In healthcare settings, ensuring patient safety while providing necessary treatments is a fundamental responsibility. The ability to properly administer care, understand the right methods, and avoid common mistakes is crucial for any professional. Mastery of these skills is essential for effective patient outcomes and reducing the risk of harm.
Knowledge and competence in handling various procedures are key aspects of this profession. Healthcare providers must be well-versed in appropriate techniques, the proper use of tools, and the correct dosages. These abilities can greatly impact the overall quality of care delivered.
As professionals prepare for assessments in this area, it’s important to focus on both the theoretical knowledge and the practical application of skills. By studying various scenarios, understanding common challenges, and reviewing essential guidelines, individuals can enhance their proficiency and readiness for any real-life situations.
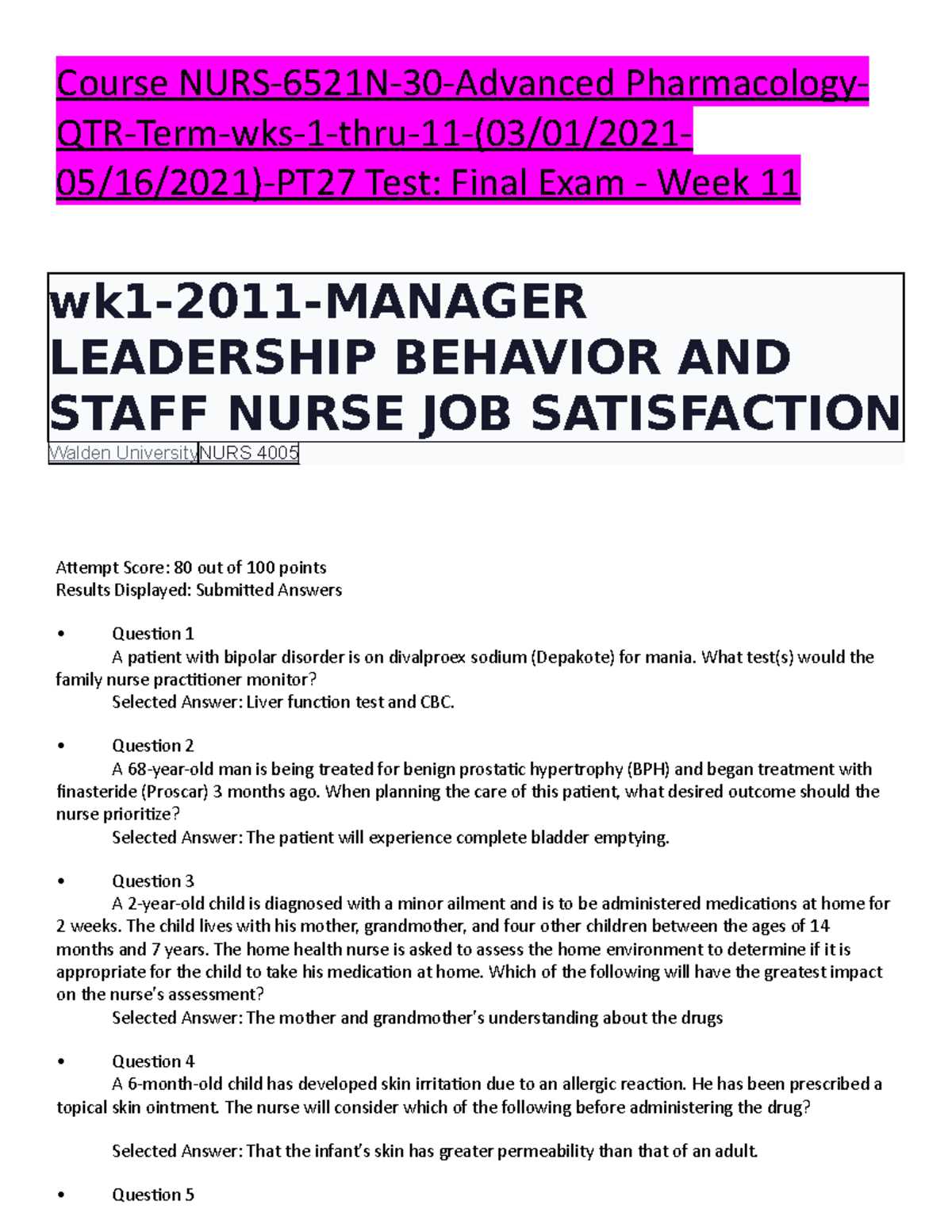
Medication Administration Knowledge and Assessment
Achieving proficiency in delivering proper healthcare requires not only a solid understanding of procedures but also the ability to apply that knowledge effectively in real-world scenarios. The process of evaluating one’s competence in this field includes mastering core principles and techniques essential for safe practices. This section aims to outline the key areas that are typically assessed during evaluation phases, focusing on the skills that are necessary to ensure the safety and well-being of patients.
Core Principles of Safe Healthcare Delivery
Effective healthcare involves understanding various methods for administering care, recognizing potential risks, and adhering to strict protocols to prevent errors. These principles are tested through both practical scenarios and theoretical assessments, which help gauge how well a professional can execute safe and accurate treatments. Key areas include:
| Key Area | Description |
|---|---|
| Proper Technique | Ensuring correct application of procedures to avoid complications. |
| Dosage Calculation | Accurately measuring and administering the right amount of substances. |
| Risk Awareness | Identifying and managing potential hazards that may affect patient outcomes. |
| Documentation | Maintaining accurate records to track treatments and outcomes. |
Preparation for Assessments in Healthcare Procedures
Preparation involves a thorough review of essential concepts and practical skills. Professionals must focus on the theoretical foundations as well as how to execute them under pressure. Mock scenarios and case studies are often used to simulate real-life situations, offering opportunities to practice responses and refine techniques. With diligent preparation, individuals can demonstrate their readiness to provide the highest level of care.
Key Concepts in Healthcare Delivery
To ensure safe and effective patient care, it’s essential to understand the fundamental principles that guide healthcare practices. Properly applying techniques, maintaining accurate dosages, and adhering to safety protocols are all critical elements that healthcare professionals must master. This section highlights the core concepts that form the foundation for delivering high-quality care and preventing errors in patient treatment.
Accuracy in Dosage and Measurement
One of the most crucial aspects of healthcare procedures is ensuring the precise calculation and delivery of substances. Even small discrepancies in measurement can lead to serious consequences. Healthcare providers must be well-versed in using proper tools and techniques to calculate dosages accurately, taking into account factors like patient age, weight, and health conditions.
Safe Techniques and Protocols
Following established guidelines and safety protocols is vital to prevent complications. Each procedure has its own set of recommended steps to ensure that healthcare is delivered correctly. These protocols cover everything from preparation to disposal, ensuring that the risk of contamination or error is minimized. Professionals must be diligent in adhering to these methods to protect both the patient and themselves.
Understanding Dosage Calculations for Nurses

Accurately calculating dosages is a critical skill in healthcare, ensuring that patients receive the correct amount of treatment. A small error in dosage can have significant consequences, making it essential for nurses to have a thorough understanding of how to properly measure and administer substances. This section explores the key principles behind dosage calculations, providing guidance on how to avoid common mistakes and ensure patient safety.
Basic Principles of Dosage Calculations
To accurately determine the right dosage, healthcare professionals must first understand the basic formulas and conversion factors involved in the process. This includes knowing how to convert between different units of measurement, such as milligrams to grams or milliliters to liters. Nurses must also be familiar with different dosage forms (e.g., tablets, liquids) and how to adjust calculations based on the patient’s individual needs, such as age, weight, and condition.
Common Challenges in Dosage Calculations
One of the most frequent challenges nurses face is ensuring that they interpret the prescription correctly and apply the correct formula. Misreading labels, not accounting for dilution factors, or miscalculating the quantity can lead to serious errors. Regular practice, attention to detail, and verification of calculations are essential strategies for overcoming these challenges and ensuring accurate results.
Common Healthcare Errors to Avoid

In healthcare, even small mistakes can have serious consequences. Understanding the most common errors and knowing how to prevent them is essential for ensuring patient safety. This section outlines frequent mistakes that professionals encounter and provides strategies for avoiding these pitfalls, improving the overall quality of care provided to patients.
Incorrect Dosage Calculations
One of the most frequent errors in healthcare is the incorrect calculation of treatment amounts. Misjudging the proper quantity can lead to underdosing or overdosing, both of which pose significant risks. Professionals must double-check calculations and ensure the appropriate units are used. Regular practice and familiarity with dosage formulas can help mitigate this issue.
Failure to Check for Allergies or Interactions
Another common mistake is neglecting to verify a patient’s allergies or potential drug interactions before delivering treatment. Failing to do so can result in adverse reactions or dangerous side effects. It is critical to review patient history and consult updated medical records to prevent harmful interactions. Developing a systematic approach for reviewing this information is key to reducing errors.
Importance of Proper Drug Storage Practices
Storing healthcare substances correctly is vital to maintaining their effectiveness and ensuring patient safety. Improper storage can lead to contamination, degradation, or reduced potency, all of which can negatively affect treatment outcomes. This section emphasizes the importance of following proper storage guidelines to preserve the quality and safety of healthcare supplies.
Temperature, humidity, and light exposure are key factors that can impact the integrity of substances. It is crucial to store items in conditions recommended by manufacturers or regulatory standards, whether in a cool, dry place or a refrigerated environment. Additionally, keeping products in their original packaging helps prevent contamination and ensures they are used within their shelf life.
Adhering to proper storage protocols also helps prevent errors, such as mixing up products or administering expired substances. Maintaining organized storage systems and regularly auditing stock ensures that healthcare providers have access to safe and effective treatments when needed.
Guidelines for Safe Healthcare Delivery
Ensuring the safety of patients during treatment requires strict adherence to best practices. Following well-established guidelines is crucial to minimizing the risk of errors and safeguarding patient well-being. This section outlines key recommendations for delivering care safely and effectively, focusing on the most important steps to prevent mistakes and enhance outcomes.
| Guideline | Description |
|---|---|
| Verify Patient Information | Always confirm the patient’s identity, allergies, and relevant medical history before providing any treatment. |
| Check for Interactions | Ensure that prescribed treatments do not interact negatively with any other substances the patient is currently taking. |
| Follow Standard Procedures | Adhere to established procedures for delivering care to prevent errors and ensure consistency in practice. |
| Double-Check Dosages | Always verify the correct dosage and measurement to avoid under or over administration. |
| Maintain Proper Documentation | Accurately record all treatments and observations to ensure clarity and continuity of care. |
By incorporating these guidelines into everyday practice, healthcare professionals can significantly reduce the chances of mistakes and provide better care to their patients. Following these protocols ensures that both the safety and effectiveness of treatments are prioritized at every step.
Preparation Tips for Healthcare Competency Assessments
Preparing for assessments in healthcare requires a focused approach, balancing both theoretical knowledge and practical skills. The key to success lies in understanding core concepts, practicing hands-on techniques, and honing the ability to apply knowledge in real-life situations. This section offers valuable strategies for those looking to excel in competency evaluations and enhance their readiness for professional responsibilities.
Study Key Concepts and Procedures
Start by reviewing essential principles and common procedures that are frequently assessed. Understanding the fundamental concepts behind patient care and treatment methods is crucial. Take time to study medical terminology, dosage calculations, and safety protocols, as these are often central to assessments. Create a study plan that allows you to break down complex topics into manageable sections for more efficient learning.
Practice Practical Skills Regularly
Equally important as theoretical knowledge is the ability to perform tasks competently and confidently. Regular practice of practical skills, such as dosage calculations, preparing and measuring substances, and following safety protocols, is key. Consider utilizing mock scenarios or practicing with a peer or mentor to simulate real-life situations and improve your performance under pressure.
Consistency and preparation are the foundations of success in healthcare assessments. By focusing on both knowledge and hands-on skills, individuals can increase their chances of achieving competency and providing safe, effective care.
Legal and Ethical Aspects of Healthcare Use
In healthcare, understanding the legal and ethical principles that govern the use of substances is essential for maintaining patient trust and ensuring safety. Professionals must adhere to laws, regulations, and ethical standards that protect both the patient and the healthcare provider. This section delves into the fundamental legal and ethical considerations that healthcare workers must be aware of when managing patient treatments.
Legal Responsibilities
Healthcare professionals are bound by laws that dictate how treatments should be provided. These laws vary by country and region but are typically designed to ensure patient safety and establish clear standards for practice. Key legal responsibilities include:
- Obtaining informed consent before providing treatment
- Adhering to regulations regarding prescribed dosages and substances
- Documenting treatments accurately and thoroughly
- Respecting patient confidentiality and privacy
Ethical Considerations

Alongside legal obligations, healthcare professionals must also consider the ethical implications of their actions. Ethical standards guide behavior and decision-making, ensuring that patient welfare is prioritized. Important ethical aspects to keep in mind include:
- Respecting patient autonomy and decision-making
- Ensuring fairness and equality in care, regardless of background or status
- Balancing patient needs with professional integrity and responsibility
- Avoiding conflicts of interest that could compromise patient care
By following both legal and ethical guidelines, healthcare workers contribute to a safer, more transparent healthcare environment that respects patients’ rights and maintains professional accountability.
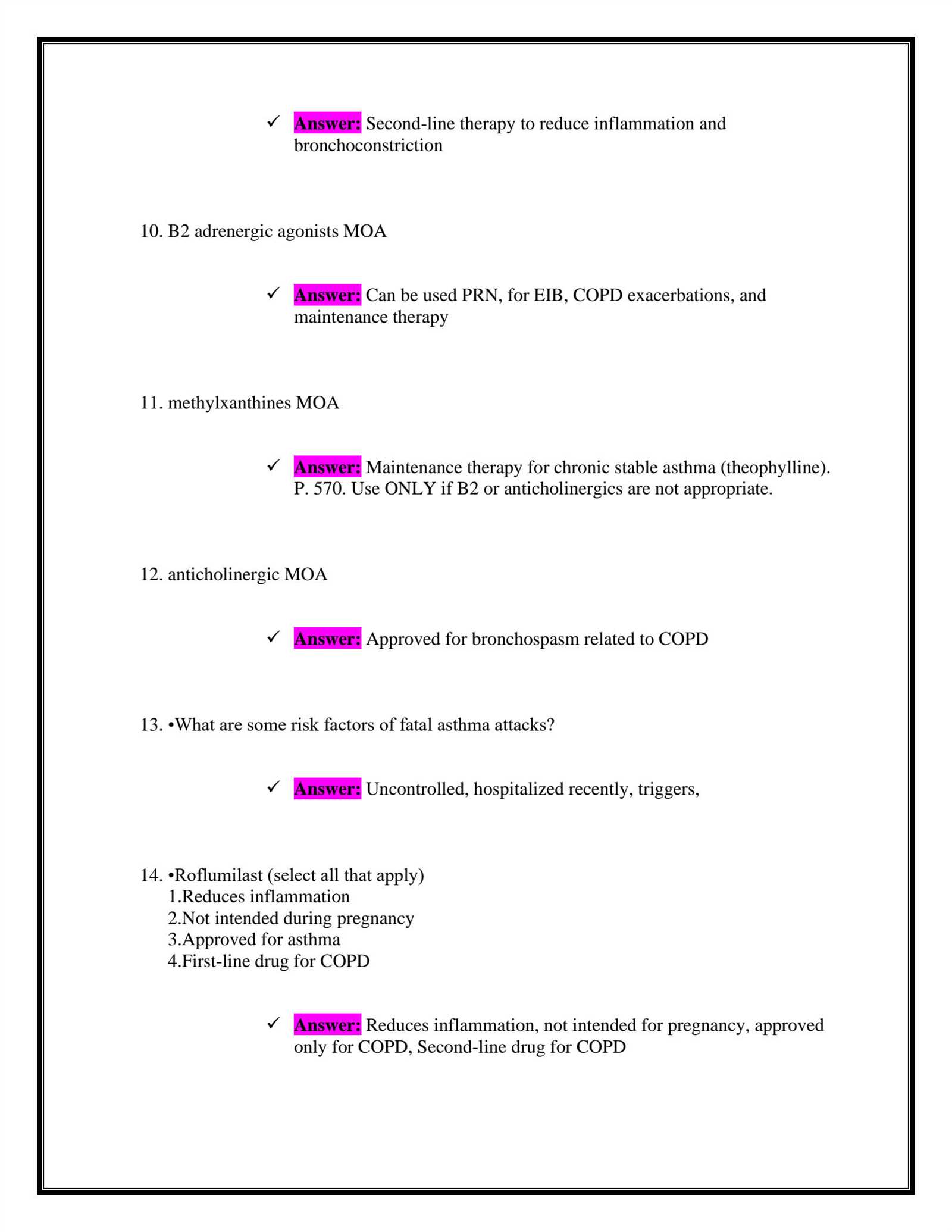
Healthcare Delivery Routes and Techniques
In healthcare, there are various methods for delivering treatments to patients, each chosen based on the specific needs of the patient and the type of care required. These methods, or routes, vary in terms of their effectiveness, speed of action, and potential for side effects. This section explores the different delivery routes and techniques used in healthcare practice, providing insight into their advantages and limitations.
Common Routes for Treatment Delivery
The route through which a substance is delivered plays a significant role in how quickly and effectively it reaches its intended target. Some common routes include:
- Oral: Substances are ingested through the mouth and absorbed through the digestive system. This is one of the most common and convenient routes but may be slower in terms of onset.
- Topical: Applied directly to the skin or mucous membranes, this route is typically used for localized treatments, such as ointments or creams.
- Intravenous (IV): Administered directly into the bloodstream through a vein, this method provides the fastest onset of action and is often used in emergency situations.
- Intramuscular (IM): Injections are given directly into the muscle, providing faster absorption than oral administration but slower than IV.
- Subcutaneous: Administered just under the skin, this route is commonly used for vaccines or certain long-term treatments.
Techniques for Safe and Effective Delivery
Regardless of the route chosen, using the correct technique is essential to ensure the treatment is effective and safe. Some best practices include:
- Proper Hygiene: Always wash hands and use clean equipment to prevent infection or contamination.
- Correct Dosage: Ensure that the correct amount is administered according to the patient’s needs and prescribed guidelines.
- Accurate Timing: Administer treatments at the appropriate intervals to maintain their effectiveness.
- Patient Monitoring: Observe patients for adverse reactions and ensure they are responding positively to the treatment.
By following these methods and techniques, healthcare professionals can ensure they are providing the safest and most effective care to their patients.
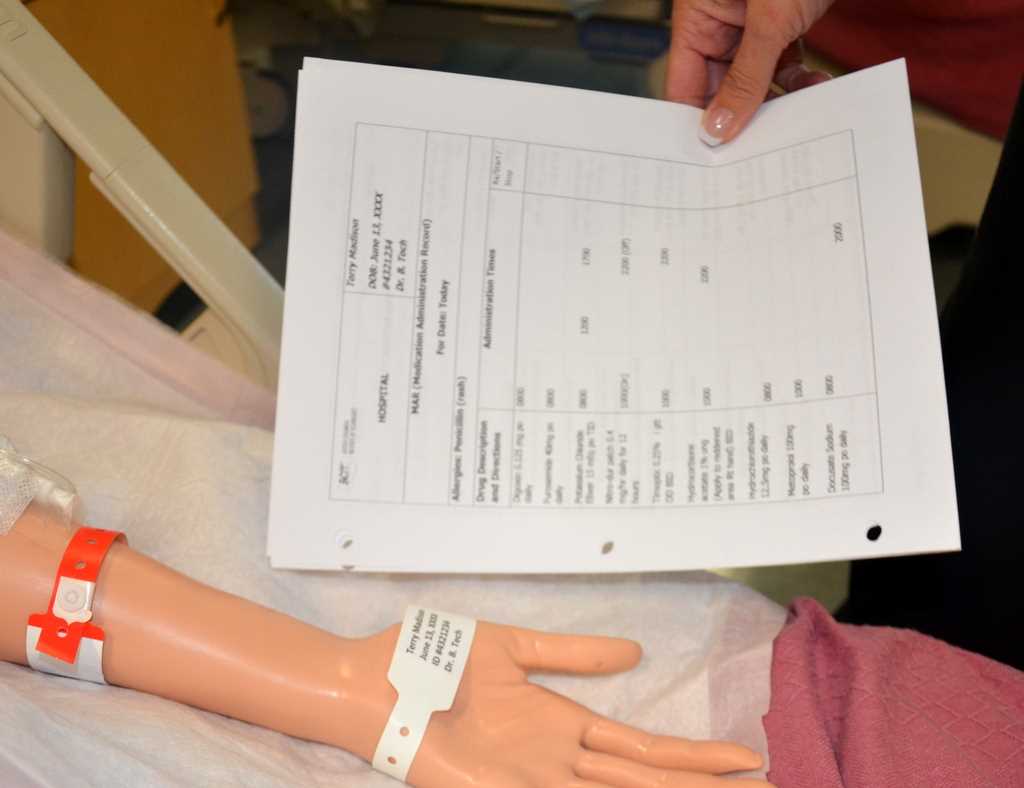
Documentation Best Practices for Nurses
Accurate and thorough documentation is an essential part of nursing practice. It ensures that patient care is well-coordinated, that legal requirements are met, and that healthcare providers are held accountable for the care they provide. In this section, we will explore best practices for documentation, focusing on maintaining clear, concise, and accurate records in order to provide optimal patient care.
Key Principles of Effective Documentation
Proper documentation is based on several key principles that help ensure the accuracy and reliability of patient records. These include:
- Clarity: Always write in clear and simple language to avoid any misunderstandings. Avoid jargon or abbreviations that may not be universally understood.
- Accuracy: Ensure that all information recorded is factual and free from errors. Cross-check information when necessary to confirm its validity.
- Timeliness: Document care as soon as possible after it is provided to ensure that the information is fresh and accurate.
- Completeness: Provide a comprehensive account of the care provided, including assessments, actions taken, and the patient’s response to treatment.
Best Practices for Specific Documentation Areas
In nursing, there are specific areas where documentation plays a critical role in patient safety and continuity of care. Below are some best practices for common documentation tasks:
- Patient Assessments: Always include detailed observations of the patient’s condition, including any changes in symptoms, vital signs, and physical findings.
- Treatment Plans: Document the prescribed interventions, including any medications, therapies, or other procedures, and ensure these are followed precisely as ordered.
- Patient Responses: Record the patient’s reactions to treatments, noting any adverse effects or complications. This information is vital for ongoing care planning.
- Communication with Other Healthcare Providers: Ensure that communication with other team members, such as physicians or specialists, is documented, especially when new orders or changes in care plans are made.
By adhering to these best practices, nurses can ensure that their documentation is clear, accurate, and useful in enhancing patient care and promoting effective communication within the healthcare team.
Role of Pharmacology in Medication Safety

Pharmacology plays a critical role in ensuring the safety of treatments prescribed and administered to patients. It involves the study of how substances interact with the body, how they are metabolized, and their potential effects on various systems. A clear understanding of pharmacology is essential for healthcare providers to minimize the risks associated with treatments and enhance patient safety.
By gaining knowledge of how different drugs work, their side effects, and their interactions with other substances, healthcare professionals can make informed decisions when prescribing or administering treatments. This helps avoid common risks such as overdosing, adverse reactions, and harmful drug interactions.
Additionally, pharmacology aids in proper dosage calculation, correct delivery methods, and monitoring patient responses. Healthcare providers must continually update their knowledge in this field to stay informed about new drugs, evolving treatment protocols, and emerging safety guidelines. In doing so, they ensure the best outcomes for patients while minimizing the potential for harm.
Understanding Side Effects and Drug Interactions
When substances are used to treat medical conditions, they can produce effects beyond the intended therapeutic outcomes. These unintended effects, known as side effects, may range from mild discomfort to severe health risks. Additionally, when different substances are taken together, they can interact in ways that modify their individual effects, sometimes in unpredictable ways. Understanding these side effects and interactions is essential for ensuring safety and effectiveness during treatment.
Healthcare professionals must be aware of potential side effects that may arise from various treatments and the interactions between different therapeutic substances. By doing so, they can take necessary precautions, adjust dosages, and prevent any adverse reactions that may compromise patient health.
Common Side Effects
Some side effects are common and predictable, while others are rare and can be difficult to anticipate. Recognizing these effects can help healthcare providers take prompt action. Below are some frequent side effects and their potential causes:
| Side Effect | Possible Cause | Recommended Action |
|---|---|---|
| Fatigue | Interaction with sedative substances | Monitor patient activity, adjust dosages as needed |
| Nausea | Gastrointestinal irritation | Administer with food, consider alternative options |
| Dizziness | Drop in blood pressure | Ensure proper hydration, monitor blood pressure regularly |
Drug Interactions and Risks
When different substances are taken together, they may either enhance or inhibit each other’s effects. Some combinations may lead to dangerous reactions, increasing the risk of side effects or reducing the efficacy of treatment. Healthcare providers need to assess all substances a patient is taking to prevent harmful interactions.
| Type of Interaction | Example | Potential Risk |
|---|---|---|
| Enhancement | Combining blood thinners with certain pain relievers | Increased risk of bleeding |
| Inhibition | Mixing certain antibiotics with antacids | Reduced effectiveness of the antibiotic |
| Synergy | Combining medications for pain relief and anti-inflammatory effects | Increased risk of stomach ulcers or bleeding |
Being aware of side effects and interactions is crucial for managing treatment safely. Both healthcare providers and patients must work together to monitor and adjust therapy to ensure that the benefits outweigh the risks. Regular reviews of treatment plans can help avoid complications and ensure the best possible outcomes.
Reviewing the Five Rights of Medication Administration
In healthcare, ensuring the safe delivery of treatments is critical. One of the fundamental approaches to minimizing errors and safeguarding patient well-being is by adhering to a set of guiding principles. These principles help healthcare professionals provide the correct therapy in the right manner, ensuring optimal outcomes. The five key rights are an essential framework for reducing the risk of mistakes and improving patient care.
Understanding the Core Principles
The five key principles emphasize the importance of verifying key aspects before any substance is given to a patient. Each “right” focuses on a specific area that must be checked to prevent any errors that could compromise patient safety. These principles serve as a checklist that healthcare workers must follow, ensuring that every aspect of the process is correct, from identifying the right patient to monitoring the results of the treatment.
- Right Patient: Always confirm the identity of the person receiving treatment. This can be done by using two forms of identification, such as a name and birthdate.
- Right Treatment: Verify that the prescribed therapy is the correct one for the patient’s condition and that no contraindications exist.
- Right Dosage: Double-check the correct amount of the therapy, considering factors like the patient’s weight, age, and condition.
- Right Time: Administer the treatment at the prescribed time, ensuring that intervals between doses are properly maintained.
- Right Route: Confirm the appropriate method of delivery, whether it be oral, intravenous, topical, or another route.
Implementing the Five Rights in Practice
When these principles are followed closely, the risk of harm to patients decreases significantly. Healthcare professionals must be diligent in reviewing the five rights, particularly in busy environments where distractions are common. Regular training, clear communication, and thoughtful double-checking are essential components of putting these principles into action. Through adherence to these rights, the healthcare team ensures that patients receive safe, effective care tailored to their needs.
Training on Emergency Medication Responses
In healthcare settings, being prepared for sudden and critical situations is essential to providing the best possible care. One of the most important skills is understanding how to respond quickly and effectively with the proper therapies during emergencies. This involves knowing the correct interventions, dosages, and techniques for immediate patient care. Effective response requires not only knowledge of the necessary substances but also the ability to act swiftly and accurately under pressure.
Key Principles of Emergency Responses
When facing urgent health situations, healthcare professionals must act quickly while ensuring the right steps are followed to stabilize the patient. These responses can include administering life-saving treatments, controlling symptoms, or preparing the patient for further medical procedures. Clear procedures and protocols help prevent confusion during high-stress moments. In addition to understanding the necessary steps, healthcare workers must remain calm and focused, keeping a clear head while making quick decisions.
- Assessment: Quickly evaluate the patient’s condition, noting any signs or symptoms of distress. Proper assessment is crucial for choosing the right response.
- Proper Dosage: Ensure the correct dosage is given based on the patient’s age, weight, and condition. Over- or under-dosing can lead to serious complications.
- Timely Action: Act promptly, as the first few minutes of an emergency can significantly impact the patient’s chances of recovery.
- Documentation: After the response, document all actions taken, substances used, and patient reactions to ensure accurate records for future care.
Simulations and Practice Drills
To ensure readiness, healthcare workers should participate in regular drills and simulations that mimic real-life emergencies. These exercises help to reinforce knowledge, sharpen decision-making skills, and improve coordination among team members. Practicing different scenarios builds confidence, allowing professionals to respond swiftly when an actual emergency occurs. Training must cover a range of potential situations, from common to rare emergencies, ensuring that the team is prepared for any situation that arises.
Impact of Patient Allergies on Medication Administration
Allergies play a crucial role in determining the appropriate therapeutic interventions for a patient. When a patient has a known allergy to a particular substance, it is vital for healthcare professionals to be aware of the potential risks involved with using certain treatments. Failing to consider allergies can lead to severe reactions, which may compromise patient safety. Therefore, understanding the relationship between allergies and the substances used in medical care is essential for providing safe and effective treatment.
Types of Allergic Reactions
Allergic reactions can vary from mild to severe, and understanding their symptoms helps healthcare providers prevent potential harm. Common types of allergic reactions include:
- Skin Reactions: These can include rashes, itching, and swelling, which may occur when a patient is exposed to an allergen.
- Respiratory Reactions: Symptoms such as wheezing, difficulty breathing, and tightness in the chest may occur, particularly with certain substances like antibiotics or anesthetics.
- Anaphylaxis: A life-threatening reaction that can cause a sudden drop in blood pressure, swelling of the throat, and difficulty breathing. This requires immediate intervention.
Considerations for Safe Practice
Healthcare professionals must take extra precautions when treating patients with known allergies. Several factors should be considered to reduce the risk of adverse events:
- Complete Allergy History: Always gather a detailed allergy history from the patient, including any previous reactions to substances used in healthcare settings.
- Cross-Check Medication Ingredients: Verify the composition of each substance before administering it, ensuring that no known allergens are present.
- Labeling and Documentation: Clearly label patient charts with known allergens and update records regularly to ensure that no allergen exposure occurs during treatment.
- Alternative Treatments: In cases where an allergen cannot be avoided, consult with colleagues or specialists to explore alternative therapies.
By considering patient allergies and adjusting treatments accordingly, healthcare providers can significantly reduce the risk of allergic reactions and ensure patient safety throughout their care.
How to Handle Medication Refusals from Patients

Patient refusal of treatment is a common challenge that healthcare providers face. When patients choose not to take prescribed treatments or follow recommended care plans, it can create barriers to effective healing and recovery. It is crucial to understand the underlying reasons for refusal and address them in a professional and empathetic manner, while respecting the patient’s autonomy and right to make informed decisions about their care.
Common Reasons for Treatment Refusals
Patients may refuse treatment for a variety of reasons. Some of the most common reasons include:
- Fear of Side Effects: Patients may have concerns about the potential negative effects of a prescribed treatment, whether real or perceived.
- Misunderstanding or Lack of Information: Some patients may refuse care simply because they do not fully understand the purpose of the treatment or how it will benefit them.
- Previous Negative Experiences: Past experiences with treatments that did not work or caused harm can lead to hesitance in accepting similar therapies.
- Cultural or Religious Beliefs: Certain beliefs or practices may conflict with the use of specific treatments, leading to refusal.
- Financial Concerns: The cost of treatments or medications may be a barrier for some patients, especially those without adequate insurance coverage.
Strategies for Managing Refusals
When faced with a refusal, healthcare providers should take thoughtful steps to address the situation and work collaboratively with the patient. Some effective strategies include:
- Open Communication: Take time to discuss the patient’s concerns, listen actively, and provide clear, non-technical explanations of the benefits and risks of the treatment.
- Education: Provide written or visual materials that help explain the treatment process, potential outcomes, and the importance of adhering to the prescribed plan.
- Offer Alternatives: When possible, suggest alternative treatments or options that align better with the patient’s preferences or needs.
- Respect Autonomy: While it’s important to offer guidance, always respect the patient’s right to refuse treatment and ensure they are making an informed decision.
- Documentation: Carefully document the refusal, including the reasons for it, any discussions held, and the steps taken to address the concerns. This can be important for legal and clinical purposes.
Handling patient refusals with care and respect helps build trust and can lead to more cooperative relationships, ultimately resulting in better healthcare outcomes.