratory issues, will help ensure that you are ready for any situation that may arise in a clinical setting.
Core Areas of Focus
- Early identification of life-threatening conditions
- Effective airway management and breathing support
- Cardiopulmonary resuscitation (CPR) and defibrillation procedures
- Medications used in pediatric emergencies
- Effective communication within a healthcare team
Common Scenarios for Review
- Child experiencing respiratory distress or failure
- Cardiac arrest in a pediatric patient
- Shock management and fluid resuscitation
- Emergency medication dosages and routes
- Post-resuscitation care and reassessment
By focusing on these core areas and reviewing common emergency scenarios, you can ensure that you are well-equipped to perform under pressure and respond swiftly to pediatric medical emergencies. Understanding these key elements will allow you to demonstrate competence and confidence during your evaluation process.
Overview of Pediatric Advanced Life Support Certification
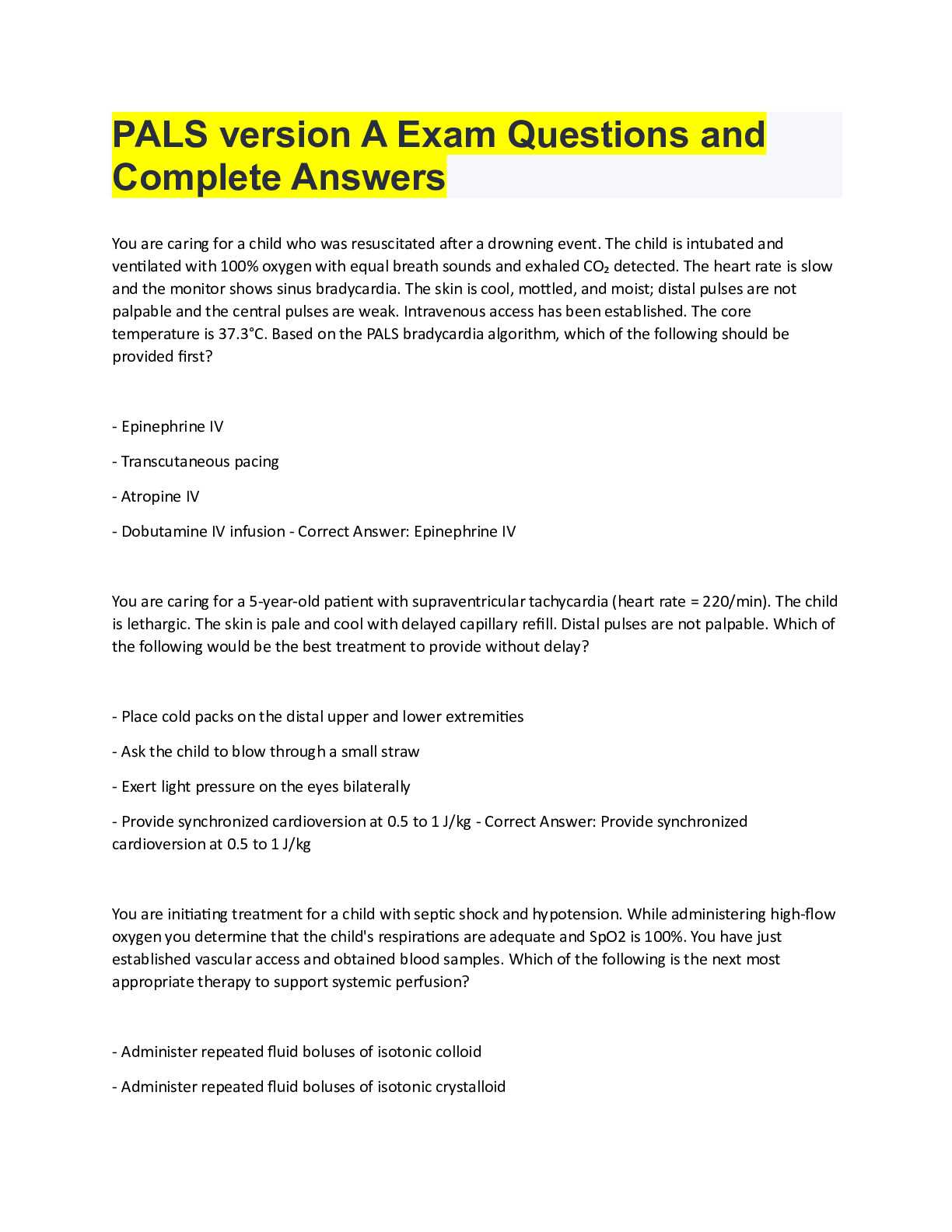
Achieving certification in pediatric emergency care is a crucial step for healthcare professionals aiming to provide life-saving interventions for children in critical situations. This process ensures that individuals are trained in essential techniques and protocols to respond effectively to medical emergencies involving children, from cardiac arrest to respiratory distress. The certification process is designed to validate both theoretical knowledge and practical skills in handling pediatric emergencies.
Key Components of Certification
- Understanding pediatric resuscitation guidelines
- Mastery of airway management techniques
- Proficiency in defibrillation and medication administration
- Effective teamwork and communication in emergency settings
- Assessment and management of pediatric shock and arrest scenarios
Who Should Pursue Certification
- Pediatricians and family medicine doctors
- Emergency medical technicians (EMTs)
- Nurses working in pediatric care or emergency departments
- Paramedics and other healthcare professionals involved in critical care
Obtaining certification is an essential qualification for those working in pediatric emergency care, ensuring that they possess the knowledge and ability to act quickly and efficiently during urgent medical situations. The process equips professionals with the skills needed to manage complex pediatric emergencies while adhering to best practices and clinical guidelines.
Key Concepts in Pediatric Advanced Life Support
In pediatric emergency care, there are several fundamental principles that form the backbone of effective treatment in life-threatening situations. These concepts include early recognition of critical conditions, appropriate response methods, and the use of specific techniques to stabilize young patients. Mastering these key areas is essential for healthcare providers to ensure the best possible outcomes in emergencies involving children.
The ability to act swiftly and correctly is paramount, as the physiological differences in children require tailored approaches compared to adults. Properly managing airway issues, administering medications, and performing resuscitation techniques are just a few examples of the essential skills that must be mastered to effectively handle pediatric emergencies.
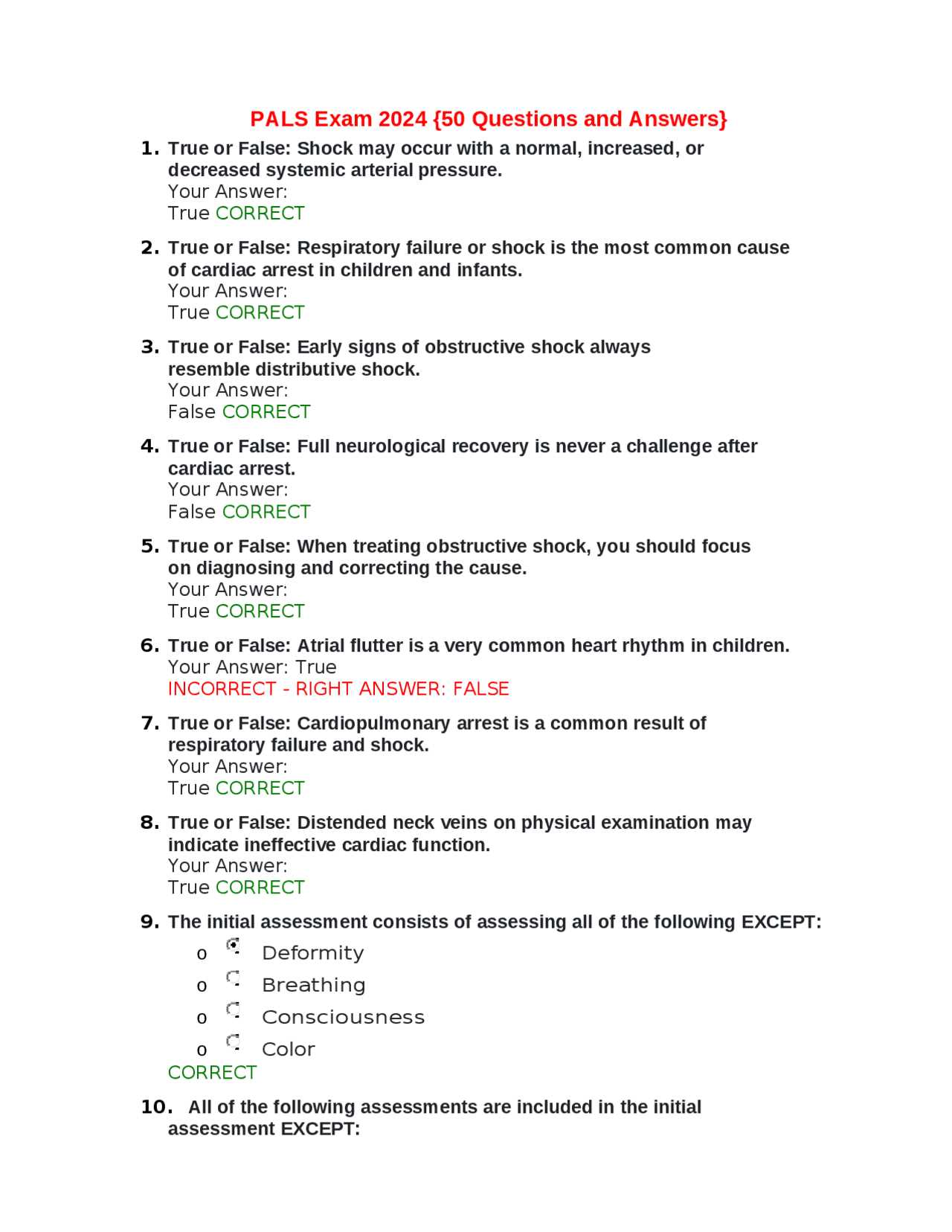
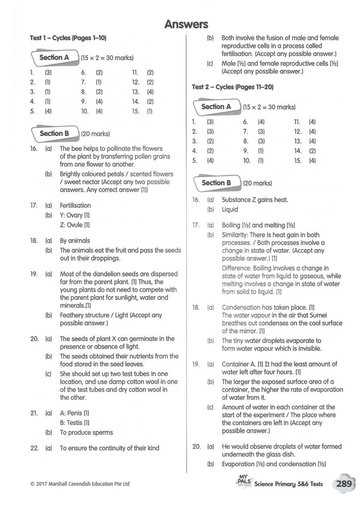
Commonly Asked Pediatric Emergency Care Scenarios
During the evaluation process for pediatric emergency care, certain topics and scenarios tend to be emphasized more frequently. These common situations typically test a healthcare professional’s ability to apply critical concepts in real-life emergencies. Understanding these areas is key to demonstrating competence and readiness to handle pediatric emergencies effectively.
Below are some of the most frequently encountered situations that are examined during the evaluation process. Mastering the response to these scenarios will help ensure that you are well-prepared to manage critical situations involving children in various stages of medical distress.
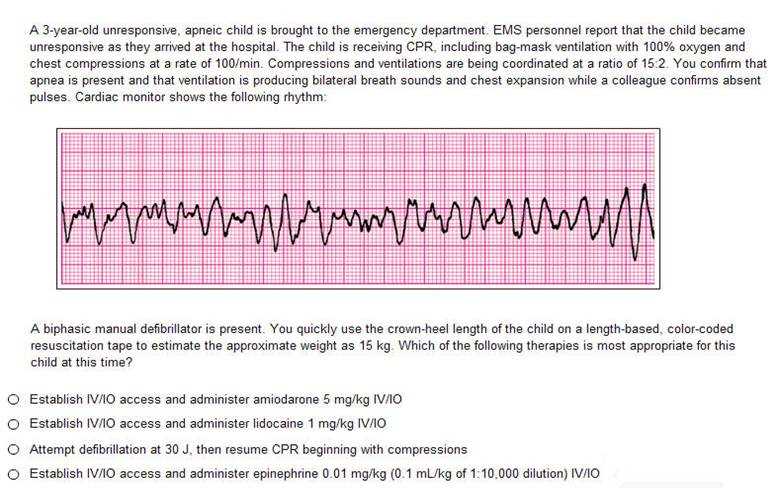
Understanding Pediatric Cardiac Arrest Scenarios
In pediatric emergencies, cardiac arrest is one of the most critical and time-sensitive situations that healthcare professionals must be prepared for. Recognizing the signs of a child in cardiac distress and responding appropriately can make the difference between life and death. This section focuses on the essential steps and considerations for managing a pediatric patient experiencing cardiac arrest.
Signs of Cardiac Arrest in Children
- Sudden loss of consciousness
- Absence of normal breathing or irregular gasping
- Unresponsiveness to stimuli
- Weak or absent pulse
Key Interventions for Pediatric Cardiac Arrest
- Immediate CPR: Initiate chest compressions and rescue breaths to maintain circulation and oxygenation.
- Defibrillation: Use a defibrillator when appropriate to restore normal heart rhythm.
- Medication: Administer emergency drugs, such as epinephrine, to support cardiovascular function.
- Advanced Airway Management: Secure an airway and provide ventilation support if needed.
Each step in the management of a child in cardiac arrest must be carried out swiftly and with precision. The key to success in these high-pressure situations lies in early recognition and prompt action, along with ongoing assessment of the patient’s condition throughout the process.
Importance of Early Recognition in Pediatric Emergency Care
In pediatric emergencies, early recognition of life-threatening conditions plays a vital role in improving patient outcomes. Identifying signs of distress or deterioration in a child as soon as possible allows healthcare providers to initiate the appropriate interventions quickly. Delays in recognition or action can lead to irreversible damage and significantly decrease the chances of survival. The ability to assess and act swiftly is essential in saving lives and preventing long-term complications.
Key Signs to Recognize Early
| Condition | Early Indicators | Recommended Action |
|---|---|---|
| Respiratory Distress | Rapid breathing, wheezing, nasal flaring, and cyanosis | Administer oxygen and support ventilation |
| Shock | Pale or mottled skin, weak pulse, rapid heart rate | Fluid resuscitation and monitoring of vital signs |
| Cardiac Arrest | Unresponsiveness, absent pulse, irregular or absent breathing | Initiate chest compressions and defibrillation |
Benefits of Early Intervention

Recognizing the signs of distress early on not only improves the chances of survival but also reduces the potential for long-term complications. Early intervention helps stabilize the child’s condition, allows for timely medication administration, and prepares the healthcare team for the next steps in treatment. In critical care, seconds matter, and being proactive is essential in achieving positive outcomes.
Airway Management in Pediatric Emergency Care
Effective airway management is a critical component in the care of children experiencing respiratory distress or failure. Securing the airway ensures that oxygen can reach the lungs and is essential for stabilizing the patient. In pediatric emergency care, a variety of techniques and tools are available to manage and maintain a clear airway, depending on the severity of the situation. Understanding these techniques and when to apply them is vital for healthcare providers during critical interventions.
Common Airway Techniques
| Technique | Indication | Key Considerations |
|---|---|---|
| Head-Tilt, Chin-Lift | Unresponsive patient with no suspected spinal injury | Ensure proper alignment to open the airway |
| Jaw-Thrust | Unresponsive patient with possible cervical spine injury | Use without tilting the head to avoid spinal movement |
| Endotracheal Intubation | Severe respiratory distress, inadequate oxygenation | Requires advanced skills and equipment |
| Oropharyngeal Airway | For unconscious patients with no gag reflex | Measure for correct size to avoid trauma |
Monitoring and Maintaining the Airway
Once the airway is secured, continuous monitoring is necessary to ensure it remains open and that the child is receiving adequate oxygen. Healthcare providers should be prepared to adjust their interventions based on the patient’s response, including repositioning or using additional airway devices as needed. Regular assessment of breathing patterns, pulse oximetry readings, and overall patient condition are essential for maintaining the airway and preventing further complications.
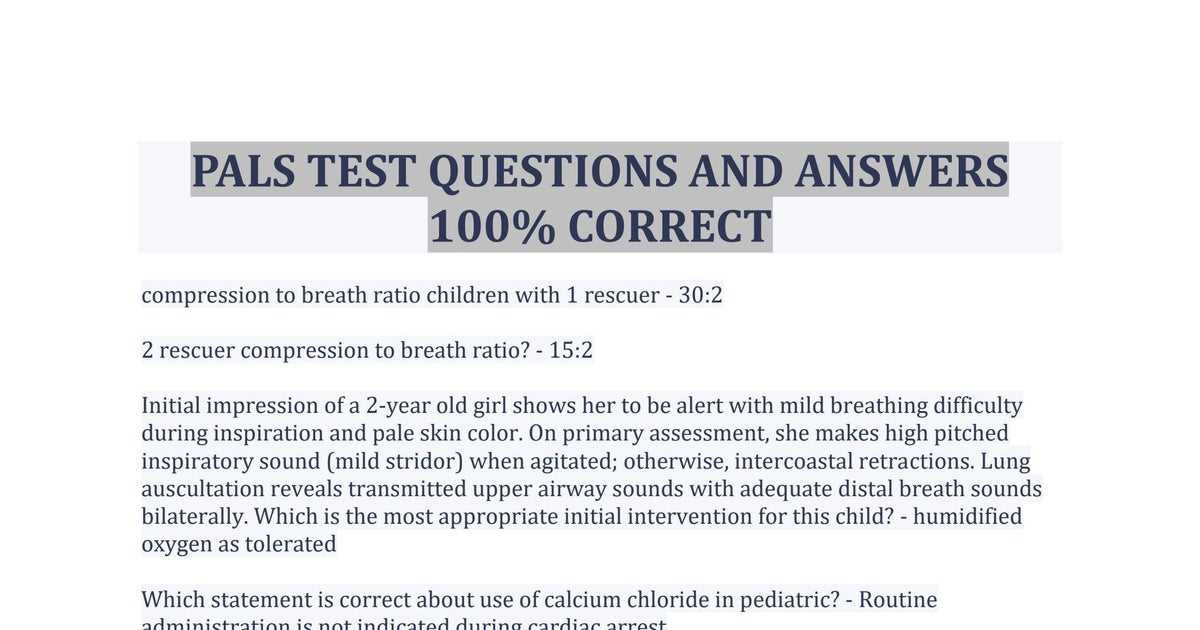
Effective CPR Techniques for Children
When a child experiences cardiac arrest, immediate action is crucial to improve their chances of survival. Cardiopulmonary resuscitation (CPR) is the most effective method to maintain circulation and oxygenation until more advanced care can be provided. However, performing CPR on children requires specific techniques that differ from those used in adults due to their smaller size and different physiological needs. Mastery of these techniques is essential for healthcare professionals and anyone trained to respond to emergencies involving children.
Steps for Performing Chest Compressions
- Positioning: Place the child on a firm, flat surface. For infants, use two fingers at the center of the chest, just below the nipple line. For older children, use one or two hands depending on the child’s size.
- Compression Depth: Compress the chest at least one-third the depth of the chest (about 1.5 inches for infants, 2 inches for children).
- Compression Rate: Perform compressions at a rate of 100-120 per minute.
- Allow Full Recoil: Ensure that the chest fully rises between compressions to allow the heart to refill with blood.
Rescue Breaths and Airway Management
- Airway Open: Use the head-tilt, chin-lift maneuver to open the airway. For infants, avoid tilting the head too far back.
- Rescue Breaths: After every 30 compressions, provide two rescue breaths. Ensure the chest rises with each breath to confirm adequate ventilation.
- Breathing Rate: Deliver 2 breaths after every 30 compressions. For infants, use a gentle breath, covering both the nose and mouth with your mouth. For older children, provide a regular-size breath.
Effective CPR requires not only the right technique but also the ability to adapt quickly to the child’s response. Continuously assess the situation and be prepared to adjust your approach if necessary. Early and correct intervention can significantly increase the chances of survival and recovery for a child experiencing cardiac arrest.
Advanced Ventilation Methods in Pediatric Emergencies
When a child is in respiratory distress or failure, providing adequate ventilation is essential for maintaining oxygen levels and preventing further complications. In certain situations, advanced techniques are necessary to ensure effective airway management and respiratory support. These methods require specialized knowledge and training, and are crucial for healthcare providers responding to severe cases of respiratory compromise in children. Understanding when and how to use these techniques can greatly improve outcomes in pediatric emergencies.
Advanced Techniques for Effective Ventilation
- Bag-Valve Mask (BVM) Ventilation: This technique involves using a self-expanding bag connected to a mask that covers the child’s mouth and nose, allowing the healthcare provider to deliver positive pressure ventilation. It is especially useful when the child cannot breathe on their own.
- Endotracheal Intubation: In cases of severe respiratory failure, intubation may be necessary to secure the airway and provide continuous ventilation. This technique requires advanced skills and appropriate equipment to place a tube in the trachea and ensure proper ventilation.
- Supraglottic Airway Devices: These devices are an alternative to endotracheal intubation when rapid or difficult intubation is anticipated. They are placed above the glottis and provide a clear airway for delivering oxygen and ventilation.
Indications for Advanced Ventilation
- Inability to Maintain Oxygenation: If a child’s oxygen levels are low despite basic airway management and supplemental oxygen, advanced techniques may be needed.
- Inadequate Spontaneous Breathing: When a child is unable to maintain adequate breathing on their own, mechanical ventilation through advanced methods can support their respiratory needs.
- Airway Obstruction: In cases of severe airway obstruction, advanced interventions such as intubation or supraglottic airway devices may be required to bypass the obstruction and restore normal breathing.
Advanced ventilation methods are vital tools in pediatric emergency care, especially in life-threatening situations. Mastery of these techniques allows healthcare professionals to respond quickly and effectively, improving the child’s chances of survival and recovery.
Pharmacological Interventions in Pediatric Emergencies
In critical pediatric situations, the use of medications is a key component of effective treatment. Pharmacological interventions can support vital functions such as circulation, breathing, and neurological activity, especially when the child’s condition deteriorates rapidly. Administering the right medications at the right time can significantly impact outcomes in emergency scenarios. Healthcare providers must be knowledgeable about the various drugs available, their indications, dosages, and potential side effects in order to provide optimal care during pediatric emergencies.
Common Medications and Their Uses
- Adrenaline (Epinephrine): Often used during cardiac arrest or severe anaphylactic reactions, adrenaline stimulates the heart and improves blood flow to vital organs.
- Atropine: Used to treat bradycardia (slow heart rate), atropine increases the heart rate by blocking parasympathetic influences on the heart.
- Amiodarone: This medication is used in cases of ventricular arrhythmias, providing electrical stability to the heart and reducing abnormal heart rhythms.
- Dextrose: For children suffering from hypoglycemia (low blood sugar), dextrose helps rapidly raise blood glucose levels and prevent further neurological damage.
Considerations When Administering Medications
- Dosage Adjustments: Children require age-appropriate doses, which can vary significantly from adult recommendations. Accurate weight measurement is essential for calculating the correct dose.
- Potential Drug Interactions: Care must be taken to avoid interactions between medications, as some drugs can amplify or diminish the effects of others.
- Side Effects and Monitoring: All medications carry potential side effects, and it’s important to monitor the child closely for any adverse reactions, especially when treating acute conditions.
Understanding pharmacological interventions and their proper administration is essential for managing pediatric emergencies effectively. Healthcare providers must be equipped with the knowledge to make quick, informed decisions in order to provide the best care possible for critically ill or injured children.
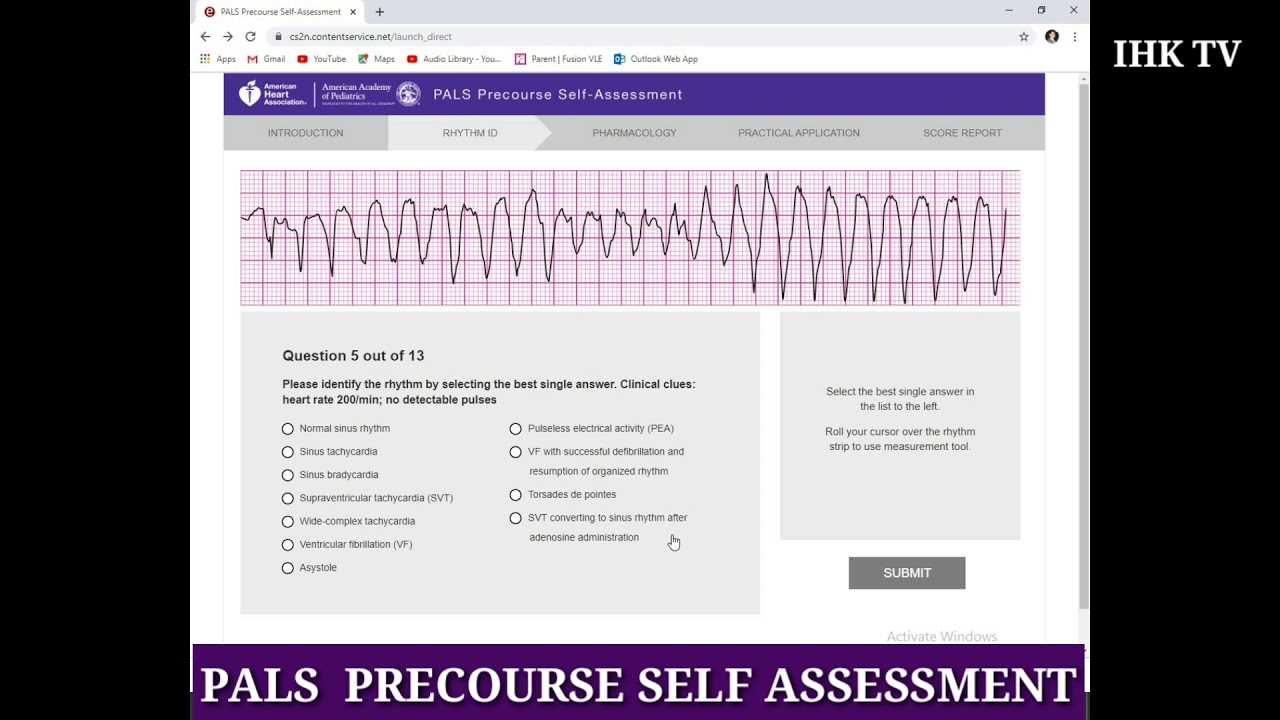
Interpretation of Pediatric ECG Strips
Reading and understanding ECG strips for children is a vital skill for healthcare providers. It involves evaluating the electrical activity of the heart to detect irregularities in rhythm, rate, and overall cardiac function. Unlike adults, pediatric ECGs display unique patterns due to differences in heart size, rate, and development. Being able to interpret these patterns accurately ensures timely interventions for children experiencing cardiac events.
Key Features in Pediatric ECG Interpretation
- Heart Rate: Children’s heart rates are generally faster than those of adults, and the normal range varies with age. Identifying the expected heart rate for a child’s age is key to distinguishing normal rhythms from abnormal ones.
- PR Interval: The PR interval measures the time taken for the electrical signal to travel from the atria to the ventricles. This interval tends to be shorter in children, but any deviations could indicate conduction problems.
- QRS Complex: The QRS complex represents the electrical impulse as it travels through the ventricles. Prolonged or abnormal QRS durations may indicate potential conduction issues.
- QT Interval: The QT interval measures the time it takes for the heart muscle to contract and relax. An extended QT interval can signal the potential for life-threatening arrhythmias.
Common Abnormalities in Pediatric ECG Strips
- Sinus Tachycardia: An elevated heart rate, often caused by fever, stress, or dehydration. This condition is usually not dangerous, but it must be distinguished from other forms of arrhythmia.
- Bradycardia: A slower-than-normal heart rate, often related to excessive vagal tone or systemic conditions such as hypoxia. Severe bradycardia may require immediate attention.
- Supraventricular Tachycardia (SVT): A rapid heart rate originating in the atria, which can cause symptoms such as dizziness and fainting. Prompt treatment is necessary to prevent complications.
- Ventricular Tachycardia (VT): A dangerous arrhythmia originating in the ventricles, which can lead to cardiac arrest if not treated immediately.
For pediatric patients, accurately interpreting ECG strips is essential for identifying life-threatening conditions quickly. Proper analysis can guide healthcare professionals in delivering effective treatments and improving patient outcomes.
Responding to Shock in Children
Shock in pediatric patients is a critical condition that requires immediate attention to prevent organ failure and other severe complications. It occurs when the circulatory system fails to deliver enough oxygenated blood to the body’s organs and tissues, leading to impaired function. Recognizing the early signs and understanding the appropriate steps for treatment can significantly improve outcomes in children suffering from shock.
Signs of Shock in Pediatric Patients
- Rapid Heart Rate: An elevated heart rate is a common early response to reduced blood volume or poor circulation.
- Pale or Cool Skin: Poor perfusion can cause the skin to become pale, cold, or clammy to the touch, particularly in the extremities.
- Weak Pulse: The pulse may feel weak or difficult to detect, especially in peripheral areas such as the wrists or ankles.
- Decreased Blood Pressure: A drop in blood pressure, although often a late sign in children, can indicate severe shock or progressing organ failure.
- Altered Mental Status: A child in shock may become restless, confused, or lethargic due to poor blood flow to the brain.
Management of Shock in Children
Effective management of shock requires a systematic approach to address the underlying cause and stabilize the child. The following steps are essential in responding to shock:
- Early Identification: The first step in managing shock is recognizing its signs and differentiating it from other potential conditions. Early intervention is crucial for preventing deterioration.
- Airway and Breathing Support: Ensuring that the airway is open and the child is breathing effectively is paramount. Administering oxygen may be necessary to improve oxygen saturation.
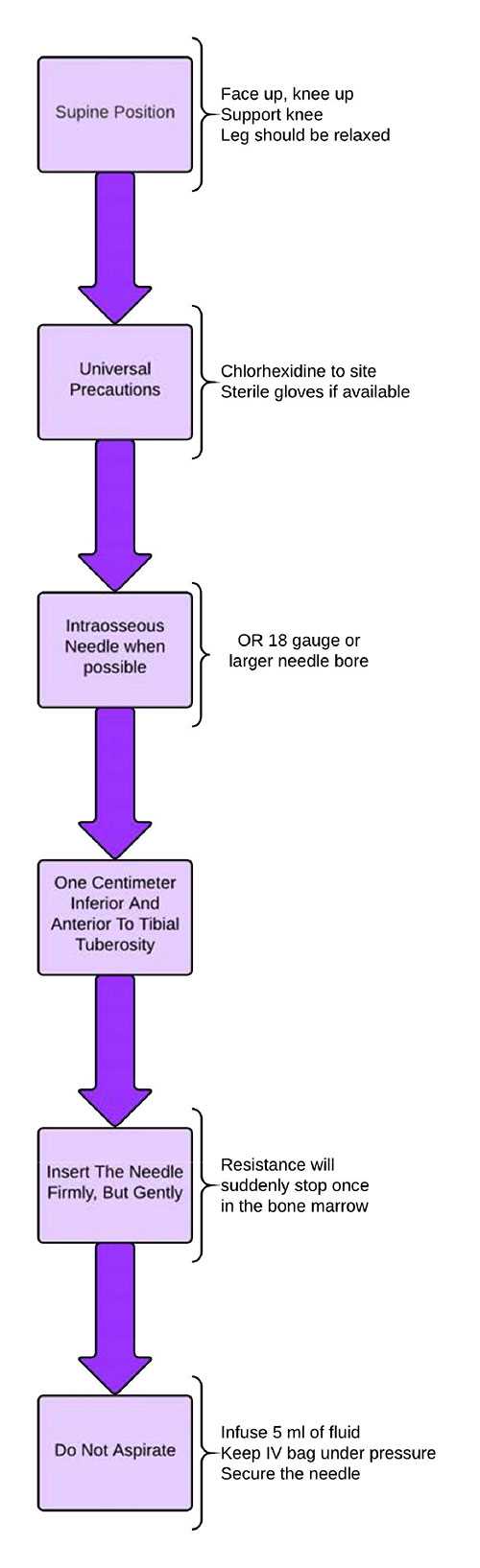
- IV Fluid Resuscitation: Fluid replacement, typically with isotonic solutions, helps restore blood volume and improve circulation. The rate and type of fluids depend on the child’s condition and the cause of shock.
- Medications: In some cases, medications may be required to support blood pressure or correct underlying issues, such as infection or blood loss.
- Continuous Monitoring: Close monitoring of vital signs, including heart rate, blood pressure, and oxygen levels, is essential to assess the effectiveness of treatment and guide further interventions.
Prompt and accurate intervention can make a significant difference in a child’s recovery from shock. Healthcare providers must be trained to recognize early signs, act quickly, and provide the necessary interventions to improve circulation, oxygen delivery, and overall stability.
Managing Respiratory Distress in Pediatric Emergencies
Respiratory distress in children is a serious condition that can lead to respiratory failure if not promptly addressed. It occurs when the child struggles to maintain adequate oxygen levels and effective ventilation. Timely recognition and appropriate management are crucial to prevent further complications and ensure the child’s stability. Respiratory distress may stem from various causes, including infections, asthma, trauma, or airway obstruction. Understanding the key steps to manage this condition can significantly improve patient outcomes.
Signs of Respiratory Distress in Children
- Increased Respiratory Rate: A child in respiratory distress often breathes faster than usual in an attempt to compensate for low oxygen levels.
- Use of Accessory Muscles: Visible chest retractions, such as the use of neck muscles, can indicate that the child is struggling to breathe.
- Abnormal Breath Sounds: Wheezing, stridor, or crackles may be heard, depending on the cause of the distress, signaling airway narrowing or fluid in the lungs.
- Color Changes: Cyanosis, or a bluish tint to the skin, lips, or extremities, is a late sign of inadequate oxygenation and requires immediate intervention.
- Altered Mental Status: Difficulty in concentrating, irritability, or lethargy can result from insufficient oxygen supply to the brain.
Management Strategies for Respiratory Distress
Management of respiratory distress requires a focused approach, aiming to address the underlying cause, improve oxygenation, and ensure the child’s airway remains open. The following steps are commonly employed in the clinical setting:
- Positioning: Position the child in a way that optimizes breathing. Elevating the head or propping the child up may help open the airways and ease breathing.
- Oxygen Therapy: Administering oxygen via nasal cannula or mask is often the first step to improve oxygen saturation and relieve distress.
- Airway Management: If the airway is compromised, clearing the airway and ensuring patency with suctioning, or advanced interventions such as intubation, may be necessary.
- Role Clarity: Every team member must understand their specific responsibilities. This clarity helps to prevent confusion and ensures that each task is performed efficiently and effectively.
- Leadership: Strong leadership is critical in guiding the team through complex procedures. The leader should make decisions, delegate tasks, and provide direction while maintaining a calm presence.
- Collaboration: Team members must collaborate effectively, sharing information, resources, and observations in real time. Each person’s input is vital to the success of the intervention.
- Mutual Respect: Respect for each team member’s expertise and experience fosters a positive working environment. This respect leads to better decision-making and more efficient problem-solving.
- Clear and Concise Information: In a high-pressure environment, it is important to deliver information in a simple and direct manner. Avoiding jargon and speaking clearly ensures that everyone understands critical updates.
- Closed-Loop Communication: To avoid misunderstandings, it’s essential that messages are confirmed and repeated by the recipient. This helps ensure that tasks are carried out as intended.
- Regular Updates: The team should provide ongoing updates on the patient’s condition and progress during the intervention. This keeps everyone informed and allows for timely adjustments to the treatment plan.
- Managing Conflict: Disagreements or tension may arise during high-stakes situations. Having protocols in place for resolving conflicts ensures that the team remains focused on the patient’s well-being rather than on individual differences.
- Monitor Vital Signs: Regular checks of heart rate, respiratory rate, blood pressure, and oxygen saturation levels are essential to track the patient’s recovery and detect any potential issues early.
- Neurological Evaluation: Assessing the patient’s neurological status, including responsiveness and pupillary reaction, helps determine brain function and possible damage following the emergency.
- Airway Management: Ensure that the airway remains clear and maintain adequate ventilation. If respiratory support is needed, continue with the appropriate interventions, such as oxygen therapy or mechanical ventilation.
- Fluid and Electrolyte Balance: Check for signs of dehydration, acidosis, or electrolyte disturbances, which can occur after the initial treatment phase. Adjust fluid and electrolyte management accordingly.
- Continue Monitoring: Keep close watch on the patient’s condition with continuous monitoring to detect any signs of deterioration or complications.
- Optimize Oxygenation: Administer supplemental oxygen to maintain appropriate levels of oxygen in the blood. This can support tissue perfusion and prevent hypoxia.
- Medications: Provide appropriate medications based on the patient’s needs, including vasopressors, antiarrhythmic drugs, or sedatives if required for ongoing stability.
- Reevaluate Treatment Plans: As the patient stabilizes, periodically reassess the need for further interventions and adjust treatment protocols accordingly. This may include transitioning to less intensive care once the patient is stable.
- Master the Basics: Familiarize yourself with the foundational principles of pediatric care, such as recognizing early signs of distress, understanding the anatomy and physiology of children, and knowing the appropriate interventions for various emergencies.
- Learn Emergency Protocols: Study the specific steps to take in critical scenarios, including resuscitation guidelines, airway management, and fluid resuscitation methods. Know when and how to administer medication, as well as how to monitor vital signs under emergency conditions.
- Simulate Real-Life Situations: Engage in practice drills that replicate actual emergency scenarios. This will help you build confidence in making quick decisions and improve your ability to stay calm under pressure.
- Work in Teams: Learn to collaborate effectively with other healthcare professionals. Team dynamics are essential in emergency settings, and understanding how to communicate and delegate tasks efficiently is crucial for success.
- Know the Time Limits: Be aware of the time constraints for each part of the assessment. Practice managing your time wisely so that you can complete each section without rushing or overlooking critical details.
- Stay Focused: Prioritize tasks based on urgency. In high-pressure situations, it’s easy to become overwhelmed, so staying focused on the most pressing issues is key to managing emergencies effectively.
- Stay Updated on Protocols: Ensure that you are familiar with the most current guidelines for pediatric care. Emergency protocols evolve over time, so it is essential to study the latest recommendations and best practices.
- Use Study Materials: Make use of study guides, online resources, and practice exams to reinforce your knowledge and test your understanding of important concepts.
Team Dynamics and Communication in Pediatric Emergency Care
Effective teamwork and clear communication are vital components in managing critical pediatric emergencies. In these high-stress situations, a coordinated effort from all healthcare providers is essential to ensure timely interventions and optimal outcomes. Every team member must understand their role and work together seamlessly, often under challenging conditions. The ability to communicate clearly and decisively can make a significant difference in the care provided to the patient.
Key Elements of Effective Teamwork
Communication Strategies in Critical Situations
By fostering effective teamwork and communication, healthcare providers can better manage pediatric emergencies. A unified approach, built on trust and clarity, can lead to faster decision-making, improved patient care, and ultimately better outcomes in critical situations.
Reassessment and Post-Resuscitation Care
Following the initial stabilization of a pediatric patient, continuous evaluation is crucial to assess the effectiveness of interventions and ensure that any underlying issues are addressed. After a resuscitation attempt, the patient’s condition may evolve rapidly, requiring frequent reassessment. Proper post-resuscitation management plays a vital role in preventing further complications and improving long-term outcomes.
Key Steps in Reassessment
Post-Resuscitation Care Guidelines
Timely reassessment and thorough post-resuscitation care are key to improving survival rates and minimizing long-term damage in critically ill pediatric patients. By continually evaluating and adjusting treatment plans, healthcare providers can help ensure the best possible outcomes in these high-risk scenarios.
Strategies for Passing the PALS Test
Preparing for advanced pediatric care assessments requires a combination of knowledge, practice, and focus. Successful completion of these evaluations not only requires understanding theoretical concepts but also the ability to apply them effectively in clinical scenarios. The following strategies will help you approach this challenge with confidence and increase your chances of success.
1. Understand Core Concepts
2. Practice with Scenarios
3. Focus on Time Management
4. Review Key Guidelines
By focusing on the critical aspects of pediatric care and practicing your response skills, you can improve your chances of passing this evaluation. Stay calm, stay prepared, and approach each scenario methodically for the best outcome.
Frequently Made Mistakes in PALS Exams
During pediatric emergency care evaluations, many individuals make certain errors that can negatively impact their performance. Understanding these common mistakes can help prevent them and improve overall preparedness. By recognizing where mistakes are typically made, you can better focus your efforts and approach each task with more precision and confidence.
1. Incorrect Prioritization of Interventions
One of the most common errors is failing to prioritize interventions based on the severity of the child’s condition. In emergency situations, quick thinking and prioritizing the most critical actions can make a significant difference. Misjudging the urgency of certain procedures may lead to delays in treatment.
2. Inadequate Airway Management
Proper airway management is crucial in pediatric emergencies. A frequent mistake is either underestimating the importance of securing the airway or performing airway interventions incorrectly. This can result in inadequate oxygenation and increased risk to the child’s well-being.
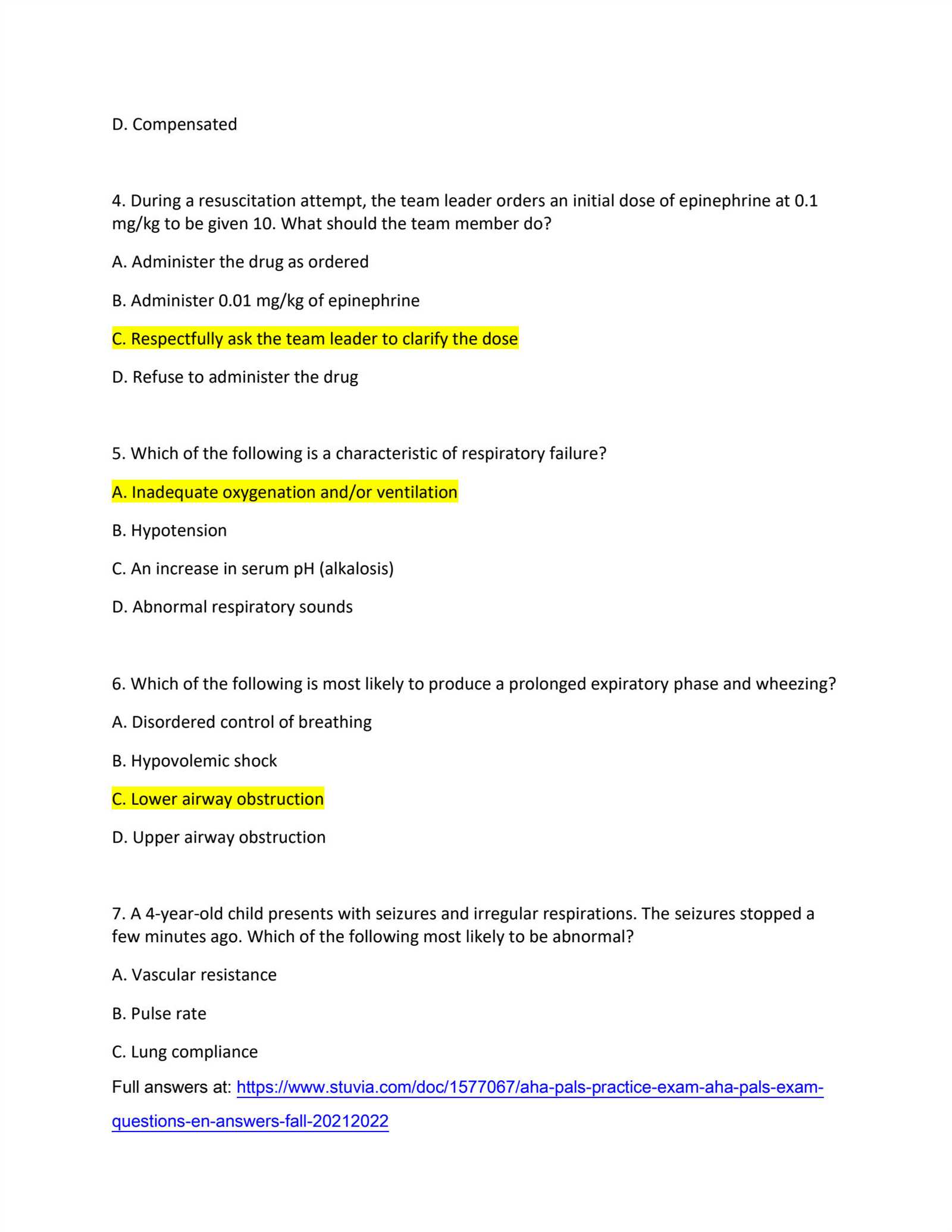
3. Mismanagement of Medications
Incorrect dosages or timing when administering medications can have serious consequences. Some candidates may mistakenly administer incorrect amounts or fail to recognize the contraindications of specific drugs, leading to ineffective or harmful outcomes.
| Common Mistakes | Impact on Outcome | Correction Strategy |
|---|---|---|
| Prioritizing less critical issues | Delays in life-saving interventions | Understand the hierarchy of care and assess the most critical aspects first |
| Improper airway management | Insufficient oxygenation | Practice airway techniques regularly to ensure proficiency |
| Incorrect medication administration | Potential for overdose or ineffective treatment | Double-check dosages and drug protocols before administration |
4. Failure to Follow Protocols
Emergency care protocols provide a structured framework for responding to critical situations. Not following these guidelines can lead to confusion, mistakes, and suboptimal care. It is essential to familiarize oneself with the established steps for every emergency scenario.
5. Lack of Effective Communication
In emergency settings, communication is vital. A common mistake is failing to communicate clearly with the team, which can lead to misunderstandings and delays. Ensuring that all team members are on the same page and delegating tasks efficiently is key to successful outcomes.
By being aware of these frequent mistakes and preparing for them, you can improve your ability to perform effectively in pediatric emergency situations. Staying calm, organized, and focused on the most critical aspects of care will help you achieve the best possible results.