When it comes to life-saving procedures during critical cardiac events, having a solid understanding of emergency protocols is essential. Mastering these concepts can make the difference in real-life situations where quick thinking and the right actions are crucial. This section is designed to provide you with key insights and strategies for excelling in a professional certification that focuses on advanced cardiovascular emergencies.
In this guide, we will explore the most important components of the certification process, offering a comprehensive approach to help you succeed. By reviewing common scenarios, understanding core techniques, and testing your knowledge, you will build the confidence needed to respond effectively in high-pressure situations. Whether you’re new to this field or refreshing your skills, our aim is to enhance your preparedness for emergency care.
Heartcode ACLS Test Answers Guide
Successfully navigating the certification process for advanced emergency care requires both a solid understanding of critical procedures and the ability to apply them in real-world situations. This section offers a structured approach to help you prepare for the evaluation that assesses your readiness to handle life-threatening scenarios. We will cover the essential components, key concepts, and strategies to ensure you’re fully equipped for the challenges ahead.
To excel in the certification process, it’s important to focus on the most commonly tested topics. These include recognizing signs of cardiac arrest, knowing the correct sequence of interventions, and understanding the role of medications in stabilizing patients. Additionally, practice with simulated cases allows you to reinforce your knowledge and gain confidence in your skills.
Through this guide, you’ll gain insights into the core principles that will be evaluated, as well as tips on how to approach questions with precision. Whether you’re just starting or preparing for a recertification, staying focused on key elements and consistently testing your understanding will set you on the path to success.
Understanding Advanced Life Support Certification
Obtaining certification in advanced emergency care is a critical step for healthcare professionals involved in managing life-threatening cardiovascular events. This qualification demonstrates proficiency in performing essential life-saving interventions, allowing practitioners to respond effectively in high-pressure situations. Understanding the certification process and its requirements will help you prepare for successful completion.
Core Skills and Knowledge
To earn this certification, candidates must demonstrate knowledge of various protocols related to cardiac emergencies. The certification process typically focuses on the following key areas:
- Recognizing and diagnosing life-threatening conditions
- Applying appropriate interventions and therapies
- Managing airways and monitoring vital signs
- Working effectively within a team during emergencies
Certification Process Overview
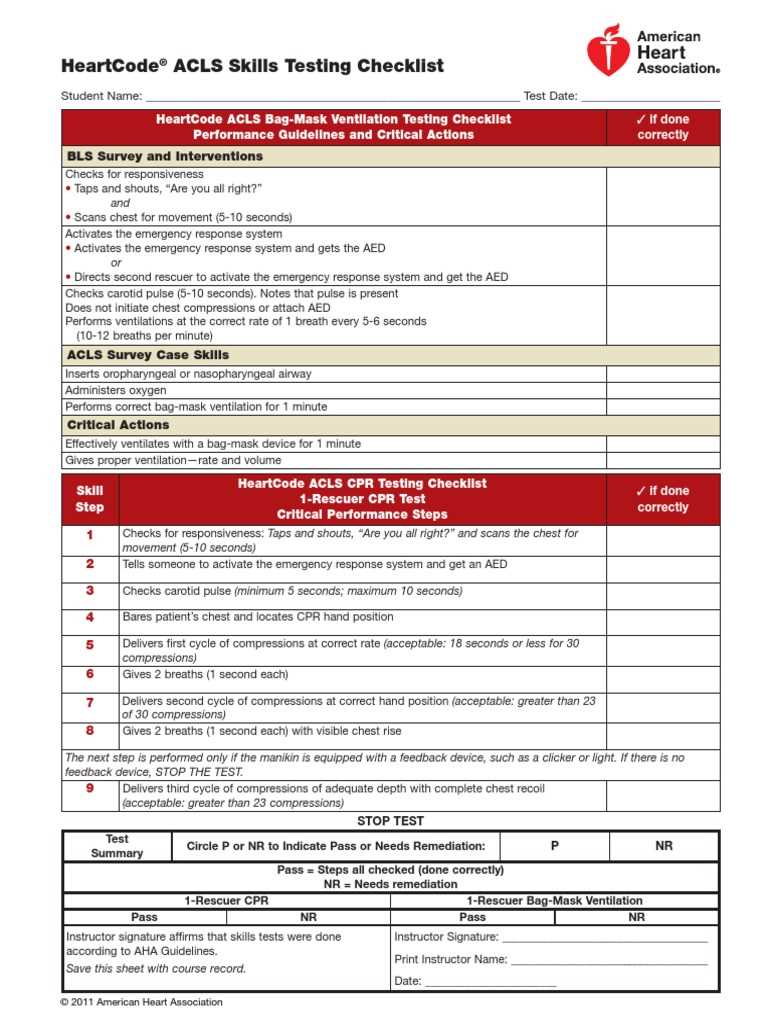
The certification procedure includes both theoretical and practical assessments. Here are the main steps involved:
- Complete the online learning modules that cover essential emergency protocols
- Participate in a hands-on skills session to practice key interventions
- Pass a final assessment that tests your ability to apply knowledge in a simulated environment
Successfully completing these stages equips healthcare professionals with the necessary skills to handle critical situations confidently and competently.
How to Prepare for the Certification Exam
Effective preparation for advanced emergency care certification requires a focused approach that emphasizes both knowledge and practical skills. Success in this field depends on a thorough understanding of emergency protocols and the ability to apply them under pressure. Proper preparation ensures that you can confidently respond to life-threatening situations and perform essential interventions when necessary.
To begin, familiarize yourself with the core concepts that are commonly evaluated in the certification process. This includes learning the steps for managing cardiac emergencies, understanding the correct timing for interventions, and reviewing common medications and their uses. It’s also helpful to practice with case studies that simulate real-life scenarios, allowing you to reinforce your skills in a controlled setting.
Additionally, engage in hands-on training sessions where you can apply what you’ve learned in practical exercises. Regularly testing your knowledge through quizzes or mock evaluations can also boost your confidence and ensure you’re ready for the final assessment.
Key Concepts for Advanced Emergency Care Exam
In order to succeed in the certification for advanced emergency care, it’s crucial to focus on the core principles that govern critical care procedures. Understanding the theoretical knowledge behind life-saving interventions and how to apply them effectively in real-life situations will prepare you for the challenges ahead. Mastery of these key concepts is essential for anyone aiming to demonstrate competence in managing cardiovascular emergencies.
Life-Threatening Conditions and Their Recognition
One of the most important aspects of the certification process is the ability to recognize the signs and symptoms of severe cardiovascular conditions. Being able to identify these conditions promptly is critical to initiating the correct interventions. Key conditions to focus on include:
- Cardiac arrest
- Arrhythmias
- Acute myocardial infarction (heart attack)
- Stroke and other cerebrovascular emergencies
Critical Interventions and Techniques
Equally important is understanding the correct sequence of interventions and therapies to apply once a life-threatening situation is recognized. These interventions include:
- Effective chest compressions and defibrillation
- Airway management and ventilation
- Administering appropriate medications and dosages
Mastery of these skills ensures that you can provide the necessary care in any emergency situation, increasing the chances of a positive outcome.
Commonly Asked Questions in Advanced Care Evaluations
When preparing for certification in advanced emergency care, it’s important to be familiar with the types of questions that are commonly asked. These questions typically focus on critical concepts and scenarios that assess your ability to handle high-stress situations effectively. Understanding these common queries will help you feel more confident and ready for the assessment process.
Below are some frequently asked questions you may encounter during the evaluation:
- What is the first step to take when responding to a cardiac arrest emergency?
- Which medications are recommended for stabilizing a patient after a heart attack?
- How do you assess the effectiveness of chest compressions during CPR?
- What is the correct sequence for managing a stroke victim?
- How do you distinguish between different types of arrhythmias?
These types of questions will require you to apply your knowledge of emergency care protocols and demonstrate your ability to make quick, informed decisions in critical situations. Practice answering these questions will help ensure you’re prepared for any challenge during the evaluation.
Effective Study Strategies for Advanced Care Certification
To succeed in obtaining certification in advanced emergency care, a structured and strategic approach to studying is essential. The complexity of the subject matter demands focused preparation that combines both theoretical knowledge and hands-on skills. Implementing effective study strategies will enhance your understanding and ensure that you’re fully prepared for the assessment.
Organize Your Study Plan
One of the most effective ways to prepare is to create a study schedule that breaks down the material into manageable sections. This allows you to focus on one topic at a time, reinforcing your understanding before moving on to the next. Key steps in creating an effective study plan include:
- Setting aside dedicated study time each day
- Prioritizing difficult or unfamiliar topics
- Reviewing key concepts regularly to reinforce learning
Use Practice Materials
Another valuable strategy is to utilize practice questions and mock scenarios. These materials help you apply what you’ve learned to real-world situations, improving your ability to think critically under pressure. Some helpful resources include:
- Online quizzes that simulate real assessments
- Interactive case studies that test your decision-making skills
- Review sessions with peers or instructors to discuss complex scenarios
Combining these study strategies with consistent practice will not only help you pass the evaluation but will also equip you with the necessary skills to respond effectively in emergency situations.
Advanced Care Evaluation Format Explained
Understanding the structure of the advanced emergency care certification assessment is crucial for successful preparation. The evaluation format is designed to test both theoretical knowledge and practical application in real-life emergency scenarios. Being familiar with the format helps reduce anxiety and allows you to focus on applying your skills effectively during the evaluation.
The assessment typically consists of several sections that evaluate different aspects of your knowledge and decision-making abilities. These sections include:
- Theoretical Knowledge: Questions on protocols, pharmacology, and procedures relevant to life-saving interventions.
- Scenario-Based Questions: Hypothetical scenarios where you must demonstrate how to manage emergency situations based on your training.
- Practical Skills Evaluation: A hands-on segment where you are required to perform life-saving techniques such as CPR, defibrillation, and airway management.
Familiarizing yourself with the structure and type of questions in each section allows you to concentrate your efforts on areas that need improvement, ultimately increasing your confidence and performance during the assessment.
Practice Questions for Advanced Care Preparation
One of the best ways to prepare for advanced emergency care certification is by practicing with questions that mirror the format and content of the evaluation. Practice questions allow you to test your knowledge, improve recall, and better understand the application of life-saving protocols in real-world situations. By working through these questions, you can identify areas where you need further study and refine your decision-making skills under pressure.
Types of Practice Questions
Practice questions typically come in a variety of formats to ensure that you are ready for all sections of the evaluation. Some common types include:
- Multiple-Choice Questions: These questions assess your understanding of emergency protocols, pharmacology, and clinical guidelines. They often test your ability to choose the correct action in a given scenario.
- Scenario-Based Questions: These simulate real-life emergency situations where you must apply your knowledge to determine the best course of action. Scenarios often include patient history, vital signs, and available interventions.
Why Practice is Crucial
Regularly working through practice questions helps you become more comfortable with the format of the assessment and allows you to gauge your level of preparedness. The more you practice, the more confident you will feel during the actual evaluation, improving both your performance and your ability to stay calm during high-pressure situations.
Advanced Care Certification Review Resources
When preparing for the advanced care certification, using comprehensive review resources is essential to ensure that all aspects of the program are covered. These resources can help you understand critical concepts, reinforce knowledge, and identify areas for improvement. Whether you prefer interactive study guides, video tutorials, or practice exams, there are a variety of materials available to support your learning process.
Types of Review Resources
Different types of review resources cater to various learning preferences. Some common options include:
- Study Guides: Detailed written materials that explain key concepts and procedures, often accompanied by diagrams and summaries for quick revision.
- Video Tutorials: Visual learning tools that demonstrate life-saving techniques and protocols, helping you understand the practical application of theoretical knowledge.
- Practice Exams: Simulated exams that mimic the structure and content of the actual certification evaluation, allowing you to test your knowledge and improve your time management.
Recommended Review Tools
Below is a table listing some of the most popular and effective resources for review:
| Resource | Type | Description |
|---|---|---|
| Official Study Guide | Written | A comprehensive manual covering all key concepts and protocols for emergency care. |
| Interactive Practice Exams | Online | Timed exams that simulate the actual certification process, helping you assess your readiness. |
| Video Demonstrations | Visual | Step-by-step video tutorials that showcase emergency care procedures in action. |
Using a combination of these review resources will enhance your preparation, ensuring that you are well-equipped to succeed in the certification process.
Understanding Cardiac Arrest Algorithms
Cardiac arrest algorithms are essential frameworks used in emergency medical scenarios to guide healthcare professionals through the steps needed to treat patients experiencing sudden cardiac arrest. These algorithms provide a systematic approach, ensuring that the most effective and timely interventions are administered to restore normal heart function. Understanding these protocols is crucial for making critical decisions during high-pressure situations.
The algorithms typically follow a series of decision points based on the patient’s condition, such as the rhythm of the heart, responsiveness, and overall stability. Each step in the process is designed to improve the chances of survival and minimize the risk of complications.
Key Steps in Cardiac Arrest Protocols:
- Initial Assessment: Quick evaluation of the patient’s condition to determine if cardiac arrest is present and whether immediate intervention is required.
- CPR (Cardiopulmonary Resuscitation): Administering chest compressions and rescue breaths to maintain circulation and oxygenation until advanced interventions are available.
- Defibrillation: Using electrical shocks to reset the heart’s rhythm in cases of shockable rhythms like ventricular fibrillation or pulseless ventricular tachycardia.
- Medications: Administering drugs such as epinephrine to stimulate the heart and improve the chances of successful resuscitation.
By mastering these algorithms and practicing them regularly, healthcare providers can ensure they are prepared to act swiftly and effectively during a cardiac arrest emergency.
How to Handle Cardiac Emergencies
Handling cardiac emergencies requires prompt action and a clear understanding of the necessary steps to provide immediate care. Whether a person is experiencing a heart attack, arrhythmia, or sudden cardiac arrest, the ability to act quickly can make the difference between life and death. It is essential to stay calm, assess the situation, and apply the appropriate interventions without delay.
In most cases, the first responder should focus on performing basic life support measures, including cardiopulmonary resuscitation (CPR) and defibrillation if necessary. The goal is to maintain circulation and oxygenation until advanced medical help arrives.
Essential Steps for Handling Cardiac Emergencies:
| Step | Description |
|---|---|
| Assessment | Quickly evaluate the victim for signs of cardiac arrest, including unresponsiveness and absence of a pulse. Confirm the need for immediate action. |
| CPR | Start chest compressions to keep the blood flowing and perform rescue breaths if trained. Continue until professional help takes over or the victim shows signs of recovery. |
| Defibrillation | If available, use an automated external defibrillator (AED) to deliver shocks to the heart to restore normal rhythm in cases of shockable rhythms. |
| Advanced Care | Once emergency medical services arrive, they will take over and provide advanced life support, including medications and airway management. |
By understanding and applying these basic principles, you can significantly improve the outcomes of cardiac emergencies and help save lives when every second counts.
Tips for Passing the Certification Exam
Successfully completing a certification exam in emergency cardiac care requires both knowledge and practice. The process can be challenging, but with the right strategies, you can confidently approach the exam. The key is to understand the material thoroughly, practice your skills, and manage your time effectively during the exam.
By focusing on the most critical concepts, reinforcing your knowledge through practical exercises, and reviewing important procedures, you can increase your chances of success. Here are some helpful tips to guide your preparation and boost your performance on the certification exam.
| Tip | Description |
|---|---|
| Review Core Concepts | Focus on understanding the primary principles of emergency cardiac care, including CPR, defibrillation, and recognition of life-threatening arrhythmias. Ensure you are comfortable with the algorithms and decision-making processes. |
| Practice Skills | Hands-on practice is essential. Make sure to regularly practice key techniques such as chest compressions, rescue breathing, and using an AED. Familiarize yourself with these procedures until they become second nature. |
| Take Practice Exams | Utilize practice exams and quizzes to test your knowledge. These will help you become familiar with the exam format, identify weak areas, and refine your approach. |
| Manage Time Effectively | During the exam, be mindful of time constraints. Answer the questions you know first, and make sure to pace yourself so you have time to review your responses before finishing. |
| Stay Calm and Focused | Staying calm is key during the exam. Take deep breaths, read each question carefully, and think through your answers. Confidence will help you make better decisions. |
By applying these strategies and dedicating time to preparation, you can improve your chances of passing the certification exam with flying colors.
Signs and Symptoms of Cardiac Arrest
Recognizing the early indicators of cardiac arrest is crucial for timely intervention. Understanding the common signs can make a significant difference in saving a life. When a person experiences this life-threatening event, immediate action is necessary to increase the chances of survival. Familiarity with the symptoms enables quick recognition and the initiation of the appropriate emergency response.
Key Symptoms to Watch For
The following symptoms are commonly associated with cardiac arrest and should not be ignored:
- Sudden Loss of Consciousness: The individual may collapse unexpectedly and be unresponsive, showing no signs of awareness.
- Absence of Pulse: A person in cardiac arrest will not have a detectable pulse, which can be checked by palpating the carotid artery.
- No Breathing: Victims may stop breathing or exhibit irregular, gasping breaths (agonal breathing) that are not sufficient for survival.
- Chest Pain: Severe, unexplained chest discomfort or pressure can sometimes precede cardiac arrest, but it may not always be present.
- Sudden Weakness or Dizziness: Extreme fatigue, lightheadedness, or fainting can also occur in the moments leading up to a cardiac event.
Immediate Actions
When you recognize these symptoms, it is important to act quickly. The following steps should be taken:
- Check for a Pulse and Breathing: Confirm whether the person is breathing and has a pulse. If not, begin CPR immediately.
- Call Emergency Services: Dial emergency services for professional assistance. Provide them with the location and details of the situation.
- Use an AED: If available, use an automated external defibrillator (AED) to deliver a shock to the heart and restore a normal rhythm.
By identifying the signs of cardiac arrest early and responding quickly, you can significantly improve the chances of survival for the affected person.
Role of Medications in ACLS Procedures
Medications play a vital role in the management of critical cardiovascular emergencies. They are administered during life-threatening situations to stabilize the patient, restore normal heart rhythms, and improve the chances of survival. The right medications, when used promptly and effectively, can help support the heart’s function and prevent further complications during a medical emergency.
Various classes of drugs are utilized in emergency cardiac care, each with specific functions. Some are aimed at restoring normal heart rhythms, while others help to manage blood pressure, reduce the risk of blood clots, or improve the heart’s ability to pump blood. Understanding the appropriate use of these medications is essential for healthcare providers involved in emergency interventions.
Commonly used medications in emergency cardiovascular procedures include:
- Antiarrythmics: These medications help to correct irregular heart rhythms, restoring normal cardiac function.
- Vasopressors: They are used to elevate blood pressure in situations of low blood pressure, improving blood flow to vital organs.
- Anticoagulants: These drugs are important in preventing the formation of blood clots, which can complicate heart attacks or strokes.
- Inotropes: These agents enhance the heart’s ability to contract and pump blood, improving cardiac output during critical episodes.
Administering these medications must be done under careful guidance to ensure they are effective and to avoid potential adverse reactions. Knowledge of the correct dosage, timing, and indications for each drug is critical in enhancing the outcomes of emergency procedures and improving patient survival rates.
Advanced Airway Management in Emergency Care
Effective airway management is a critical component in managing life-threatening situations, particularly in cases of respiratory failure or cardiac arrest. Ensuring an open and unobstructed airway allows for proper oxygenation and ventilation, which is essential for survival. In advanced medical protocols, a range of techniques and tools are utilized to secure the airway, prevent complications, and provide optimal care for the patient.
Advanced airway management techniques go beyond basic methods such as head-tilt-chin-lift and mouth-to-mouth resuscitation. These procedures often require specialized equipment and training to be executed successfully. The primary goal is to maintain an open airway, ensure adequate oxygen supply, and manage the airway in situations where standard methods are ineffective.
The key components of advanced airway management include:
- Endotracheal Intubation: This technique involves placing a tube directly into the trachea to secure the airway and facilitate the administration of oxygen and other necessary treatments. It is commonly used in severe respiratory distress or during resuscitation efforts.
- Supraglottic Airway Devices: These devices, such as the laryngeal mask airway (LMA), provide an alternative to endotracheal intubation, offering a less invasive way to ensure airway patency in emergency situations.
- Ventilatory Support: Once the airway is secured, providing adequate ventilatory support is crucial. This includes using mechanical ventilators or manual devices to assist or take over the patient’s breathing process, ensuring sufficient oxygenation.
Successful airway management is not only about securing the airway but also about making quick decisions, using the appropriate equipment, and understanding when to switch between different methods. Proper training and understanding of these advanced techniques can significantly improve patient outcomes during critical emergencies.
Importance of High-Quality Chest Compressions
Chest compressions play a vital role in the initial stages of managing cardiac emergencies. They are designed to maintain circulation and ensure that oxygen-rich blood continues to flow to vital organs, especially the brain and heart. High-quality compressions are essential for increasing the chances of survival in patients who are in cardiac arrest. Without proper blood circulation, tissues and organs begin to deteriorate quickly, leading to irreversible damage.
Effective chest compressions must be performed with proper depth, rate, and recoil to ensure blood is circulated effectively throughout the body. The recommended depth is around 2 inches (5 cm), with compressions occurring at a rate of 100 to 120 per minute. Allowing full chest recoil between compressions ensures that the heart has enough time to refill with blood before the next compression. Inadequate or poorly performed compressions can significantly decrease the chances of a successful outcome.
Key factors that contribute to high-quality chest compressions include:
- Depth: Compressions should be deep enough to generate adequate blood flow. Insufficient depth may not effectively circulate oxygenated blood to critical areas.
- Rate: The pace of compressions is just as important as the depth. Maintaining a consistent and appropriate rate is necessary to maximize circulation.
- Recoil: Ensuring that the chest fully returns to its normal position between compressions helps in promoting blood flow and maintaining adequate heart function.
Performing high-quality chest compressions consistently throughout resuscitation efforts is one of the most significant actions a responder can take to improve survival rates. They are often the cornerstone of any resuscitative effort and can be the deciding factor in whether a person survives or not. Training and practice are essential to ensure that these life-saving techniques are performed effectively under stress.
Post-Resuscitation Care and Follow-Up
Once the immediate threat of cardiac arrest is managed and the individual is stabilized, the next phase of care is essential to ensure recovery and prevent further complications. Post-resuscitation care focuses on monitoring, addressing any underlying causes, and optimizing organ function to increase the chances of survival and long-term health. This stage involves a combination of therapeutic strategies, medical assessments, and continuous monitoring to support the patient as they transition from an emergency state to a more stable condition.
Monitoring and Stabilization
After successful resuscitation, it is crucial to maintain close monitoring of the patient’s vital signs. This includes tracking blood pressure, heart rate, oxygen saturation, and respiratory status to detect any signs of deterioration. In addition, ensuring the patient remains adequately oxygenated and maintaining proper ventilation is key during this period. Medications may be administered to regulate heart rhythms or manage any underlying conditions that contributed to the cardiac event.
Further Medical Interventions and Assessment
During the post-resuscitation phase, medical teams will work to identify and treat the underlying cause of the cardiac arrest, such as an arrhythmia, heart attack, or electrolyte imbalance. Imaging tests, blood work, and other diagnostic tools may be used to provide a comprehensive assessment of the patient’s condition. Additionally, targeted temperature management (cooling) may be employed to protect brain function in some cases.
Follow-up care often includes a structured rehabilitation plan to address physical and psychological recovery. This may involve physical therapy, counseling, and monitoring for any potential complications. Long-term follow-up is essential to assess heart function, prevent future episodes, and ensure the overall health and well-being of the patient.