In today’s healthcare environment, safeguarding sensitive information is more critical than ever. Organizations are required to maintain the highest standards of confidentiality and security to protect patient data. Adherence to various laws and regulations ensures that health-related details remain protected from unauthorized access, securing both individual privacy and the trust in healthcare systems.
Comprehending these regulations can be challenging, especially for professionals who must pass assessments to confirm their understanding. These evaluations test knowledge of the principles governing the handling of personal health information and other confidential details. Mastering these concepts is essential for those working in medical, administrative, or security roles within the healthcare sector.
Passing such evaluations demands thorough preparation and a clear grasp of the core principles that govern patient confidentiality and data protection. Success not only ensures compliance with legal standards but also upholds the integrity of healthcare practices across the country.
Understanding Key Healthcare Data Protection Principles
In the healthcare sector, protecting sensitive personal information is a foundational principle. Laws have been enacted to ensure that patient records and related details are shielded from unauthorized access, misuse, or disclosure. These regulations are crucial in maintaining public trust and safeguarding individual rights in medical and administrative settings.
There are several key concepts that professionals need to understand to comply with these standards:
- Confidentiality: Ensuring that information shared between a healthcare provider and a patient remains private and protected from unauthorized access.
- Data Security: Implementing safeguards to prevent unauthorized access, alteration, or destruction of personal health information.
- Access Control: Limiting access to sensitive data only to authorized personnel based on their role and need to know.
- Patient Rights: Giving individuals control over their personal health information, including the right to access, correct, or restrict its use.
Professionals must be familiar with how these principles apply to daily operations in medical facilities, ensuring compliance with legal standards and minimizing the risk of data breaches. Mastery of these concepts is essential for anyone involved in handling or managing patient information.
Key Components of Healthcare Data Protection Regulations
Healthcare organizations are required to adhere to several critical regulations designed to protect patient information. These standards outline how personal health records should be managed, shared, and secured to prevent unauthorized access. Understanding the essential components of these regulations is vital for professionals in the healthcare field to ensure compliance and safeguard sensitive data.
The following are the primary elements of these regulations:
- Security Standards: Requirements for safeguarding electronic health records through encryption, secure communication channels, and access controls.
- Compliance Audits: Regular reviews and audits to ensure that organizations are meeting legal obligations for information security and privacy.
- Data Breach Protocols: Specific procedures to follow in case of a data breach, including notification requirements to affected individuals and government authorities.
- Minimum Necessary Rule: Limiting access to personal health information to only the minimum amount necessary for specific tasks or roles.
- Patient Consent: Ensuring that patients provide explicit consent for the use and disclosure of their health information, with certain exceptions for healthcare operations.
Each of these components plays a crucial role in maintaining the confidentiality and security of patient information. By understanding and applying these standards, healthcare professionals can help mitigate risks and maintain trust in healthcare systems.
Importance of Legal Compliance in Data Protection
Ensuring the confidentiality of personal information is not just an ethical responsibility but a legal one. Regulations governing the handling of sensitive data in healthcare aim to protect individuals’ rights and uphold public trust. Compliance with these laws is essential for organizations that manage patient information to prevent legal penalties and mitigate risks associated with data breaches.
Consequences of Non-Compliance
Failure to adhere to data protection regulations can result in severe consequences, including:
- Legal Penalties: Organizations may face hefty fines and sanctions for violating regulations governing the protection of personal data.
- Loss of Trust: Non-compliance can damage the reputation of healthcare providers, eroding patient trust and confidence in their ability to safeguard sensitive information.
- Security Breaches: A lack of adherence to regulatory standards can leave organizations vulnerable to cyberattacks, potentially exposing sensitive data to unauthorized parties.
Benefits of Compliance
Adhering to data protection laws offers several benefits that go beyond legal protection:
- Enhanced Security: By following established standards, organizations can improve their data security measures, ensuring patient information is adequately protected.
- Patient Confidence: Compliance helps build trust with patients, showing that healthcare providers are committed to safeguarding their personal health information.
- Operational Efficiency: Following compliance protocols streamlines data management processes, reducing the risk of errors and enhancing operational efficiency.
In summary, maintaining compliance with data protection regulations is vital for the well-being of both healthcare organizations and the individuals they serve. It not only prevents legal repercussions but also fosters a culture of trust and security within the healthcare system.
Common Mistakes in Data Protection Education
When it comes to safeguarding sensitive health information, thorough education is essential. However, many individuals make common errors during their learning process, which can lead to gaps in understanding the key principles of information security. These mistakes can have serious consequences, especially when it comes to maintaining compliance with legal standards and avoiding data breaches.
Overlooking Key Concepts

One of the most frequent errors is failing to fully grasp the foundational concepts behind data protection. Some of the common pitfalls include:
- Misunderstanding Access Controls: Many fail to recognize the importance of limiting access to sensitive data to only authorized personnel based on their roles.
- Neglecting Data Encryption: Not understanding how encryption and secure data transmission methods are vital for protecting information in transit and at rest.
- Underestimating Data Retention Policies: Confusion around how long certain data should be stored and when it should be securely deleted can lead to potential compliance violations.
Relying on Outdated Information
Another critical mistake is relying on outdated or incorrect material. Legal standards and technological advancements evolve, and staying up to date is crucial. Common mistakes in this area include:
- Using Old Training Resources: Outdated training materials may not reflect the latest regulations or best practices, leading to gaps in knowledge.
- Ignoring New Technology Risks: Failing to account for the challenges introduced by new technologies, such as cloud storage or mobile access, can create vulnerabilities in data security.
By being aware of these common mistakes, individuals can avoid critical errors that may compromise the protection of sensitive information and help ensure they are fully prepared to handle data responsibly.
How the Assessment Process Works
The assessment process is designed to evaluate an individual’s understanding of critical regulations governing the protection of sensitive health information. It tests knowledge in a structured format, ensuring that individuals are well-prepared to handle confidential data according to legal standards. The process involves a series of questions covering various aspects of security, access controls, and compliance with applicable laws.
Typically, participants are required to complete the assessment within a set timeframe, answering questions based on their knowledge of regulatory guidelines. The test format may include multiple-choice questions, scenario-based questions, or even short-answer items that require detailed responses. The goal is to assess both theoretical understanding and practical application of data protection principles.
Key Features of the Assessment:
- Timed Completion: Participants must complete the test within the designated period, usually offering a limited number of attempts to achieve a passing score.
- Scenario-Based Questions: The test may feature real-world scenarios to evaluate how well individuals can apply their knowledge in practical situations.
- Scoring System: The test results are typically scored automatically, providing instant feedback on correct and incorrect responses.
- Multiple Attempts: In some cases, individuals may be allowed multiple attempts to retake the assessment until they achieve the required score.
Successfully passing the assessment confirms that an individual has acquired the necessary knowledge to handle sensitive data securely and in accordance with legal standards. This certification is often a prerequisite for roles involving the management of confidential health information.
Preparing for Data Protection Certification Assessments
Successfully passing a certification test focused on data security regulations requires careful preparation and a solid understanding of the core principles involved in safeguarding sensitive health information. Professionals must be familiar with the legal frameworks, security protocols, and operational procedures that ensure compliance and protect patient data from unauthorized access.
Here are some key steps to effectively prepare for such assessments:
- Review Core Regulations: Start by thoroughly reading the regulations governing the protection of personal health information. Focus on the key provisions regarding data access, storage, transmission, and disclosure.
- Study Best Practices: Familiarize yourself with the industry’s best practices for data security. This includes understanding how to implement encryption, access controls, and secure communication practices.
- Understand Scenarios: The test may feature case-based questions that assess how well you can apply knowledge to real-world situations. Practice with hypothetical scenarios to improve your decision-making skills under various conditions.
- Take Practice Quizzes: Many resources offer mock tests or quizzes that simulate the actual assessment. These help familiarize you with the format and types of questions you’ll encounter, as well as identify areas where you need to improve.
- Stay Updated: Regulations and best practices evolve, so make sure your study materials are current. Keeping up with the latest updates ensures you’re not tested on outdated information.
By following these steps, individuals can boost their chances of passing the certification assessment, ensuring they are well-equipped to handle confidential information in compliance with legal standards. Proper preparation not only leads to success in the assessment but also enhances one’s ability to safeguard sensitive data in the workplace.
Essential Tips for Passing Certification Assessments
Successfully completing a certification assessment that tests knowledge of regulatory guidelines and data protection practices requires more than just familiarity with the content. It involves a strategic approach to preparation, focusing on understanding key concepts, applying best practices, and managing your time effectively during the test. Here are some essential tips to help you pass with confidence.
Start by familiarizing yourself with the most common topics covered in these assessments. Ensure that you have a deep understanding of core regulations, including access control, data security, and breach management. This foundation will be crucial for answering both theoretical and practical questions.
- Review the Official Study Materials: Use trusted resources provided by your organization or official platforms to study the relevant material. These materials are designed to align closely with the assessment content and will help you focus on what is most important.
- Practice with Sample Questions: Taking practice tests or quizzes that mimic the format of the real assessment will help you get comfortable with the structure and types of questions you’ll encounter. It also allows you to identify any areas where you need additional study.
- Focus on Key Regulations: Concentrate your efforts on understanding the specific legal requirements that govern data handling and security. Pay attention to common scenarios and examples of how these regulations are applied in practice.
- Stay Calm and Manage Time: During the assessment, take your time to read each question carefully. Avoid rushing, as this can lead to errors. Manage your time wisely, ensuring that you can complete all questions without feeling pressured.
- Seek Clarification When Needed: If you encounter unclear or complex questions, don’t hesitate to ask for clarification (if allowed). Sometimes, even a small misunderstanding can affect your overall performance.
By following these tips, you can approach the assessment with the confidence and knowledge needed to succeed. With preparation, focus, and effective study strategies, passing the certification will be a manageable and rewarding experience.
Role of Confidentiality in Healthcare
Confidentiality is a cornerstone of the healthcare system, ensuring that sensitive patient information is protected from unauthorized access. It is essential for fostering trust between healthcare providers and patients, encouraging individuals to share their health history openly, which is critical for providing accurate and effective care. Maintaining confidentiality is not only a legal obligation but also a professional responsibility that upholds the integrity of the healthcare profession.
Why Confidentiality Matters
Confidentiality serves multiple purposes in the healthcare environment:
- Trust Building: When patients know their information is secure, they are more likely to be honest with their healthcare providers, leading to better diagnosis and treatment outcomes.
- Legal Compliance: Healthcare organizations must comply with a variety of regulations that mandate the secure handling of patient data. Violating confidentiality can result in significant legal consequences.
- Prevention of Harm: Protecting sensitive data helps prevent potential harm, such as discrimination, identity theft, or financial loss, which can arise from unauthorized disclosure.
Maintaining Confidentiality in Practice
Healthcare professionals must take specific actions to ensure the confidentiality of patient information:
- Access Controls: Only authorized individuals should have access to sensitive data, based on their role and necessity in patient care.
- Secure Communication: Health information should be communicated through secure methods, whether in writing, over the phone, or digitally, to prevent unauthorized interception.
- Data Encryption: Encrypting digital data ensures that even if information is intercepted, it remains unreadable to unauthorized parties.
Ultimately, maintaining confidentiality is a critical practice that supports both patient rights and the effective functioning of the healthcare system. It is an ongoing responsibility for all professionals within the sector.
Top Resources for Data Protection Education
When preparing for certification or enhancing knowledge about data security regulations, it’s essential to use reliable and comprehensive resources. These materials provide a structured approach to understanding the complexities of safeguarding personal health information. The right tools can make the difference between simply passing a test and truly mastering the concepts that will guide your professional responsibilities in handling sensitive data.
Here are some of the best resources to help you prepare for data protection assessments:
- Government Websites: Official government platforms, such as the Department of Health and Human Services (HHS), offer free resources and guidelines on the proper management and protection of sensitive health data. These sites often include detailed regulations, FAQs, and compliance tools.
- Online Educational Platforms: Websites like Coursera, Udemy, and LinkedIn Learning offer comprehensive courses focused on legal standards for information protection, covering everything from data encryption to breach response protocols.
- Webinars and Workshops: Many organizations host live or recorded webinars that discuss current best practices and regulatory changes. These events are valuable for gaining deeper insights and asking questions in real-time.
- Books and Textbooks: Comprehensive guides, such as *The Complete Guide to Data Security* or similar textbooks, provide in-depth knowledge on regulations, compliance strategies, and security measures. These can be excellent for structured, self-paced learning.
- Certification Programs: Accredited certification programs, such as those offered by the American Health Information Management Association (AHIMA) or the Health Information and Management Systems Society (HIMSS), offer specialized courses and credentials for professionals working with health data.
By utilizing these resources, individuals can gain a well-rounded understanding of the regulations governing data protection and become proficient in securing sensitive information in compliance with legal standards. Whether you are preparing for an assessment or simply looking to expand your knowledge, these tools will provide the foundation needed for success.
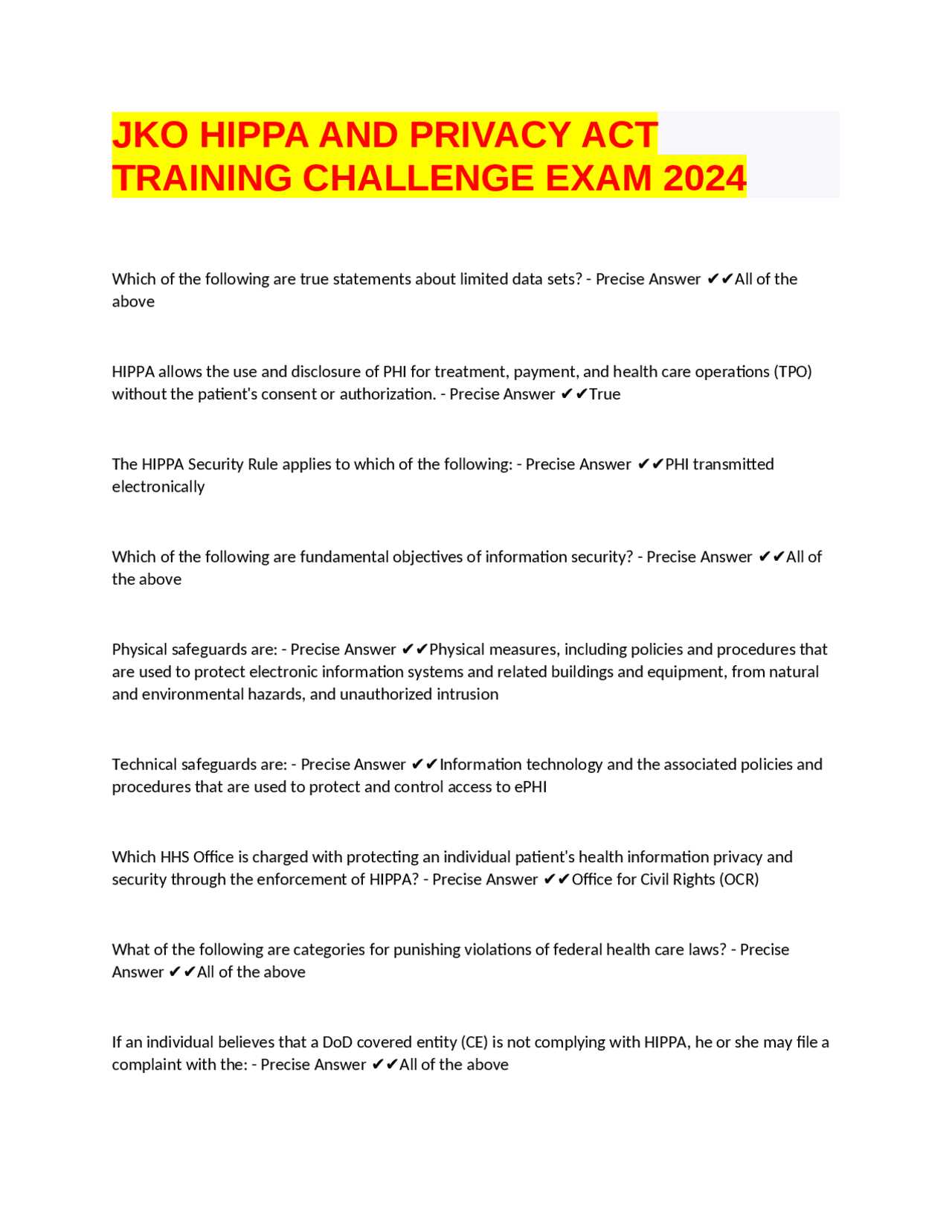
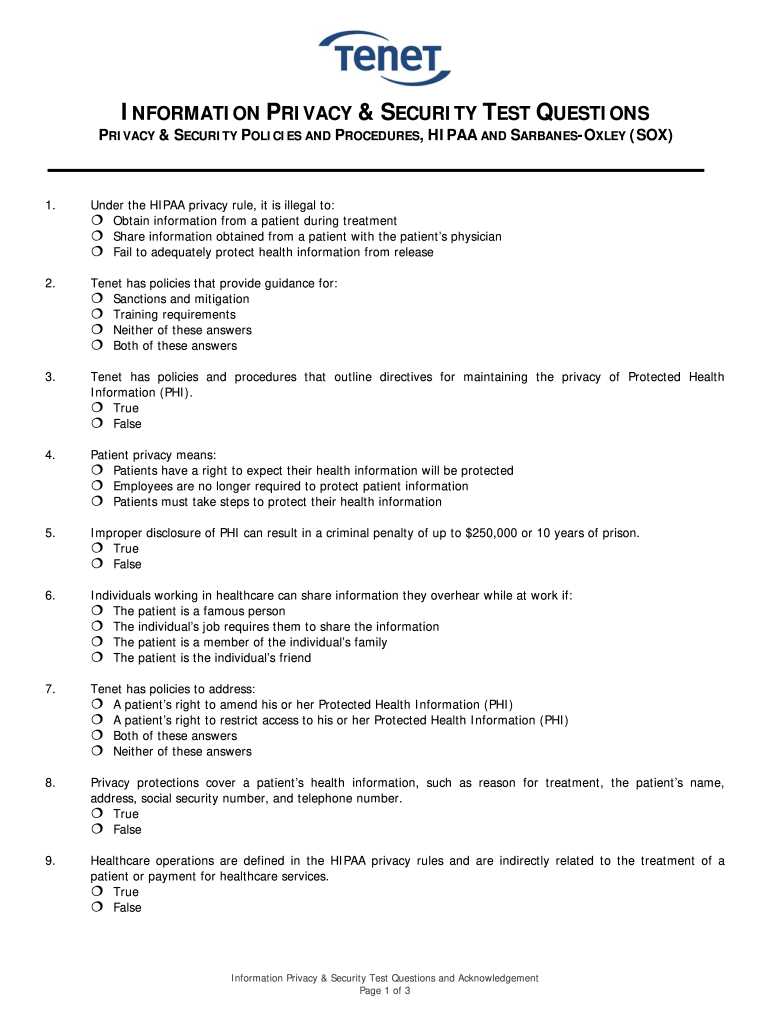
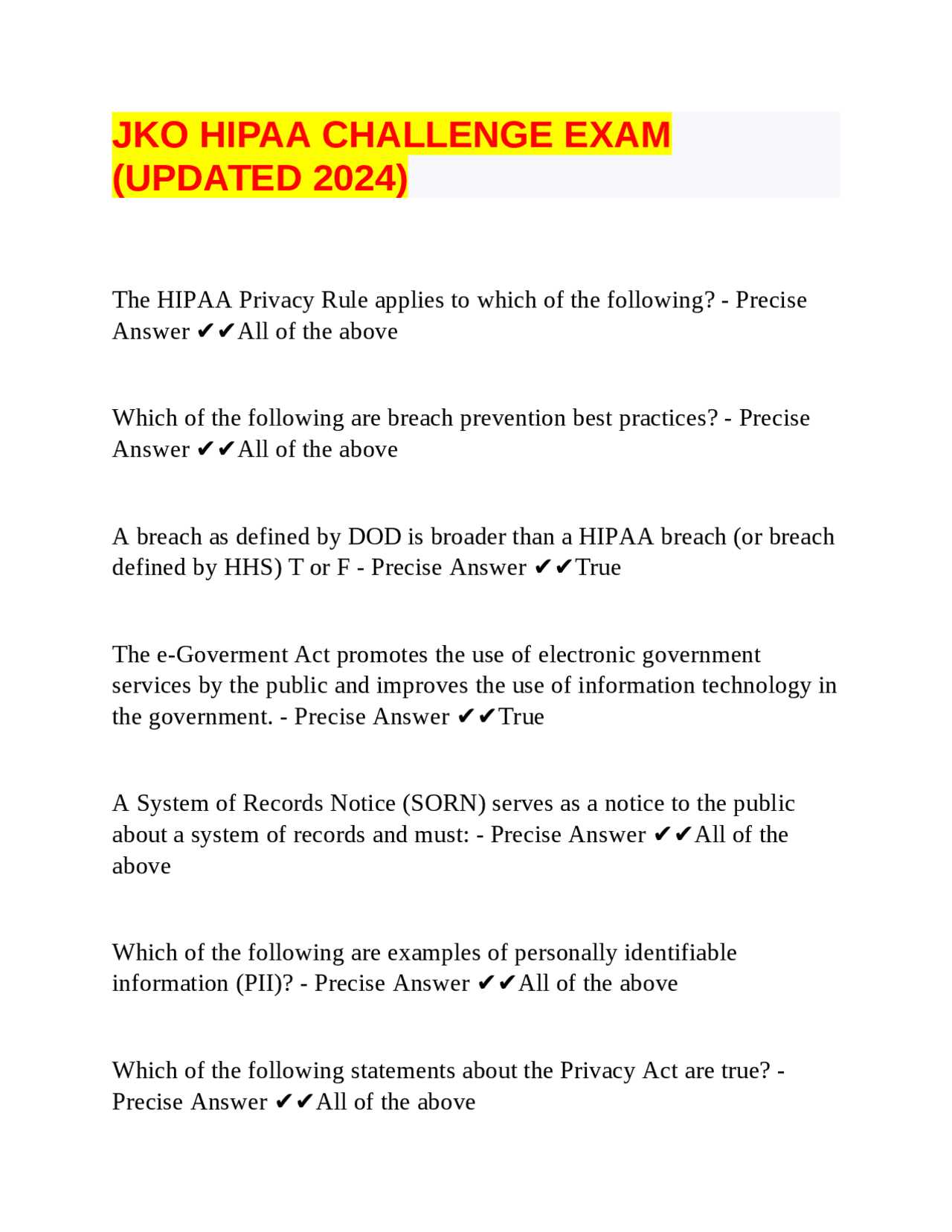
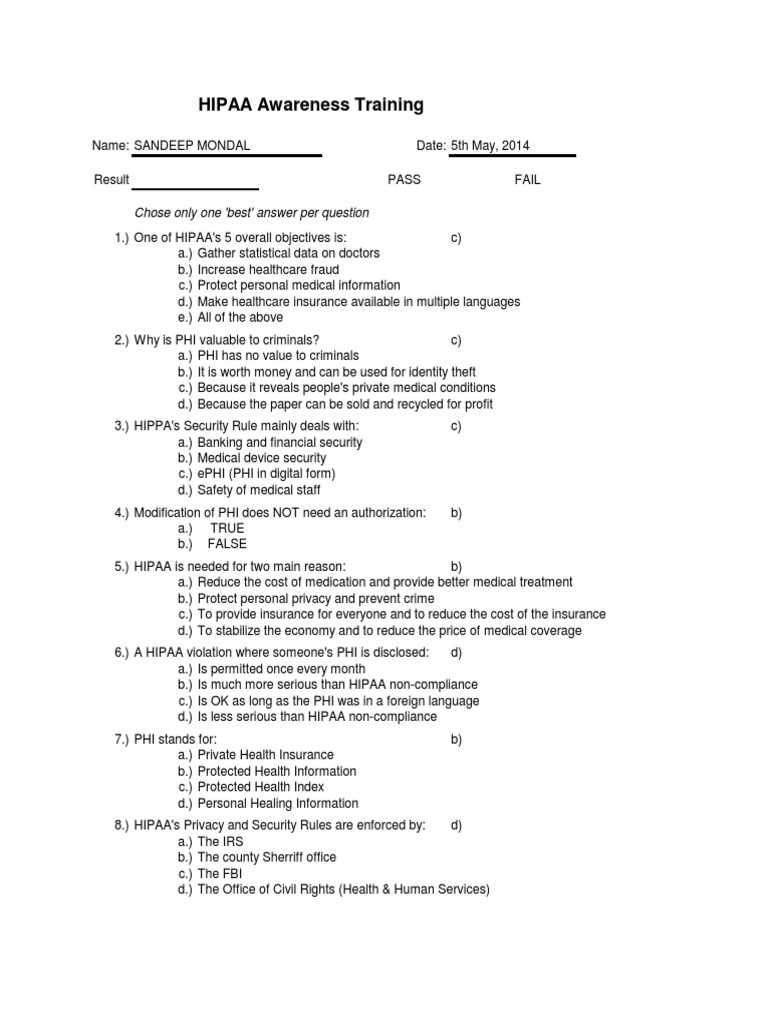
Common Questions in Certification Assessments
When preparing for certification assessments related to data protection regulations, it’s important to be familiar with the types of questions you may encounter. These assessments typically cover a wide range of topics designed to test your understanding of security measures, legal compliance, and best practices for handling sensitive health information. Knowing the kinds of questions commonly asked can help you focus your studies and boost your confidence.
Here are some of the most common types of questions found in these assessments:
- Regulatory Compliance Questions: These questions assess your knowledge of laws governing the handling of sensitive information. For example, you may be asked to identify which regulations apply in specific scenarios or to explain the consequences of non-compliance.
- Scenario-Based Questions: These questions present real-world situations in which you must apply your understanding of security protocols. You might be asked how to handle a data breach or how to ensure that only authorized individuals have access to confidential information.
- Data Security Best Practices: These questions focus on the practical steps involved in securing personal health data. Expect questions about encryption, access controls, secure communication methods, and how to ensure confidentiality in everyday healthcare operations.
- Roles and Responsibilities: Many questions address the specific responsibilities of healthcare workers in protecting patient information. You may be asked to identify which staff members are responsible for specific data security tasks or to outline the steps they must take to maintain compliance.
- Legal Implications of Data Breaches: Questions in this category test your understanding of the legal consequences that can arise from mishandling sensitive data. You may be asked about potential fines, sanctions, or reputational damage following a data breach.
By understanding these common question types, you can better prepare for your certification assessment, ensuring that you are equipped to handle various scenarios and demonstrate your knowledge of data security regulations effectively.
Understanding Protected Health Information
Protected health information (PHI) refers to any personal data related to an individual’s health status, care, or payment for medical services that is kept private and secure. This information can be used to identify a person and is often collected and stored by healthcare providers, insurance companies, and other entities involved in patient care. Safeguarding this data is essential to ensure confidentiality, trust, and legal compliance within the healthcare industry.
PHI encompasses a wide range of data, including but not limited to medical records, test results, insurance information, and any other personal health-related details. Understanding what constitutes PHI is critical for healthcare professionals, as mishandling this data can lead to legal consequences and breaches of trust with patients.
What Constitutes Protected Health Information?
Protected health information can include any of the following types of data:
| Type of Information | Examples |
|---|---|
| Personal Identifiers | Name, address, phone number, Social Security number |
| Medical Records | Doctor’s notes, lab results, diagnosis |
| Payment Information | Billing records, insurance claims, payment history |
| Healthcare Provider Information | Doctor’s name, hospital name, clinic visits |
How PHI is Protected

There are various methods and technologies used to ensure the security and confidentiality of protected health information. These include:
- Encryption: Data encryption ensures that any transmitted or stored health information is unreadable to unauthorized individuals.
- Access Control: Limiting access to sensitive information ensures that only authorized personnel can view or modify patient records.
- Data Masking: Masking or de-identifying data when necessary ensures that personal identifiers are not exposed in certain circumstances.
Understanding what constitutes protected health information, how it is used, and how to ensure its security is vital for anyone working in healthcare. By adhering to these standards, professionals can help maintain patient trust and comply with legal requirements for safeguarding sensitive data.
Privacy Act’s Impact on Health Records
The implementation of regulations governing the protection of personal health data has had a profound effect on how healthcare organizations manage, store, and share health records. These rules ensure that sensitive patient information is kept confidential and secure, outlining strict guidelines for how it can be accessed, shared, and used. The legislation not only protects individuals’ rights but also helps healthcare providers maintain public trust by safeguarding the integrity of patient information.
Understanding the impact of these regulations is crucial for healthcare professionals, as compliance is not optional but a legal requirement. These regulations dictate the methods for storing, transmitting, and using patient records, as well as the protocols for responding to potential breaches of data security.
Key Impacts on Health Records Management
The implementation of these laws has significantly changed how health information is managed. Below are some of the main effects:
| Impact Area | Description |
|---|---|
| Access Restrictions | Healthcare providers are required to limit access to personal health information to only those who need it for legitimate medical or administrative purposes. |
| Patient Consent | Before sharing health data with third parties (such as insurance companies or researchers), healthcare providers must obtain explicit patient consent, ensuring individuals have control over their own information. |
| Data Accuracy | Healthcare organizations are required to maintain accurate, up-to-date health records, which includes giving patients the right to review and request corrections to their records if necessary. |
| Audit Trails | An audit trail must be maintained to track all access and modifications made to health records, ensuring accountability and transparency in handling sensitive data. |
Legal Ramifications of Non-Compliance
Failing to adhere to these regulations can result in significant legal consequences, including fines and legal action against the healthcare provider. Non-compliance can also lead to loss of trust from patients, which can have long-term repercussions for an organization’s reputation and ability to operate effectively.
By understanding the privacy protections and their impact on health records, healthcare organizations can ensure that they comply with the law, protect patient data, and foster a culture of trust and responsibility in their operations.
How to Avoid Privacy Violations
Maintaining the confidentiality of sensitive information is a fundamental responsibility for healthcare professionals. To avoid privacy violations, it is essential to adopt a comprehensive approach that includes proper handling of data, adherence to security protocols, and awareness of the rules governing the sharing of personal information. Ensuring that patient data remains secure not only complies with the law but also fosters trust and respect between healthcare providers and their patients.
Here are some key practices that can help prevent privacy violations in healthcare settings:
| Best Practice | Description |
|---|---|
| Limit Access to Sensitive Information | Ensure that only authorized personnel have access to sensitive patient data, and restrict access to information on a need-to-know basis. |
| Use Strong Authentication Methods | Implement strong password policies, multi-factor authentication, and encryption to protect digital records from unauthorized access. |
| Implement Secure Communication Channels | Use encrypted methods for transmitting sensitive data electronically and avoid sharing personal health information over unsecured channels like email or text messages. |
| Educate Staff Regularly | Provide ongoing education to employees about their responsibilities in safeguarding sensitive information and the consequences of violations. |
| Conduct Regular Audits | Perform regular audits of data access logs to monitor for unauthorized access or unusual activity that may indicate a potential breach. |
| Ensure Secure Disposal of Data | Ensure that paper records containing sensitive information are shredded and that electronic records are properly deleted to prevent unauthorized recovery. |
By following these best practices, healthcare organizations can significantly reduce the risk of privacy violations. Adopting a proactive approach to data protection not only helps to comply with legal requirements but also safeguards the reputation and integrity of the healthcare system as a whole.
Consequences of Non-Compliance with Health Data Protection Laws
Failing to comply with regulations governing the handling of sensitive health information can have severe repercussions for healthcare organizations and their employees. Non-compliance not only jeopardizes patient trust but also exposes organizations to significant legal, financial, and reputational risks. These regulations are in place to ensure the confidentiality, integrity, and security of personal health data, and violating these standards can lead to serious consequences for all parties involved.
The penalties for not adhering to these laws can vary depending on the severity of the violation, the level of negligence, and the harm caused. It is essential for healthcare professionals and organizations to understand the potential risks and take proactive steps to maintain compliance at all times.
Legal and Financial Penalties
Organizations found guilty of non-compliance can face substantial legal and financial penalties. These include:
- Fines: Penalties can range from minor fines for small infractions to multi-million-dollar penalties for serious violations, such as large-scale data breaches or systemic issues with data protection.
- Criminal Prosecution: In cases of intentional misuse of data or gross negligence, individuals may face criminal charges, leading to further legal consequences and potential jail time.
- Compensation for Damages: Organizations may be required to compensate affected individuals for damages resulting from the mishandling of their health information, including emotional distress or financial losses caused by identity theft.
Reputational Damage
Non-compliance can also cause significant damage to the reputation of healthcare providers. When patient information is compromised or mishandled, it erodes trust and confidence in the organization. The long-term impact of this damage can include:
- Loss of Patients: Patients may choose to seek care elsewhere if they feel that their personal information is not being adequately protected.
- Public Scrutiny: A breach or violation of confidentiality can attract negative media attention, potentially harming the organization’s public image and leading to loss of business.
- Loss of Partnerships: Organizations found in violation may lose contracts or partnerships with other healthcare providers, insurers, or government agencies, further limiting their ability to operate effectively.
Understanding the consequences of non-compliance emphasizes the importance of prioritizing data protection within healthcare organizations. Regular audits, employee education, and the implementation of security measures are essential to avoid costly violations and to ensure the safety and privacy of patient information.
Effective Strategies for Health Data Protection Education
Ensuring that healthcare professionals understand the importance of safeguarding sensitive patient information requires a strategic approach to education. Effective instruction not only covers legal obligations but also fosters a culture of security, where all team members recognize the value of protecting personal health data. A well-rounded education plan ensures that employees are prepared to handle information responsibly and comply with relevant laws, mitigating risks associated with data breaches or violations.
Successful education initiatives should be interactive, ongoing, and tailored to the specific needs of each organization. By employing a variety of learning strategies, healthcare providers can enhance understanding and ensure that staff members remain compliant with regulations over time.
1. Regular Workshops and Webinars
Hosting regular workshops and webinars is an excellent way to keep staff updated on the latest requirements and best practices. These sessions provide opportunities for employees to ask questions, share experiences, and engage in discussions about real-world scenarios. Offering these sessions virtually or in-person allows flexibility for busy healthcare teams.
- Interactive Discussions: Encourage open discussions where employees can talk about challenges they’ve faced in protecting sensitive data.
- Scenario-based Learning: Use real-life examples to highlight potential threats and teach proper responses in handling information securely.
2. Incorporating E-Learning Modules
Implementing e-learning modules allows employees to access educational materials at their own pace, making it easier for them to fit learning into their schedules. Online training can be structured with tests and quizzes to ensure retention and understanding of key concepts. E-learning provides a convenient method for organizations to reach a large number of employees at once, regardless of their location.
- On-demand Access: Employees can revisit training materials whenever needed, reinforcing important information over time.
- Tracking Progress: E-learning platforms allow organizations to track employee progress and completion rates, ensuring accountability.
3. Simulated Security Breach Exercises
Conducting simulated data breach exercises is an impactful way to test employee preparedness in responding to security threats. These drills help employees practice their knowledge of security protocols and identify areas for improvement. By creating realistic scenarios, teams can learn to act quickly and correctly when faced with a potential breach.
- Realistic Scenarios: Simulate different types of security threats, such as phishing attacks or unauthorized access, to prepare staff for a variety of situations.
- Post-exercise Analysis: After the simulation, provide feedback and discuss how responses could be improved, reinforcing the learning process.
By implementing these strategies, organizations can create a comprehensive and ongoing education program that ensures their staff is equipped to handle sensitive data securely, minimizing the risk of breaches or legal violations.
Benefits of Passing the Certification Test
Successfully completing certification assessments offers a range of advantages for professionals working in healthcare or any field requiring the management of sensitive data. Not only does it demonstrate a thorough understanding of relevant rules and guidelines, but it also ensures that individuals are well-equipped to safeguard critical information effectively. The knowledge gained from these assessments strengthens both personal competence and organizational security.
Achieving a passing score on these assessments provides individuals with confidence in their ability to adhere to the necessary protocols, while also reinforcing their commitment to maintaining high standards of confidentiality and compliance within their roles.
1. Enhanced Career Opportunities
Passing certification tests often opens doors to new career opportunities. Employers value candidates who have proven expertise in handling confidential information, as it directly impacts an organization’s ability to maintain regulatory compliance. These qualifications are highly sought after, leading to potential promotions or job offers in organizations that prioritize data security.
- Job Security: Certification ensures that employees are recognized as reliable and knowledgeable, boosting their value within the workplace.
- Career Advancement: Those who pass the assessments may be more likely to move into leadership or specialized roles with greater responsibilities.
2. Legal and Ethical Assurance
Having passed certification tests demonstrates a strong commitment to upholding ethical standards in managing sensitive information. It serves as evidence of an individual’s readiness to comply with legal regulations, reducing the likelihood of inadvertent violations. This not only protects the individual but also shields the organization from potential legal consequences or penalties.
- Risk Reduction: Certified professionals are less likely to make costly mistakes that could result in data breaches or legal issues.
- Trust Building: Passing certification tests builds trust with clients, patients, and partners, assuring them that their sensitive information is in safe hands.
In summary, passing these certification assessments not only brings personal growth and career benefits but also plays a key role in fostering a culture of compliance and responsibility within organizations. It strengthens both individual and organizational efforts in protecting valuable data and ensuring lawful operations.